* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Diagnostic and Therapeutic Pitfalls in Myasthenia Gravis
Pharmaceutical industry wikipedia , lookup
Drug interaction wikipedia , lookup
Prescription costs wikipedia , lookup
Adherence (medicine) wikipedia , lookup
Neuropharmacology wikipedia , lookup
Azathioprine wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Dydrogesterone wikipedia , lookup
Pharmacogenomics wikipedia , lookup
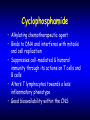
Myasthenia Gravis Shahriar Nafissi, MD Associate Professor of Neurology Tehran University of Medical Sciences Diagnosis • “Delaying the diagnosis of ocular MG is inconsequential but making an erroneous diagnosis has serious implications” Daroff RB. The office tensilon test for ocular MG. Arch Neurol 1986;33:843–844 Clinical Features When to question the clinical diagnosis • Acute course, spontaneously improving • Clustering of cases • Autonomic symptoms – – – – Orthostatic hypotension Sluggish pupils Constipation, dry mouth Reduced sweating • Decreased tendon reflexes • Familial • Minor symptoms since infancy/childhood Clinical Features • No objective finding • Diagnosis based solely on subjective response to Mestinon • Lack of clues pointing to the immunemediated nature – – – – Antibodies Thymus Response to IS, IVIG, PE Associated autoimmune diseases • Does myasthenic crisis only happen in MG? Therapeutic trial Diagnosis should not be based on subjective improvement of symptoms especially with Mestinon Tensilon Test • Pitfalls – Acute decompensation • Oropharyngeal Weakness • Cholinergic Weakness – Subjective vs. objective improvement • Some believe that it should be performed only in patients with ptosis/ophthamoplegia – Technical: • Subcutaneous injection • Not adequately flushed • Expired drug • Complications – from 23,111 edrophonium tests, 37 (0.16%) were associated with a serious complication, most often bradyarrhythmias and syncope. Respiratory failure, seizures, vomiting, and TIA were also reported – Sensitivity • Generalized MG: 72-95% • Ocular 60-86% – Specificity 97% – False positive results: • • • • Ocular> Generalized Other NMJ disorders: LEMS, Botulism, CMS LMN syndromes e.g., MND Others: brainstem glioma, MS, pituitary tumor, compressive aneurysm, GBS, Diabetic 6th palsy and inflammatory myopathy Anti-Acetylcholine Receptor Antibody • High Affinity AChR-Ab – Find a reliable laboratory – Sensitivity : • Ocular 39-71% (44%) • Generalized 87-98% (our data 82%) • Sometimes negative first, become positive later – Specificity 95-99% – Seronegative MG (~15%) • 30-70% MuSK-Positive • 66% of AChR- , MuSK- cases have low affinity AChR Ab • Low affinity MuSK Ab – False positive • SLE, RA, inflammatory neuropathy, motor neuron disease • Thymoma without MG, D-penicillamine • Relatives of patients with MG – Not useful in monitoring response to therapy Repetitive Nerve Stimulation • Sensitivity – Depends on the number of muscles tested – Ocular 11-39% – Generalized 53-98% • Specificity 95-98% Common pitfalls – Technical • Artifacts • Submaximal stimulation • Temperature < 35º C – Testing 1-2 muscles, mainly distal – Relying on borderline results – Missing other NMJ disorders • LEMS, Botulism, CMS Technical factors Ampl (mV) over Study 10 5 0 1 R AB D D IG MIN (U L) SHARIATI HOSPITAL Department of Neurology, Electromyography Unit Repetitive CMAP After Single Stimuli Patient ID: 1350 Name: mohammadi, nahid Date of birth: 01/01/1985 NCV / myasthenia test 02/25/2007 01:39:3 A1 N. ulnaris / M. abd. dig. m. 5.0 ms/Div, 3000.0 uV/Div, 1/0, 12mA Area A1 Lat A2 A2 A3 A4 A5 A6 A7 A8 A9 TOENNIES 20 10 0 Change of Ampl. - > M1 N. ulnaris right [%] Change of Area - > M1 N. ulnaris right [%] -10 -20 -30 -40 -50 -60 0 1 Stim. Site N. ulnaris right 12/18/2007 