* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Slide 1
Survey
Document related concepts
Transcript
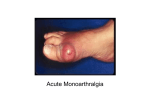
My knee hurts MSU Emergency Medicine Lansing, MI Dr. Patricia Manhire What are the Indications for Arthrocentesis? Indications for Arthrocentesis Crystal-induced arthropathy Hemarthrosis Symptomatic relief of a large effusion Unexplained joint effusion Unexplained monarthritis Suspect interarticular infection What are the Contraindications to Joint Needle Aspiration? Contraindications to Joint Needle Aspiration Absolute Overlying infection in the soft tissues* abscess & cellulitis Severe coagulopathy Severe overlying dermatitis Relative contraindication Bacteremia Hemophilia On Warfarin Uncooperative patient *** Often Acutely arthritic joint symptoms may mimic a soft tissue infection Review of Procedure Knee Arthrocentesis Ultrasound Ultrasound-assisted arthrocentesis can be used as an adjunct to assist in localization and aspiration of joint fluid. Using a linear 5-10 MHz probe Anterior transverse scan A (top)= prior to aspiration B (bottom) = following aspiration > = tip of the needle, f = femur. Filippucci E, Iagnocco A, Meenagh G, Riente L, Delle Sedie A, Valesini G, Grassi W. Position & Prep Knee extended or slightly bent Can use medial or lateral approach Controversial: Studies show bent has a lower yield of fluid in small effusions but is more comfortable. Suggest lateral with smaller effusions Prep skin povidone-iodine or Choroprep Identify Landmark Lateral Approach Insert needle 1 cm above and 1 cm lateral to the superior lateral aspect of the patella. The needle is tilted beneath the patella at a 45-degree angle. Aspiration Inserted needle through stretched skin. Stretching the skin can reduce discomfort Some administer lidocaine into the skin. The needle is directed at a 45-degree angle distally and 45 degrees into the knee, tilted below the patella Compression applied over the joint space or "milking" of the bursae, on the patellar side opposite the needle insertion site, may facilitate aspiration. Roberts & Hedges. Clinical Procedures in Emergency Med. 4th Ed Saunders 2004 You now have the Fluid Sample. What labs do you Order? Examination of Synovial Fluid Normal Noninflammatory Inflammatory Septic Clarity Transparent Transparent Cloudy Cloudy Color Clear Yellow Yellow Yellow WBC/L <200 <200–2000 200–50,000 >50,000 PMN % <25 <25 >50 >50 Culture Negative Negative >50% positive Crystals None None Multiple or none None Associated conditions Osteoarthritis, trauma, Gout, pseudogout, spondyloarthropathies, rheumatic fever Negative RA, Lyme disease, SLE RA = rheumatoid arthritis; SLE = systemic lupus erythematosus Nongonococcal or gonococcal septic arthritis What is your interpretation of the fluid? •Normal •Noninflammatory •Inflammatory •Septic So, you have determined your patient has Inflammatory Arthritis What information would help you decide which Inflammatory Arthritis your pt has: Gout? Pseudogout? Spondyloarthropathies? RA? Lyme disease? SLE? Number of joints involved Crystals or no crystals Classification of Arthritis by Number of Affected Joints Number of Joints Differential Considerations Monoarthritis Trauma-induced arthritis Infection/septic arthritis Crystal-induced (gout, pseudogout) Osteoarthritis (acute) Lyme disease Avascular necrosis Tumor 2–3 = Oligoarthritis Lyme disease Reiter syndrome Ankylosing spondylitis Gonococcal arthritis Rheumatic fever >3 = Polyarthritis Rheumatoid arthritis Systemic lupus erythematosus Viral arthritis Osteoarthritis EMERGENCY MEDICINE: A Comprehensive Study Guide, 6th ed, The McGraw-Hill Companies, Inc. Lyme Disease The arthritic manifestations occur in the weeks, months, or years following the primary, stage I infection Typically, a monarticular or migratory oligoarticular Large joints are most often affected Arthrocentesis inflammatory synovial fluid, usually with negative cultures History of endemic area exposure history of tick bite or erythema chronicum migrans (ECM) rash is helpful but often absent Show characteristic stage II and stage III findings—such as fatigue, neurologic abnormalities, and/or cardiac conduction disturbances May require laboratory confirmation Treatment is administered for 3 to 4 weeks. Rx: doxycycline, penicillin G, amoxicillin, or ceftriaxone. Rheumatoid Arthritis Symmetric, polyarticular involvement. Sparing of the distal interphalangeal (DIP) joints. Stiffness of the joints after inactivity (morning stiffness). Multisystem involvement is characteristic depression, fatigue, and generalized myalgias. pericarditis, myocarditis, pleural effusion, pneumonitis, Arthrocentesis of synovial fluid - inflammatory profile. Treatment: Salicylates or other NSAIDs Immobilization providing added relief from joint movement pain. Corticosteroids may be utilized for brief periods Long-term therapy using agents such as antimalarials, gold, and methotrexate. Ankylosing Spondylitis Seronegative spondyloarthropathies Ankylosing Spondylitis Similar to RA morning stiffness and multisystem involvement with constitutional symptoms such as malaise, weakness, and fatigue. Usually younger than age 40 Treatment consists of pain control with shortterm and long-term management with NSAIDs. Crystal-Induced Synovitis: Gout & Pseudogout Gout & Pseudogout Middle-aged and elderly adults. Both often follows trauma, surgery, a significant illness, or change in medications affecting uric acid levels. Pseudogout Positive birefingence crystals: Calcium pyrophosphate -rhomboid shape Acute treatment: same as Gout. Gout Negative birefringence: Uric acid crystals -- needle-shaped and blue 30 % have normal uric acid levels during an acute gout attack Treatment: nonsteroidal anti-inflammatory drugs (NSAIDs) or Colchicine or indomethacin Once the symptoms of an acute resolved, elimination of gout-inducing agents (diuretics, aspirin, or cyclosporine) and treatment with allopurinol or probenecid Your Diagnosis? Acute Rheumatoid Arthritis What is your Treatment Plan