* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Slides
Survey
Document related concepts
Transcript
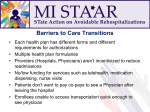
Reducing Readmissions through The Re-Engineered Discharge – (Project RED) Suzanne Mitchell, MD MS Assistant Professor, Family Medicine Department of Family Medicine / Boston University School of Medicine March 25, 2014 Participants:1-866-639-0744, no code needed The Re-Engineered Discharge (Project RED) March 25, 2014 Suzanne Mitchell, MD MS Assistant Professor, Family Medicine Department of Family Medicine / Boston University School of Medicine Agenda I. II. III. IV. V. The Transition Problem How We Got Started The RED Process Brief Mention of Health IT? Lessons Learned from Dissemination “Perfect Storm" Patient Safety “Perfect Storm" of of Patient Safety • 39.5 million hospital discharges/year = Costs totaling $329.2b! • 20% readmitted within 30 days • Hospital discharge is not-standardized: • • • • • • Loose Ends - pending and post-dc tests Communication – with PCP, ESL, Health lit Poor Information - dc summary quality and availability Poor Preparation – knowledge of dx, meds, appts Great Variability – day of the week Fragmentation – who is in charge? • Hospital Discharge is not safe! • 19% of patients have a post-discharge AE A Real Discharge Instruction Sheet ResearchQuestions We asked: • Can improving the discharge process reduce adverse events and unplanned hospital utilization? Grant reviewer asked: • What is the “discharge process”? Question for you…… • Do you know what your hospital’s discharge process is? • Do you know the parts of the process where problems are occurring for patients or hospital personnel? • ie, occurring before or following discharge? • How are you identifying the problem spots? Principles of the RED: Creating the Toolkit Readmission Within 6 Months Patient Readmitted Within 3 Months Hospital Discharge Probabilistic Risk Assessment Process Mapping Failure Mode and Effects Analysis Qualitative Analysis Root Cause Analysis THE RED INTERVENTION Two key components • In Hospital –> Preparation & Education of written plan • AHCP • After Discharge – Reinforcement of the plan • Phone call within 72 hours after discharge • Assess clinical status • Review medications and appointments RED Checklist Twelve mutually reinforcing components: 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. Medication reconciliation Reconcile dc plan with National Guidelines Follow-up appointments Outstanding tests Adopted by Post-discharge services National Quality Written discharge plan Forum What to do if problem arises Patient education as one of 30 Assess patient understanding "Safe Practices" Dc summary to PCP (SP-11) Telephone Reinforcement Provide Language Services RCT MethodsRED Intervention N=375 Enrollment N=750 Randomization Usual Care N=375 30-day Outcome Data •Telephone Call •EMR Review Enrollment Criteria: •English speaking •Have telephone •Able to independently consent •Not admitted from institutionalized setting •Adult medical patients admitted to Boston Medical Center (urban academic safety-net hospital) Personalized cover page MEDICATION PAGE (2 of 3) APPOINTMENTS PAGE PRIMARY DIAGNOSIS PAGE Question for you…… • Does your institution have a patient-centered discharge document? • If no, what are the barriers to providing such a document? • If yes, • What are the design elements that facilitate communication? • What design elements support patient self-management? FINDINGS from Project RED RCT How well did we deliver intervention RED Component Intervention Group (No,%) (N=370) * PCP appointment scheduled 346 (94%) AHCP given to patient 306 (83%) AHCP/DC Summary faxed to PCP 336 (91%) PharmD telephone call completed 228 (62%) Primary Outcome: Hospital Utilization within 30d after Discharge Readmissions Total # of visits Rate (visits/patient/month Usual Care (n=368) Intervention (n=370) 76 0.20 55 0.15 90 0.24 61 0.16 166 0.45 116 0.31 P-value ED Visits Total # of visits Rate (visits/patient/month) Hospital Utilizations * Total # of visits Rate (visits/patient/month) * Hospital utilization refers to ED + Readmissions 0.009 Secondary Outcomes Usual Care (n=368) Intervention (n=370) No. (%) No. (%) P-Value PCP follow-up rate 135 (44%) 190 (62%) <0.001 Identified dc diagnosis 217 (70%) 242 (79%) 0.017 Identified PCP name 275 (89%) 292 (95%) 0.007 * Outcome Cost Analysis Cost (dollars) Usual Care (n=368) Intervention (n=370) Difference Hospital visits 412,544 268,942 +143,602 ED visits 21,389 11,285 +10,104 PCP visits 8,906 12,617 -3,711 442,839 292,844 +149,995 1,203 791 +412 Total cost/group Total cost/subject We saved $412 in outcome costs for each patient given RED Medication Errors at 2 Day Call (n=197) Failure to take medication No. (%) Patient did not think s/he needs med 19 (15%) Patient did not fill due to cost 21 (17%) Patient did not pick up from pharmacy 14 (11%) Patient did not get prescription on discharge 15 (12%) Patient self-discontinued due to side effects 14 (11%) Patient did not fill because of insurance 10 (8%) Incorrect Administration No. (%) Wrong frequency/interval 39 (21%) Wrong dose on prescription 33 (18%) Overall, 51% experienced error within 2 days! Question for you….. • Have you tried any strategies to communicate with patients following discharge? • Are you able to make