2 3 4 5 6 7 8 9 10 M resp. Decrem. Ampl. [%] Decrem. Area [%] 35.8 45.4 TOENNIES NeuroScreen® Plus 1.70c Page - 1 R ABD POLL BR EVIS Ampl (mV) over Study 5.0 2.5 0.0 1 R EXT D IG BR EVIS Ampl (mV) over Study 10 5 0 1 2 R ULNAR - ADM 1 2 3 4 R COMM PERONEAL - EDB 5 1 2 3 4 5 Ankle 1 Wrist 1 30ms 5mV 46mA 2 1 2 1 3 4 30ms 5mV 63mA 1 2 5 B.Elbow 2 4 5 after 10s exercise 30ms 5mV 46mA 30ms 5mV 63mA 2 1 3 5 FibHead 2 30ms 5mV 46mA 3 3 4 3 4 5 after 10s exercise 30ms 5mV 63mA 3 R ABD D IG MIN (U L) Ampl (mV) over Study 10 5 0 1 False positives – Denervating diseases (MND) – Myopathies • Channelopathies • Myotonic dystrophy • Metabolic (McArdle) Myotonic Dystrophy R ABD D IG MIN (U L) Amyotrophic Lateral Scleros R ABD POLL BREVIS R ABD POLL BREVIS Ampl (mV) over Study 5.0 2.5 0.0 1 2 3 Single-Fiber EMG • Sensitivity: – Ocular 86-97% – Generalized 98-100% • Specificity 94-98% • Normal jitter in a clinically weak muscle virtually excludes MG • False Positive Results – – – – Other NMJ disorders BTX injection Neurogenic Processes, e.g., MND Myopathies: PEO, Myositis • In a patient with clinical features of NMJ, specificity is high • Helpful in differentiating central and psychogenic causes of fatigue from MG R FRONTALIS 20 10 0 0 100 200 Jitter (µs) 10m s 100 µV Ri s in g E d ge/ Ris i ng E dge 10m s 100 µV 5m s 200µ V Ri s in g E d ge/Ris i ng E dge 15m s 200 µV Ri s in g E d ge/Ris i ng E dge MuSK-Positive MG • • • • • • More severe disease, pure ocular cases rare 30-70% AChR-Ab negative cases 80-100% cases female Severe involvement of facial and bulbar muscles RNS and SFEMG negative in limb muscles Thymus pathology rare; not responsive to thymectomy • Many cases non-responsive or non-tolerant to Mestinon • Usually requires Immunosuppressive therapy • Complete remission<10%, IS withdrawn<20% MuSK-positive patients strong inverse correlation with latitude north of the equator Treatment Mestinon • Symptomatic therapy; doesn’t affect underlying mechanism • No fixed dose schedule – With any dose, some muscles get stronger, some don’t change and others get weaker – Need more drug with menstruation, emotional stress, hot weather, infection • If needs too much or if response suboptimal, consider other medications Mestinon • Cholinergic Weakness • Don’t forget irreversible damage to NMJ • MuSK-Positive Patients • When used in combination to IS, try to discontinue Mestinon as soon as the patient becomes symptom-free Thymectomy • Before deciding about thymectomy, make sure that the patient has autoimmune MG • R/O: – – – – – LEMS Congenital myasthenic syndrome Botulism Neurasthenia Mitochondrial disease Thymectomy in MG • Indicated – Thymoma – Seropositive MG onset 15-50 years with moderate or severe disease “For patients with non-thymomatous autoimmune MG, thymectomy is recommended as an option to increase the probability of remission or improvement (class II evidence)” Thymectomy in MG • Not indicated – – – – Ocular MG MuSK-Positive MG Mild generalized non-thymomatous MG Late-onset non-thymomatous MG (> 50 or 60) • No effect of thymectomy • Titin and Ryanodine Ab positive cases even deteriorated • Controversial – Seronegative generalized MG – Generalized MG with good response to other treatment modalities • Wait a while before deciding for thymectomy but not too long • Before thymectomy, the patient has to be in a stable condition • If the patient is not thymectomized, F/U CT scan every 2 years • Any MG patient undergoing thoracotomy for other causes (e.g., CABG), should have thymus removed. Corticosteroids • Corticosteroid-related exacerbations in the first 2 weeks : 15-30% – Patients with weakness in bulbar and respiratory muscles need PE first • Some don’t tolerate alternate day regimen • Suboptimal response to steroid < 20% • Steroid