* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Tuberculosis and Leprosy - Osteopathic Medical School
Survey
Document related concepts
Transcript
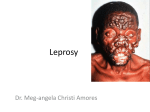
Mycobacteria: Tuberculosis and Leprosy Ben Adams DO 3-21-06 Tuberculosis Epidemiology • Estimated 1.7 billion infected persons – 1/3 of world’s population – 10 million people in US • 12 million new cases per year w/ 3 million deaths • 4 million co-infected with HIV – ¾ live in sub-Saharan Africa • Incidence tied to poverty, unemployment, homelessness, AIDS and drug resistance • Multi-drug resistant disease (MDRTB) major problem http://www.med.sc.edu:85/fox/tuber-map3.jpg Tuberculosis Etiology • Mycobacterium tuberculosis (Tubercle bacillus, MTB), M. bovis, M. africanum and BCG • Immune response contains infection in majority – 5-10% of immunocompetent develop clinical disease • Rarely eradicated due to resistance to macrophage destruction, dormancy within granulomas • Dormant bacilli resistant to antimycobacterials • Immunosuppression often leads to clinical sx Tuberculosis Etiology • MTB Surface Coat – Mycolic acid – Highly inflammatory – Stimulates Macrophages and T lymphs Tuberculosis Symptoms • Pulmonary: – SOB – Sputum production • Systemic: – – – – – Fatigue Malaise Fever (in ddx for FUO) Lethargy Weight loss Tuberculosis Symptoms • Disseminated Disease: – Miliary pattern on CXR – Pancytopenia – Other Sites: • Bones, GI, brain, meninges • Almost any organ • Asymptomatic in large number of persons – 90% The Tuberculin Reaction • The Koch Phenomenon • Most likely due to a Delayed T-cell Hypersensitivy (DTH) rxn – Mediated by sensitized T lymphs when injected into a nonsensitized individual • In sensitized individual rxn varies depending on test dose and route of administration • Local intradermal inject. leads to the local TB rxn • Reaches max intensity after 48 hrs • Consists of a sharply circumscribed area of erythema and induration The Tuberculin Reaction • Purified Protein Derivative (PPD) is currently used • Read 48-72 hours after intradermal injection • Becomes positive between 2 and 10 weeks and remains positive for many years http://www.info.gov.hk/dh/diseases/CD/photoweb/Tuberculosis-2.jpg PPD evaluation • 0.1ml of PPD (5U) placed intradermally to form a wheal • Measure true induration (not erythema) 48-72 hrs – >5mm Induration is positive in following hosts: • patients with recent close contact with a person with active TB • patients with fibrotic lesions on chest radiograph • patients with known or suspected HIV infection – >10mm Induration is positive in: • Patients with high risk comorbid conditions • Persons from endemic areas • Residents of long-term (chronic) care facilities – >15mm required for positivity in normal hosts TB Histopathology • Tubercle is the hallmark – Accumulation of epithelioid histiocytes with Langerhans giant cells – Caseation necrosis in the center – Rim of lymphs & monos • The tuberculioid granuloma is characteristic but NOT pathognomonic BCG Vaccination • Bacillus Calmette-Guerin (BCG) is a living attenuated bovine tubercle bacillus to enhance immunity to tuberculosis • Only given to TB (-) persons • Reduces childhood TB up to 75% • Normal course of BCG vaccination – 2 wks: infiltrated papule develops – 6-12 wks: size of 10mm, ulcerates, and then slowly heals leaving a scar Rare BCG Reaction Primary Inoculation TB • 2-4 wks after inoculation painless brown-red ulcer with hemorrhagic base • 3-8 wks regional lymphadenopathy - painless • Face, hands, and legs • Histopathology – Typical tubercles • Langerhan’s cells w/ epithelioid cells surrounded by monocytes Primary Inoculation TB • Course: – W/o tx may last up to 12 mo – Lesions heal by