PCP appointments at the time of discharge? • What strategies are you using for medication reconciliation at the time of discharge? Implications Should all patients get RED? Question for you….. • Is your institution doing risk stratification at the time of admission? Who is at risk of Rehospitalization? • CHF, COPD, Dementia • High risk Meds • Elderly • LOS • Co-morbidity • Men • Substance Abuse • Health Literacy (REALM) • Depression (PHQ-9) • Patient Activation (PAM) • Frequent Fliers (>2 in 6 months) Can Health IT assist with providing a comprehensive discharge? Health IT to Save Time Virtual Patient Advocates • Emulate face-to-face communication • Develop therapeutic alliance-empathy, gaze, posture, gesture • Teach AHCP • Tailored • Do “Teach Back” • Can drill down • Print Reports • High Risk Meds Lovenox Insulin Characters: Louise (L) and Elizabeth (R) Overall Usability Overall Satisfaction Ease of Use Who Would You Rather Receive Discharge Instructions From? 36% prefer Louise 48% neutral 16% prefer doc or nurse “I prefer Louise, she’s better than a doctor, she explains more, and doctors are always in a hurry.” “It was just like a nurse, actually better, because sometimes a nurse just gives you the paper and says ‘Here you go.’ Elizabeth explains everything.” 1=definitely prefer doc, 4=neutral, 7=definitely prefer agent Question for you….. • Is your institution using health IT to streamline the hospital discharge process? • What processes are you automating? • What are the benefits/challenges of using health IT for discharge process? Barriers to RED • Can appointments be made? • Will RED delay discharge time? • Who serves as the Discharge Educator? • Who does the 2 day phone call? • Who Produces the AHCP? Can we Re-Engineer the Hospital Ward? Success stories Boston HealthNet plan Period -> calendar year 2011 Patients given RED -> 500 – Discharge educator = dedicated RN – Post discharge phone call = plan’s care manager Results -> 30 day all cause readmission rate Cost savings -> well over 400k RED for Boston HealthNet RED Implementation – Strategies During hospitalization • Formal risk screening • Process for patient education • Discharge educator • Developing and teaching ACHP • Pharmacist • Standardized communication • Primary care providers • Other providers • Home care • Nursing Home RED Implementation – Strategies Prior to Discharge • Discharge Nurse Educator • Uses checklist • Assesses patient understanding of discharge plan (Teach back process used) • Care Team • Discusses discharge plan daily at team huddle • Patient • Receives individual written discharge plan RED Implementation – Strategies at time of discharge • Discharge is not rushed or late in the day • AHCP and discharge summary are sent to PCP office • Patient reminded about post discharge phone call • phone number for follow-up call confirmed RED TEAM-based CARE MD team RN team Case Mgmt Unit Coordinator/ Rounding Asst Educate patient Confirm medication plan Coordinate post discharge services Arrange 7-10 days post discharge follow up visit Discuss outstanding issues Teach AHCP Review steps to take when problems arise Prepare AHCP Reconcile discharge plan with national guidelines Assess degree of understanding – Teach Back Reinforce AHCP 24-48 hrs posthospital discharge phone call Transmit AHCP & discharge summary 24 hours post dc Barriers to High Quality Transitions • • • • • • • “Heads on Beds” Med reconciliation Discharge summary Hospital-PCP communication Language and health literacy Cognitive Issues Plan delegated to interns Role of Senior Leadership • Set the vision and the goal • Communicate Commitment • Newsletter, grand rounds, M+M, RCA, emails • Provide resources & staff • Create implementation team • Set policies to integrate across organizational boundaries • Get IT on board • Hold people accountable • Recognize and reward success 41 Role of Implementation Team • Recruit a collaborative, interdisciplinary team • Identify process owners and change champions • Staff Engagement • Energize staff • Get buy-in • • • • Implement a Plan that will work Build skills to support and sustain improvement Trouble shoot as RED is rolled out Monitor progress to provide feedback 42 Question for you….. • What barriers or facilitators have you faced in helping to manage your hospital discharge process better? Conclusions • Hospital DC is low hanging fruit • Changing the Culture of Hospitals is Hard • RED • Can decreased hospital use • 30% overall reduction, NNT = 7.3 • Saves $412 per patient • Health IT has great potential • Team-based Efficiency key to implementation • Determining who benefits is important QUESTIONS FOR ME?? Thank you! [email protected] http://www.bu.edu/fammed/projectred/ Thank You! Questions [email protected] [email protected] Project RED Website http://www.bu.edu/fammed/projectred/ Upcoming RARE Events…. Stay tuned for the next RARE Mental Health Webinar’s: April 21, 2014 Care Transitions Interventions in Mental Health Harold Pincus, Columbia University May 19, 2014 In-REACH Program Elizabeth Keck, Allina Health June 26, 2014 New York Office of Mental Health Dr. Molly Finnerty Future webinars… To suggest future topics for this series, Reducing Avoidable Readmissions Effectively “RARE” Networking Webinars, contact: Kathy Cummings, [email protected] Jill Kemper, [email protected]