* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Preventing Medication Errors in Pediatric and Neonatal
Survey
Document related concepts
Transcript
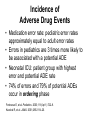
Preventing Medication Errors in Pediatric and Neonatal Patients Learning Objectives • Discuss common medication errors that occur in pediatric and neonatal patient care • Describe error reduction strategies for the pediatric and neonatal populations • Explain limitations of automated medication error reduction devices in these populations • Describe the role of the interdisciplinary team in preventing medication errors Adverse Drug Events • ADEs are injuries that result from drug use – May be preventable or nonpreventable • Potential ADEs result from medication errors with potential for harm but: – Are intercepted before reaching patient, or – Reach patient but do not cause harm . Incidence of Adverse Drug Events • Medication error rate: pediatric error rates approximately equal to adult error rates • Errors in pediatrics are 3 times more likely to be associated with a potential ADE • Neonatal ICU: patient group with highest error and potential ADE rate • 74% of errors and 79% of potential ADEs occur in ordering phase Fortescue E, et al. Pediatrics. 2003;111(4 pt 1):722–9. Kaushal R, et al. JAMA. 2001;285:2114–20. Reasons for Increased Risk • Different and changing pharmacokinetic parameters • Lack of pediatric formulations, dosage forms, guidelines • Calculation errors • Inconsistent measurement of preparations • Problems with drug delivery systems Pediatric and Neonatal Pharmacokinetics • One size doesn’t fit all – Preterm neonates (<36 weeks’ gestation) – Full-term neonates (birth to 30 days) – Infants (1–12 months) – Toddlers (1–4 years) – Children (5–12 years) – Adolescents (>12 years) Pediatric and Neonatal Pharmacokinetics • Do not use the terms interchangeably • Discuss patients in terms of age and weight to provide more accurate kinetic profile • Difference between adolescent and preterm neonate drug dose: potentially 100-fold Reasons for Increased Risk • Different and changing pharmacokinetic parameters • Lack of pediatric formulations, dosage forms, guidelines • Calculation errors • Inconsistent measurement of preparations • Problems with drug delivery systems Lack of Pediatric Formulations • May lead to: – Crushing tablets – Opening capsules and adding to food or beverage – Utilizing IV formulations for oral use – Using ophthalmic preparations in the ear – Giving oral anticonvulsants rectally – Compounding extemporaneous products Lack of Pediatric Formulations • Pitfalls of altering adult formulations – Insufficient data to support practice – Expiration dating of compounded formulation – Unknown bioavailability – Extemporaneous compounding errors Lack of Pediatric Formulations • Barriers to commercial availability – Complications of testing in pediatric patients • Concerns involving informed consent • Recruitment problems (e.g., too few patients) • Determining which pediatric subset to test – Market limitations • Cost of testing may outweigh expected market • Market share typically less than in adult market • Less financial incentive to manufacturers for most disease states Attempts to Overcome Barriers • American Academy of Pediatrics – Shared responsibility to conduct research in children to support rational drug therapy in children • Amendments to the Food, Drug, and Cosmetics Act Pediatric Research Equity Act (PREA) and Best Pharmaceuticals for Children Act – 2003, 2007 • Manufacturers of drugs or biologics that submit an application to market a new active ingredient, indication, dosage form, dosing regimen, route of administration must include a pediatric data assessment • Provided 6-month exclusivity extension • Provided funding for research of “orphan” therapies Sources of Errors • Confusion between adult and pediatric formulations • Confusion among oral liquid concentrations • “Look-alike” and “sound-alike” packaging and names • Multiple dosing styles Adult Versus Pediatric Formulations • Different concentrations • Different volumes • Should be stored in separate locations to avoid errors – Within the pharmacy – On nursing units Oral Liquid Concentrations • Multiple concentrations of same product • Fatal