scaring • Primary TB complex usually yields immunity but reactivation my occur Tuberculosis Verrucosa Cutis • Exogenous reinfection of MTB in a person previously sensitized • Minor wound often site of entry – many cases in pathologists/ postmortem attendants hence the expression “prosector’s warts” • PPD highly (+) http://dermis.net/doia/image.asp?zugr=d&lang=e&cd=21&nr=99&diagnr=17020 Tuberculosis Verrucosa Cutis • Usually a single slow-growing plaque or nodule m/c on hands – Small papule that becomes hyperkeratotic – Peripheral expansion w/ wo central clearing • Clefts and fissures discharging pus extend into the underlying base which is brownish-red to purplish Scrofuloderma • TB involvement of the skin by direct extension • Usually underlying TB lymphadenitis – Cervial Lymph nodes MC • Develops as firm subcutaneous bluish-red nodules – Break down and perforate leaving undermined ulcers and discharging sinuses – Bilateral http://www.indianpediatrics.net/jan2002/images/7.jpg Scrofuloderma • Histopathology: – Massive necrosis and abscess formation in the center – The periphery of the abscess or the margins of the sinuses contain tuberculoid granulomas and true tubercles • Acid-fast bacilli – MTB can be found Tuberculosis Orificialis • TB of mucous membranes and skin surrounding orifices – • Seen in pts with TB of internal organs – • Orificial tuberculosis. A nonhealing ulcer at the tip of the tongue GI Tract or Lungs Mouth most commonly affected site – • Usually by autoinoculation Tongue and palate • Prognosis poor – advanced internal disease • Presents as painful yellow or red nodule that ulcerates to form punched-out ulcer Tuberculosis Orificialis • Histopath: – Massive nonspecific inflammatory infiltrate and necrosis – Tubercles with caseation may be found deep in the dermis – Numerous bacilli Lupus Vulgaris • Cutaneous TB from hematogenous spread – Chronic and progressive – 50% have TB elsewhere • Single plaque of grouped red-brown papules that blanch with diascopic pressure – “Apple-jelly” nodules = pale brown/yellow – Spreads peripherally – Risk of BCC/SCC with mets • 90% occur head/neck http://dermatlas.med.jhmi.edu/derm/result.cfm?Diagnosis=-901045419 Lupus Vulgaris • Histopath – Hallmark: Classic Tubercles Metastatic Tuberculous Abscess • Tuberculous Gumma – Hematogenous dissemination from primary focus during a period of lowered resistance leading to distant abscess/ulcer • • • • • SubQ abcesses Nontender Fluctuant Singly or as multiples on the trunk, ext, or head Usually occurs in undernourished children or the immunodeficient or immuosuppressed Metastatic Tuberculous Abscess Metastatic Tuberculous Abscess • Histo: – Similar to scrofuloderma – Massive necrosis and abcess formation – Acid fast stains = copious amounts of myocbacteria Miliary TB (Miliaris Disseminata) • Hematogenous dissemination of MTB • Infants / young children • Focus of infection typically meningeal/pulmonary • May follow infections such as measles and HIV • Presentation: – Minute erythematous macules or papules and purpuric lesions – Sometimes umbilicated vesicles or central necrosis and crust develop in severely ill patients Miliary TB (Miliaris Disseminata) • Histopath: – Initially: • Necrosis and nonspecific inflam infiltrates and abcesses • Occasionally signs of vasculitis • MTB are present in and around vessels – Later stages (if the pt. develops immunity): • Lymphocytic cuffing of vessels and even tubercles Miliary TB of the Liver Multinucleated Giant Cell Tuberculids • Cutaneous immunologic rxn to TB elsewhere • By definition stains negative • Most likely the result of hematogenous dissemination in pts with high degree of immunity – With PCR, mycobacterial DNA demonstrated in