dependency Cyclosporine • Response begins after 1-2 months • Contraindicated in renal impairment and uncontrolled hypertension • Important drug interactions – NSAIDs – Statins – ACE inhibitors Mycophenolate Mofetil (Cellcept) • Relatively safe drug but Good for MG or not? Azathioprine • Particularly used as a steroid-sparing agent • Active metabolite 6-mercaptopurine • Competes with hypoxanthine and inhibits DNA/RNA synthesis • Induces B and T-cell lymphopenia • 10% of population have genetically reduced activity of enzyme thiopurine methyltransferase (TPMT) • AZA metabolism is reduced vulnerable to myelosuppression • 1/300 have undetectable TPMT activity. AZA contraindicated • Important interaction with allopurinol – Increased toxicity and myelosuppression – Dose reduced to 25% Contraindications • Known hypersensitivity to azathioprine. • Pregnancy, except where benefit outweigh risk • Breastfeeding • Very low or absent TPMT activity • Dose adjustment needed with allopurinol • Malignancy. • Renal or hepatic insufficiency (relative contraindication Risks • • • • • • Cancer Infection Hypersensitivity reactions Megaloblastic changes, leukopenia Hepatotoxicity Acute pancreatitis Cancer • Risk of malignancy for treatment duration < 10 yrs is small • Lymphoma risk increased 4-fold or 1 case/1000 patient years • AML/ myelodysplasia rare • Increased risk of skin cancer – Skin protection with UVA blockers Infection • When used in combination with steroids, increased susceptibility to viral, bacterial and fungal infection • Live vaccines contraindicated • Diminished response to killed vaccines (e.g., Hepatitis B) Dosage • TPMT activity should be measured • Usual dosage 1-3 mg/kg • Slow onset of action – Wait several months, usually 4-6 but up to 18 months for response – Is a good choice when delayed response is acceptable • Start Prednisone + AZT in moderate to severe cases from the beginning • Weekly CBC, LFT for 4 weeks Mycophenolate Mofetil (Cellcept) Mycophenolate mofetil • Active metabolite: mycophenolic acid • Inhibits inosine monophosphate dehydrogenase and depletes guanine inhibition of DNA synthesis • lymphocyte selective immunosuppressive agent • Compared to AZA: – More selective- less adverse effects – Hepatotoxicity lower – Risk of lymphoma slightly higher Dosage • • • • • • Expensive drug 1-3 gr/day Usually effect starts in two months CBC, LFT, blood chemistry monitored Dose reduction in renal insufficiency Should not be taken with azathioprine Side effects • GI upset 20% • Hematologic < 5% – Anemia, leukopenia, thrombocytopenia – Usually mild, dose-dependent, reversible • Genitourinary symptoms – dysuria, urgency, frequency, sterile pyuria, hematuria • Hepatotoxicity, respiratory failure rare • Allergic reactions Infections • • • • In > 2 g/day CMV and other herpes family viruses Bacterial, fungal PML (10 confirmed, 7 possible) Cancer risk • Mainly in transplant patients receiving multiple immunosuppressives • Lymphoma • Solid organ tumors • Skin cancer • Pregnancy • FDA pregnancy category D • only use MMF in pregnant women if the potential benefit outweighs the potential risk to the fetus (e.g., transplant patients) • Fetal malformation in 4/15 live born infants • Breast feeding contraindicated Cyclosporine (Sandimmune, Neoral) Cyclosporine • First immunosuppressive drug found to act selectively on T cells • The helper T cell is the main target, but the T suppressor cell may also be affected • Cyclosporine inhibits calcineurin phosphorylase, block genes that transcript IL-2 that is required for T cell activation • Metabolites mainly excreted in bile Dosing • distribution of the drug is limited primarily to lean body mass in obese patients • Dosing should be based on ideal body weights and divided two times/day • Significant inter- and intra-individual variability in bioavailability (1-86%) • Significant variation in bioavailability between different brands. The same brand should be used • Serum concentration • Rapid onset of action (1-2 months) • Microemulsion formulation better absorbed (Neoral) • Higher serum concentration with empty stomach • Importance of taking cyclosporine consistently before or after meals Contraindications • • • • uncontrolled hypertension Significant renal impairment Serious infections Previous history of malignancy, excluding basal cell carcinoma • Pregnancy, breast feeding • Hepatic dysfunction Drug interactions with cyclosporine Drug interactions with cyclosporine Adverse effects • Renal dysfunction – Acute: usually transient on dose reduction – Chronic: Usually irreversible, increases with duration of treatment – Better to stop the drug in 1-2 years – If >30% Cr rise 25% dose 4 w if not corrected, 50% 4 w if not: stop and don’t re-start until normalized Adverse effects • Hypertension Cancer risk • • • • • Skin SCC Lymphoma Solid tumors Paraproteinemia Reduced risk of breast and colon CA Adverse effects • Neurologic: – – – – Tremor, paresthesia, headache Seizure: dose-dependent RPLS PML • Gingival hyperplasia • Hepatotoxicity Adverse effects • Infection: rare, may require dose • Hyperlipidemia: TG> Chol – Caution with statins. Risk of rabdomyolysis • • Vaccination • Live vaccines contraindicated • Response to killed vaccines reduced but still recommended( Influenza, Pneumococcal) • Pregnancy • • • • Category C drug in pregnancy No increase in teratogenicity (629 pregnancies) trends towards low birth weight and prematurity 16% incidence of mental developmental delay (175 children) attributed to premature birth • Excreted in breast milk Cyclophosphamide (Endoxan) Cyclophosphamide • Alkylating chemotherapeutic agent • Binds to DNA and interferes with mitosis and cell replication • Suppresses cell-mediated & humoral immunity through its actions on T cells and B cells • Alters T lymphocytes towards a less inflammatory phenotype • Good bioavailability within the CNS Side effects • • • • Alopecia nausea/vomiting Transient myelosuppression Hemorrhagic cystitis 4.5% • Fluid intake + Mesna • Pregnancy: contraindicated • Breast feeding: contraindicated • Bladder Cancer – 3-5% – Mean interval of 5.8 (3-10) years – Risk of malignancy related to the cumulative dose > 80 gr • Gonadotoxicity – Amenorrhea 33-44% • IM monthly GnRH resulted in restoration of normal ovarian cycle in > 93%of women – Azospermia • More when cumulative dose > 300mg/kg Dosage • Oral cyclophosphamide • Monthly IV pulse 700mg/m2 • Adjust next monthly dose on Nadir WBC (at mid-month) • High dose myeloablation (resetting) • 50 mg/kg/day for 4 days • Max lifetime dose < 80-100 gr Rituximab (RTX) • Monoclonal Ab that targets the trans -membrane protein CD20 of B-cells significant depletion of B-cells Neurological diseases with reported use of RTX • • • • • • • • • IgM mediated neuropathy Neuromyelitis optica Dermatomyositis Multiple sclerosis Multifocal motor neuropathy Myasthenia gravis CIDP Sjogren associated neuropathy Lambert- Eaton myasthenic syn. Protocols • • • • 375 mg/m2 x 4 (each week) 750 mg/m2 x 2 (2 weeks apart) Combining RTX with IVIG Marked B-cell depletion for 6-9 months, sometimes up to 2 years • Should not be used with other immunosuppressive especially T-cell depletors Safety • Overall safe • Infusion related reactions in 84% – Minor in 97% – nausea, headache, fatigue, rash, and flulike symptoms, orthostatic hypotension – Pre-treatment with acetaminophen, steroid, and antihistamine recommended – Most severe after the first infusion • RTX associated infections 30% – Usually mild – Only 1-2% severe/ life threatening • Risk of PML