overdoses occur annually • Example of dangerous situation – Available liquid acetaminophen products: • 100 mg/mL Infant drops • 160 mg/5 mL Children’s liquid • 167 mg/5 mL Adult extra strength – Ask parent to give a child 5 mL of Tylenol • Child is 4 years old • Parents only have drops; give 5 mL of drops (500 mg) • Correct dose should have been 160 mg Look-Alike, Sound-Alike • Medication names • Medication packaging • Confusion between IV and oral products – This problem has increased in pediatrics as practice of using IV medication for oral administration has increased Additional Information on Look-Alike and Sound-Alike Medications and Packaging Available in Slide Deck for Chapters 6 and 7 Multiple Dosing Styles • Daily dosing versus every 6 hours – Acetaminophen 10–15 mg/kg/dose q 6–8 hr – Ampicillin 100–200 mg/kg/24 hr divided q 6hr – Practitioners must read the fine print • Watch your units! – mcg/kg/min versus mg/hr versus mcg/kg/hr – Electrolyte dosage • mEq versus mg versus grams Reasons for Increased Risk • Different and changing pharmacokinetic parameters • Lack of pediatric formulations, dosage forms, guidelines • Calculation errors • Inconsistent measurement of preparations • Problems with drug delivery systems Calculation Errors • Misuse of decimals Wrong Right .1 mg 0.1 mg 1.0 mg 1 mg Way to remember: if the decimal is not seen, 10-fold error might be made • Ordering a dose in volume – Creates ambiguity if medication is available in several different concentrations Calculation Errors • Single dose divided by frequency – 3 mg/kg every 8 hours • Example: 10 kg patient – Correct: 30 mg every 8 hours – Incorrect: 30 mg daily divided every 8 hours » (10 mg every 8 hours) • Not dividing daily dose by frequency – 6 mg /kg/day divided every 8 hours • Example: 10 kg patient – Correct: 20 mg every 8 hours (60 mg total daily dose) – Incorrect: 60 mg every 8 hours Calculation Errors • Errors in unit conversion • Miscalculation of body surface area • Misplaced decimals – Compounded errors: 10-fold errors • Errors calculating drip rates • Weight-based errors – Using wrong weight or old weight – Expressing weight as lb (wrong) instead of kg (right) Insulin Dilution • For insulin doses ≥5 units – May use the 100 units/mL concentration • For insulin doses <5 units – Dilute insulin in pharmacy to 10 units / mL – Only send individual, patient-specific doses to nursing unit – Vials of diluted insulin should not leave pharmacy – A 1 mL tuberculin syringe is used to administer Reasons for Increased Risk • Different and changing pharmacokinetic parameters • Lack of pediatric formulations, dosage forms, guidelines • Calculation errors • Inconsistent measurement of preparations • Problems with drug delivery systems Oral Measuring Devices • Oral medications more likely to be dispensed in bulk and not in unit of use • 3 out of 4 households still use kitchen teaspoons for measuring* • Pre-packaged dispensing cups or droppers – Mistaken for whole doses versus graduated dosing • Various calibration units on syringes – Varies on different syringe sizes *Institute for Safe Medication Practices. Safety briefs. ISMP Medication Safety Alert! February 26, 1997;2:1. Rule of 6 • The “Rule of 6” is an equation used to calculate the amount of drug to add to 100 mL of IV fluid so that an infusion rate of 1 mL/hr will deliver 1 mcg/kg/min 6 x weight (kg) = amount of drug (mg) 100 mL of solution Concerns With Rule of 6 • Not consistently used • Calculations and mixing may be completed at bedside without pharmacy double check • Typically done with critical care, high-risk drugs • Dosage adjustments can result in fluid overload – Error risk compounded when double or triple concentrating infusions • Drug waste The Joint Commission and the Rule of 6 • 2002: National Patient Safety Goal (NPSG) requiring standardization and limitation of concentrations of high-alert medications in all patients • Hospitals were allowed to apply for exemption for Rule of 6 • By December 31, 2008, all hospitals must comply with standardization Reasons for Increased Risk • Different and changing pharmacokinetic parameters • Lack of pediatric formulations, dosage forms, guidelines • Calculation errors • Inconsistent measurement of preparations • Problems with drug