both papulonecrotic tuberculid and erythema induratum of Bazin • All demonstrate rapid response to antiTB tx • Strongly positive PPD • Most exhibit tuberculosis features histologically Tuberculids • Lichen Scrofulosorum – Rare eruption of asymptomatic, minute, flat-topped yellow to pink follicular or parafollicular papules – May have a minute horny spine or fine scales – Occurs m/c on trunk of children and adolescents with TB in lymph nodes/bone – PPD (+) – Persist for months but spontaneous involution ensues – AntiTB tx results in resolution w/in weeks Tuberculids • Lichen Scrofulosorum • Histopath: – Superficial noncaseating tuberculoid granulomas develop around hair follicles • Mycobacterium are not seen and can't be cultured Tuberculids Papulonecrotic Tuberculid • Symmetric, necrotic papules that occur in crops over the extremities and heal by scarring • Dusky red, symptomless, peasized papules • Usually seen in children or young adults • • MTB DNA has been detected in about 50% of pts Papulonecrotic tuberculid. Erythematous papules and papulopustules on the heel. Tuberculids Papulonecrotic Tuberculid • Histopath: – Wedge-shaped necrosis of the upper dermis extending into the epidermis – Involvement of blood vessels is a cardinal feature • Consists of an obliterative and sometimes granulomatous vasculitis leading to thrombosis and complete occlusion Papulonecrotic Tuberculid Dusky red, pea sized papules that are symmetric and become necrotic Tuberculids Erythema Induratum (Bazin’s Disease) • Dusky-red 1-2 cm tender nodules usually occurring on the lower legs in middle-aged women • Resolve spontaneously w or wo ulceration • The vessels of these pts react abnormally to changes in ambient temp – The eruptions assoc w/ exposure to cold • Active TB is found only rarely Erythema Induratum www.emedicine.com Evidence of panniculitis exhibiting lobular, granulomatous, and lymphohistiocytic inflammation Nodules after resolving with ulceration Atypical Mycobacteria Mycobacterium marinum • “Swimming pool/fish tank” granuloma • Ulcerating lesions in skin at site of abrasions incurred in swimming pools about 2-3 wks. after inoculation • Single nodules, typically on hands, may ulcerate and suppurate with sporotricoid ascending spread • Fresh and salt water • Tx with Minocycline 100 mg bid • Heals spont. within 1-2 yrs. w/residual scarring Mycobacterium marinum Atypical Mycobacteria Mycobacterium ulcerans infection • Buruli ulcer, Bairnsdale ulcer, Searl ulcer • Subequatorial regions of Africa, wet, marshy, swampy areas • Never found outside the human body • Incubation period of ~3 mo • Painless subq swelling which enlarges to a nodule that ulcerates • Ulcer is deeply undermined and necrotic fat is exposed exposing muscle and tendon Atypical Mycobacteria Mycobacterium ulcerans infection • Histo- Central necrosis in the interlobular septa of the subcut. fat, surrounded by granulation tissue w/giant cells but no typical caseation necrosis or tubercles. AF orgs. can always be demonstrated. • TX- Excision of early lesion. Local heat, hyperbaric oxygen and chemo w/Rifampicin and Bactrim. M. ulcerans http://www.cdc.gov/ncidod/eid/vol5no3/dobos.htm In A, arrows indicate necrosis of adipose tissue distant from the location of AFB, and in B, the arrow indicates predominance of extracellular bacilli and microcolonies Atypical Mycobacteria Mycobacterium kansasaii • Unusual skin pathogen more commonly associated with pulmonary disease in middle-aged men – Infections localized to Midwestern states and Texas • Acquired from the environment • Variable skin presentations: – Nodules – Plaques – Crusted ulcers m/c in immuno-suppressed • Responsive to anti-TB tx: Streptomycin, Rifampicin, Ethambutol • Atypical mycobacterium most closely related to MTB Atypical Mycobacteria • Mycobacterium avium complex (MAI/MAC) • M. avium and M. intracellulare infects lungs and lymph nodes but occasionally causes cutaneous lesions with dissemination • Single or multiple painless, scaling, yellowish plaques w/ a tendency to ulcerate • Common in AIDS • Highly resistant to anti-TB drugs requiring several in combination: – Azithromycin, Rifampin, Ethambutol • Where feasible surgical tx is advisable • Rifampin used for prophylaxis http://meds.queensu.ca/~medpalm/PDA_Portal/case11.html Mycobacterium avium Mycobacterium intracellulare Atypical Mycobacteria Mycobacterium szulgai • Associated with: – Cervical lymphadenitis – Cellulitis – Draining nodules and plaques • Can also cause bursitis and pneumonia • More susceptible to antiTB drugs than most other atypical mycobacterium Atypical Mycobacteria Mycobacterium haemophilum • SubQ granulomatous eruptions – Immunosuppressed - HIV • Histo: – mixed polymorphonuclear and granulomatous inflam – “Dimorphic inflammatory response” • No caseation necrosis • May be sensitive to p-aminosaliclyic acid and Rifampin Atypical Mycobacteria Mycobacterium genavese • Little is known about this organism • Causes disseminated dz – Similar to M. avium intracellulare in HIV infected pts Atypical Mycobacteria Mycobacterium fortuitum complex • Three similar species: 1. M. fortuitum 2. M. chelonei 3. M. abscessus • • Saprophytes, found chiefly in soil and water Rarely cause human disease – Immunocompromised – Prosthetic heart valves and joints • Usually follows puncture wound or surgery Atypical Mycobacteria • Lymphangitic spread by Mycobacterium fortuitum. The inoculation chancre was on the foot. Leprosy (Hansen’s Disease) Etiology • Dreaded, chronic, poorly-transmissible granulomatous disease of the skin and nerves caused by acid-fast M. leprae • Probably least infectious of all diseases: – Strong cell-mediated immunity keeps organism at bay in most people – Humans only natural host but reservoirs: • 9-banded armadillo (Texas) • 3 species of monkey Leprosy Etiology • Pregnancy is a precipitating factor in 10-25% of female patients – Due to altered immunity • Approx 1/3 of newly dx'ed pts w/leprosy will eventually have some chronic disability – Secondary to irreversible nerve injury – M/C hands or feet Leprosy • Lepromin skin test – Analogous to the tuberculin test (intradermal inj of 0.1ml of a crude semi-standardized preparation of bacilli from a lepromatous nodule or armadillo liver) – Positive at 48 hours = Fernandez reaction – Positive again at 3-4 weeks = Mitusda reaction • Late reaction indicative of immune status of patient • Little is known about why different people respond differently to leprosy bacillus Leprosy Epidemiology • 5 million persons worldwide • 7 thousand active cases in USA • 250 new cases /year • 620,000 new cases worldwide/year. • 80% in 6 countries: Bangladesh, Brazil, India, Indonesia, Myanmar, Nigeria • Endemic in SE Asia, Far East, Africa, South/Central America • Cases in Puerto Rico, Cuba, USA Leprosy Biological behavior and transmission • Cell-mediated immune response – Low antigenicity • Obligate intracellular parasite • Grows only in colder areas: – skin, cutaneous nerves, testes, hands, feet • Multiplies in neurons in macrophages and keratinocytes causing nerve damage/disability Leprosy Biological behavior and transmission • Strips away myelin from nerve fibers – Directly harms nerve cells with involving the inflammatory system • Does not have to enter the schwann cells to cause degeneration of myelin Nerve Examination Sites 1) Ulnar Nerve Muscle wasting in hand with contracture 4th and 5th fingers with anaesthesia. Enlarged at or above Olecranon groove at elbow - may be confused with an enlarged Trochlear lymph gland adjacent to the nerve. 