* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Dynamic Cardiology Station for Paramedic National Registry
Survey
Document related concepts
Transcript
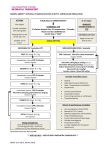
Cardiac Arrest Skills Station 1 Registry Skills Review Compiled and presented by IHCC EHS 2001 paramedic students: • Margaret Lind • Steven Rudolph • Karen Thomas Assembles Necessary Supplies • • • • • • Defibrillator Airway Adjuncts Oxygen Supplies Medications Monitor Leads Defibrillator Pads or Conductive Jelly Takes or Verbalizes Infection Control Precautions • Dons Personal Protective Equipment • Verbalizes Appropriate Level of Protection • Takes Necessary Precautions to Avoid Exposure Critical Criteria These are actions that will result in automatic failure of station! • • • • • • • • • • Failure to Verify Rhythm before Delivering Each Shock Failure to Ensure the Safety of Self and Others (Verbalizes “All Clear” and Observes) Inability to Deliver DC Shock (Does Not Use Machine Properly) Failure to Demonstrate Acceptable Shock Sequence Failure to Order Initiation or Resumption of CPR when Appropriate Failure to Order Correct Management of Airway (ET when Appropriate) Failure to Order Administration of Appropriate Oxygen at Proper Times Failure to Diagnose or Treat 2 or More Rhythms correctly Orders Administration of an Inappropriate Drug, or Lethal Dosage Failure to Correctly Diagnose or Adequately Treat V-Fib, V-Tach, or Asystole Checks Level of Responsiveness • Levels of Responsiveness – Alert – Verbal Stimuli – Painful Stimuli – Unresponsive Checks ABC’s • Airway – Patent – Simple Adjuncts • Breathing – Adequate Rate and Rhythm – Oxygen • Circulation – Gross Bleeding – Pulses Present Initiates CPR- If Appropriate (Verbally) • Pulse and Breathing Absent • Assemble Defibrillator While CPR in progress Performs “Quick Look” with Paddles • • • • • • • 1. Turn on EKG monitor 2. Turn the lead selector to PADDLES 3. Apply conductive jelly or use defibrillation pads 4. Place paddles firmly on the bare chest with the paddle marked STERNUM on right chest near sternum, and paddle marked APEX on lower left chest 5. Adjust EKG size 6. Observe scope and determine patients condition. Check pulse and verify absence of pulse 7. If fatal dysrhythmia is noted, proceed with defibrillation algorithm Cardiac Arrest Skills Station Dynamic Cardiology • • • • • • • • • • • • • • • • Correctly interprets initial rhythm Appropriately manages initial rhythm Notes change in rhythm Checks patient condition to include pulse, Correctly interprets second rhythm Appropriately manages second rhythm Notes change in rhythm Checks patient condition to include pulse, Correctly interprets third rhythm Appropriately manages third rhythm Notes change in rhythm Checks patient condition to include pulse, Correctly interprets fourth rhythm Appropriately manages fourth rhythm Notes change in rhythm Checks patient condition to include pulse, and if appropriate, BP and if appropriate, BP and if appropriate, BP and if appropriate, BP Orders high percentages of supplemental oxygen at proper times • Administer high flow oxygen – 12-15 LPM per NRB mask, or – 12-15 LPM connected to BVM, or – Positive pressure ventilation Correctly Interprets Initial Rhythm • Fatal Dysrhythmias – Ventricular fibrillation (VFib) – Pulseless ventricular tachycardia (VTach) – Asystole – Pulseless electrical activity (PEA) – Electromechanical Dissociation (EMD) – Bradycardia (non-arrest) – Tachycardia (non-arrest) Appropriately Manages Initial Rhythm • VTach, VFib – Defibrillate with 200J • Asystole V Fib – Follow Asystole algorithm • PEA, EMD Sinus Tach – Follow PEA algorithm Ventricular Fibrillation & Ventricular Tachycardia • • • • • • VFib • • ABC’S, and CPR Defibrillate up to 3 times, 200 Jules, 200300 j., 360j. If persistent or recurrent VF/VT continue CPR, and intubate Start IV Epinephrine 1mg IV push (repeat every 3-5 min.) Defibrillate. 360 J within 30-60 seconds. Administer medications of probable benefit – – – – VTach • Lidocaine 1.0-1.5mg IV push Bretylium 5mg IV push Magnesium Sulfate 1-2g IV over 1-2 min Procainamide 30 mg/min Defibrillate 360 J after each dose of medication (drug- shock, drug- shock) Asystole • • • • • Continue CPR Intubate Start IV Confirm Asystole in more than one lead Consider possible causes – – – – – – • • • Hypoxia Hyperkalemia Hypokalemia Preexisting acidosis Drug overdose Hypothermia Epinephrine 1mg IV push Atropine 1mg IV push Consider termination of efforts Pulseless Electrical Activity Electromechanical Dissociation • • • • Continue CPR Intubate Start IV Consider possible causes - treatments – – – – – – – – – • • Hypovolemia -Volume infusion Hypoxia - Ventilation Cardiac Tamponade - Pericardiocentesis Tension Pneumothorax - Needle decompression Hypothermia - See Hypothermia algorithm Massive pulmonary embolism - surgery, thrombolytics Drug overdose - Appropriate therapies Hyperkalemia - Sodium bicarbonate Massive acute myocardial infarction - See AMI algorithm Epinephrine 1mg IV push If Bradycardia – give Atropine 1mg IV push Bradycardia (non-arrest) With serious signs and symptoms Sinus Bradycardia • • • • Assess ABC’s Secure airway Start IV Attach ECG, pulse oximeter, blood pressure cuff • Assess vitals, get patient history • Perform physical exam • Interventions – – – – Atropine 0.5-1mg Transcutaneous pacing Dopamine 5-20ug/min Epinephrine 2-10ug/min • Prepare for transvenous pacer Tachycardia (non-arrest) • Assess ABC’s With serious signs and symptoms • • • • Attach ECG, pulse oximeter, blood pressure cuff Assess vitals, obtain patient history Perform physical exam If heart rate >150 – Immediate cardioversion • If heart rate<150 – Give medications – Wide complex Sinus Tachycardia • Lidocaine • Procainamide • Bretylium – Narrow complex • Adenosine • Verapamil – Cardioversion 100 J. The End