delivery systems Administration of Enteral Fluids • Enteral pumps may not be able to deliver small enough volumes to neonates – Parenteral syringe pumps have been used instead • Increases risk for accidental IV administration • To prevent accidental IV administration of enteral products – Trace tubing to point of origin prior to connecting tubing – Label tubing, administration sets, pumps – Use non-Luer feeding tubes • Will connect only with oral syringes Strategies for Medication Error Reduction Strategies With Highest Error Prevention Potential in Pediatric Patients • Improved communication among physicians, nurses, and pharmacists • Unit-based clinical pharmacists making rounds with the health care team • Use of computerized prescriber order entry (CPOE) with decision support Fortescue E, et al. Pediatrics. 2003;111(4 pt 1):722–9. Staff Competencies • Require math competencies for all staff • Develop competencies for entire team before new service is implemented • Provide resources for maintaining competency for pediatric and neonatal pharmacology • Ensure competency on all staffing shifts Patient Information • Provide patient age and date of birth – Decreases risk of confusing age in years versus months • Weight and height in metric measures only • Patient’s medication history – Include concentration of all medications – Record doses in milligrams, not in volume – Specifically ask about common OTCs • Acetaminophen, ibuprofen, vitamins Know Your Own Height and Weight • Provides a frame of reference • Know your height in centimeters • Know your weight in kilograms Reduction of Calculation Errors • Establish reliable method of providing current patient weight in kg to the health care team • Require calculated dose and dose per weight (i.e., mg/kg) on each order – Acetaminophen 100 mg (10 mg/kg) every 6 hours by mouth – Exceptions • Vitamins, topicals, other medications not requiring weightbased dosing • Require independent double check of dosing calculations Reduction of Calculation Errors • Use pre-calculated dose sheets – Emergency medication sheets – Commonly used medications • Standardize dosing and concentrations – IV drip rates or concentrations – Recipes and strengths for extemporaneous compounds • Provide pediatric references in ordering, dispensing, and administration locations • Encourage rounding to whole numbers when possible Reduction of Calculation Errors • Include warnings for potentially low or high doses in the pharmacy and CPOE systems • Appropriately use decimal points – Utilize leading zeros: – Do not use trailing zeros: 0.1 (right) 1 (right) .1 (wrong) 1.0 (wrong) Reduction of Prescribing Errors • Verbal orders – Only for emergent/urgent situations • Always write down order and read back – Not allowed when the prescriber and chart are available – Not accepted by pharmacy without written confirmation (prescription faxed/sent prior to dispensing) – Limit to formulary drugs – Received only by those authorized by the hospital to do so – Spell drug names and pronounce numeral digits • Fifty, Five Zero – Never accept verbal chemotherapy orders – Have order signed by prescriber as soon as possible Cohen MR. Medication Errors. Causes, Prevention, and Risk Management; 11.1–11.16. Reduction of Prescribing Errors • Write directly into patient’s chart • Avoid abbreviations – Do not use u for unit; spell out “unit” • U can be misread as a zero • 10u can be misread as 100 – Do not use cc; use mL • cc can be misread as 00 • 1cc has been interpreted as 100 • Include patient weight in each order Reduction of Dispensing Errors • Standardize concentrations • Use one consistent formula or standard concentration • Use commercially available unit of use preparations whenever feasible • Have pharmacy prepare all IV admixtures and oral liquid preparations • Independently double check prior to dispensing Reduction of Administration Errors • Oral liquids – Dispense in unit of use • Oral syringes • Dispensing bottles – Do not administer oral liquids with IV syringes • Syringe tips are a choking hazard – Only utilize dosing graduated cups or oral syringes • Oral syringes have caps that are harder to remove Reduction of At-Home Administration Errors • Dispense appropriate measuring device with each prescription and refill • Review dosing instructions with caregivers • Suggest a “1 caregiver” administration policy – Prevents overdoses by well-meaning multiple caregivers administering doses • Ask caregiver to demonstrate administration technique – Including measuring doses Medication Safety in Pediatric Emergencies • Broselow tape – “Measuring tape” placed next to a supine child – Based on child’s length, tape estimates child’s weight • Broselow tape and code medication concentrations must match within a facility • Educate staff on proper use and limitations of using tape • Utilize most recent tape version • Limitations for Broselow tape – Incorrect positioning next to child – Doses may be expressed in volume – Provides directions to make infusions with non-standard concentrations Section of Broselow Tape Medication Safety in Pediatric Emergencies • Provide age-appropriate code trays – Adult, pediatric, neonatal – Set appropriate par levels • Provide pre-printed “code sheets” – Weight-based dosing algorithms – Ideally, print individualized code sheets for each patient • Establish verbal order procedures • Involve a pharmacist in ED medication use Reducing Errors in the Pediatric OR • Within therapeutic classes – Reduce number of drugs and concentrations • Label all medications placed on and off sterile field including: – Drug name – Concentration/strength – Date and initials of person preparing • The Joint Commission NPSG • Segregate neuromuscular blocking agents from other medications Reducing Errors in the Pediatric OR • Add required medications to surgeon’s preference cards or pre-printed order forms – Avoids verbal orders or faxes from OR • Standardize medications and concentrations for same procedures • Advocate for weight-based preparation of anesthesia supplies – Provide standardized trays • Communicate information about perioperative medication use to postoperative care team Pre-Procedure Sedation • Often prescribed for administration at home prior to arrival at physician’s office – Chloral hydrate and benzodiazepines most common • American Academy of Pediatrics – Children should not receive sedatives without supervision and monitoring by skilled medical personnel with appropriate resuscitation equipment Automation • Automated Dispensing Cabinets (ADC) • Bar Code Point of Care (BPOC) • Computerized Prescriber Order Entry (CPOE) • “Smart” Infusion Pumps Role of Automation in Pediatric and Neonatal Services • Safety – CPOE: Ability to check prescribed doses against patient weight – ADCs make dosages available for emergent or after hours use – Bar coding checks for correct patient, drug, dose, dosage form, and time at point of drug administration – Smart infusion pumps allow for safety checks on standard concentrations prior to infusion Pitfalls of Automation in Pediatric and Neonatal Services • CPOE – Data are only as accurate as information entered – Correct patient weight may not be in system – Labels may not be appropriate for pediatric dosage forms • Bar code reading – Difficult on pediatric dosages – Difficult on pediatric and neonatal arm/leg bands Pitfalls of Automation in Pediatric and Neonatal Services • ADCs – Medications requiring further preparation or measurement by the nurse may be stored in ADC – Drugs may be obtained before pharmacist review (override) – When accessing one particular drug, nurse may have access to other drugs • “Smart” infusion pumps (use a drug library to provide alerts if pump is potentially misprogrammed) – Systems may not allow for hundredths decimal place – Doses in small total volumes may not account for volume needed to fill tubing – Infusion rates can be checked only if IV drug is a standard concentration Additional Information on Automation Available in Slide Deck for Chapter 15 References Cohen MR. Medication Errors. Causes, Prevention, and Risk Management; 11.1–11.16. Fortescue E, Kaushal R, Landrigan CP, et al. Prioritizing strategies for preventing medication errors and adverse drug events in pediatric inpatients. Pediatrics. 2003;111(4 pt 1):722–9. Institute for Safe Medication Practices. Safety briefs. ISMP Medication Safety Alert! February 26, 1997;2:1. Kaushal R, Bates DW, Landrigan C, et al. Medication errors and adverse drug events in pediatric inpatients. JAMA. 2001;285:2114–20.