2) Median Nerve Muscle wasting and contractures of thumb and 2nd and 3rd fingers. Enlarged at anterior wrist but difficult to distinguish from adjacent tendons. 3) Radial Nerve Wrist drop - not common. An enlarged radial cutaneous nerve may be palpated at the lateral border of the radius proximal to the wrist. This nerve passes to the dorsum of the hand. 4) Lateral or External Popliteal Nerve Foot drop. May be palpated crossing the neck of the fibula. Can often be palpated in a normal muscular person. 5) Posterior Tibial Nerve Posterior and inferior to the medial malleolus. 6) Great Auricular Nerve A sensory skin nerve which crosses the sternomastoid muscle in the neck. It is usually not palpable in a normal person. 7) Skin Sensory Nerves near skin lesions may be enlarged. 8) 7th Cranial Nerve It is not palpable but damage to the nerve leads to facial paralysis and lagophthalmos. 9) 5th Cranial Nerve Sensory Fibers If it is damaged, it leads to anaesthesia of cornea. Leprosy Biological behavior and transmission • Transmission similar to TB – Nasal mucosa – Typically requires extensive contact • Incubation for Tuberculoid leprosy is up to 5 yrs and may be > 20 yrs Leprosy Diagnosis • 2 of 3 clinical criteria 1. Anesthesia of the skin 2. Thickened peripheral nerves 3. Typical skin lesions • Slit-skin smear (Abroad) – Tissue fluid exudate examined with Fite stain to determine bacterial index (multibacillary vs. paucibacillary) • Punch bx of skin lesion (USA) – Fite stain reveals intracellular bacilli – PCR Leprosy Diagnosis • Histologic changes helpful but are not diagnostic – One exception to this rule: • Presence of epitheloid cell granulomas w/in nerves = Tuberculoid leprosy or a severe reversal reaction. Leprosy Identification and Quantification of Bacilli • AFB in tissue are best shown by carbolfuschin staining using modifications of the Ziehl-Neelson method collectively called FiteFarraco stains • M. leprae are weekly acid fast • Rod shaped bacilli – Found in macrophages and nerves – Quantified logarithmically by the bacillary index (BI): the numbers of bacilli per oil-immersion field or the numbers of OIFs sought to find 1 bacilli Clasification of Leprosy Tuberculoid Leprosy • TT = Polar Tuberculoid – Features: • • • • • • Single to few anesthetic macules or plaques Hypopigmented Borders well defined Peripheral nerve involvement common Localized & asymmetrical May contact epidermis and do more damage to nerves than LL – Lepromin Rxn: very strong – Bacillary density: None Tuberculoid Leprosy Central HypoPigmentation Elevated Border Tuberculoid Leprosy Histology Linear granuloma following the course of a nerve Higher power view of granuloma surrounding the nerve Borderline Tuberculoid Leprosy Lesions similar to TT Borders less distinct Multiple (>5) Satellite lesions sometimes seen around larger lesions Peripheral nerves involved earlier Lepromin Rxn: Mild Bacillary Density: Scant Borderline Leprosy • Still more lesions that BT • Borders more vague • Asymmetric • Bizarre punched-out lesions • Hair loss • Anhydrosis • Most common type • Lepromin Rxn: Weak • Bacillary Density: Moderate Borderline Lepromatous Leprosy • • • • • • • • • Multiple macular/papular/plaques Symmetric lesions Vague borders Neuritis late then neural lesions Surface smooth and shiny with ill-defined border Mixed granulomas Leprae in neurons = enlargement Lepromin Rxn: None Bacillary Density: Heavy Borderline Lepromatous Leprosy Multiple Erythematous Plaques with Vague border Lepromatous Leprosy • Multiple, non-anesthetic, macular and papular lesions • No neural lesions until very late • Late complications: – Madarosis – Leonine facies – Testicular damage • Lepromin Rxn: None • Bacillary Density: Heavy Lepromatous Leprosy Note the diffuse infiltration of the face with leonine facies and madarosis Lepromatous Leprosy • Pts have masses of histiocytes – Do not form good granulomas – Lepra cells = foamy macrophages packed with bacilli – Globi = masses of bacilli – Grenz Zone = seperates epidermis from dermis Lepromatous Leprosy Indeterminate Leprosy • Vaguely defined hypopigmented or red macules • With or without sensory deficit • Lepromin Rxn: Weak • Bacillary Density: Rare Lucio Leprosy • Scleroderma-like with hair loss and telangiectasias • Diffusely seen in Mexican/Latin American patients • May give rise to obstructive vasculitis – Aka Lucio phenomenon Sequelae of Leprosy 1.Madarosis 2.Saddle nose 3.Blindness in the left eye Reactional States • 50% of patients after initiation of therapy • Causes considerable morbidity • Immune response-destructive, inflammatory process Reactional States Type 1 Lepra Reactions (upgrade) • • • • • • • • Jopling's type 1 Reaction Affects individuals with borderline disease Type IV hypersensitivity – Cell-mediated change Major Complication: Nerve swelling, pain and damage Cutaneous lesions become tender, erythematous Accelerated destruction of bacilli Treat promptly with prednisone 40–60 mg/daily Note downgrading reactions occur before the initiation of tx and represent shift to LL Reactional States Erythema Nodosum Leprosum (Type II lepra rxn) • Josling's type 2 reaction • Occurs in 50% of patients with LL and BL • Immune complex reaction (type III) between M. leprae antigens and host Ig • Widely distributed dermal nodules – Do not occur at previous skin lesions • IC precipitate in skin, endothelium, nerves, eyes • Systemic Sx’s: Fever, malaise, ulceration, neuritis, uveitis, glaucoma, acute inflammation • Tx with Thalidomide 400 mg daily Erythema nodosum leprosum (type 2 reaction) with the appearance of multiple red papulonodules in a patient with lepromatous leprosy Reactional States Lucio Phenomenon (Type III Lepra Reaction) • Latin Americans - Mexicans • Pts have La bonita's form of leprosy – Diffuse Lepromatosis • Lucio reaction results in large bullous lesions that ulcerate usually below knees – Due to deep cutaneous vasculitis (hemorrhagic infarcts) – Complications: sepsis and death – Tx: • Unresponsive to steroids or thalidomide • Antimicrobial chemo for leprosy • Wound care of ulcers Treatment of Leprosy Medications of choice • Dapsone: – 100mg/d in adults – 1mg/kg/d in children • Clofazimine (Lamprene): – 50-100mg/d in adults – unestablished in children • Rifampin: – 600mg/mo in adults Treatment of Leprosy Type of Leprosy Monthly Paucibacillary (I, TT, BT) Rifampin 600mg Daily Dapsone 100mg Duration 6 months Multibacillary (LL,BL,BB) Rifampin 600mg Clofazimine 50mg 24 months Clofazimine 300mg Dapsone 100mg Treatment of Leprosy Effective 2nd-line drugs • Ofloxacin • Minocycline • Clarithromycin Treatment of Leprosy Monitoring • Dapsone: – Baseline G6PD and Hgb • Rifampin: – Baseline LFTs and platelets • Baseline and q 2 week PE of sensation and motor nerve function first months of therapy • Opthalmology baseline and periodic exam • Repeat slit-skin, Bx, PCR for response to tx High Resistance Tuberculoid Leprosy • Characterized by: – Few lesions – Rare organisms – Epitheloid cell granulomas w/ tendency to self-cure – Plaques w/ sharp margins are the inscription of anti-M. leprae DTH on the skin – Nerve trunk palsies are its inscription on the peripheral nerves Low Resistance Lepromatous Leprosy • Characterized by: – Wide dissemination – Abundant orgs – Foamy macrophages – Untreated relentless progression