* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download C. parvum
Survey
Document related concepts
Transcript
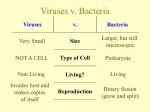
AIDS and Opportunistic Infections April 13, 2010 Silvia N. J. Moreno History of AIDS • 1981: PCP and Kaposi’s sarcoma reported by doctors in NY and Los Angeles. CDC reports in MMW a strange killer pneumonia spreading among gay men. Is was designated as GRID (Gay-Related Immune Deficiency). • 1982-1985: Cases of AIDS in 1982 began to be reported by fourteen nations. In 1982 CDC received its first report of "AIDS in a person with hemophilia (from a blood transfusion), and in infants born to mothers with AIDS.” • 1983: Dr. Montagnier announced the isolation of LAV retrovirus (lymphadenopathy-associated virus), which later was identified as the cause of AIDS. 33 countries reported cases. • 1984: Dr. Robert Gallo of the NCI isolated HTLV-III retrovirus ( Human T-cell lymphotropic virus III). It was later determined that LAV and HTLV-III were the same virus • 1985: AIDS awareness was brought to the public's consciousness, Rock Hudson, died of AIDS shortly after making it public thus becoming the first major public figure to announce that he had AIDS. An HIV blood test was brought to large companies to make it available in large scale. History of AIDS • 1986: President Reagan makes his first mention of the word “AIDS” publicly and request the Surgeon General C. Everett Koop to prepare a report which was released in October 1986. He followed with a brochure: “Understanding AIDS” that was sent to 107 million households. It warned that “AIDS is one of the most serious health problems that has ever faced the American public”. It discussed risk behaviors. • 1987: AZT (also known as Retrovir®, zidovudine, or ZDV) -- GlaxoSmithKline -- became the first anti-HIV drug (a Nucleoside Reverse Transcriptase Inhibitor) approved by the FDA. Reverse transcriptase is the enzyme that HIV uses to make a DNA copy of its RNA. This is necessary for the production of the viral double-stranded DNA which is integrated into the genetic material of the infected cell. AZT is used in combination with at least two other anti-HIV drugs. History of AIDS • 1987: A touch of a Princess: On March 20, 1987 princess Diana changed the public perception of AIDS at the opening of a special ward at London’s Middlesex Hospital. She was seen not wearing gloves and shaking hands with people with AIDS. 1990: Death of Ryan White, a nineteen year old, white, heterosexual, teenager from Indiana died because of AIDS which he contracted from blood products, as part of his treatment for hemophilia. • In August of 1990, President George H.W. Bush signed the the Ryan White Comprehensive AIDS Resources Emergency (CARE) Act into law. • The bill authorized $881 million in relief funds to the 16 cities hardest hit by the epidemic. Congress only appropriated $350 million. • President Bush also signed the Americans with Disabilities Act (ADA) in 1990 to protect people with HIV/AIDS from discrimination. History of AIDS 1999: Origin of HIV-1 Discovered. A research team from UAB lead by Dr Beatrice Hahn identified a subspecies of chimpanzee (Pan troglodytes troglodytes) native to West-Central Africa as the natural reservoir for HIV-1. Viruses related to HIV-1 had previously been found in chimpanzees and were given the designation SIVcpz (for Simian Immunodeficiency Virus). P. T. troglodytes has been the source of three independent cross-species transmission events. Both HIV-1 (chimpanzees) and HIV-2 (sooty mangabeys) originated in Africa. Why the epidemic arose in the mid-20th century is not clear. People in some African nations contract the virus by eating 'bushmeat' Pan troglodytes sub-especies and distribution 1. Pan troglodytes verus 2. P. t. vellerosus 3. P. t. troglodytes 4. P. t. schweinfurthii The Nobel Prize in Physiology or Medicine for 2008 with one half to Harald zur Hausen for his discovery of “human papilloma viruses causing cervical cancer” and the other half jointly to Françoise Barré-Sinoussi and Luc Montagnier for their discovery of “human immunodeficiency virus.” Four's a crowd. The Nobel Assembly surprised many by not sharing the award with pioneering AIDS researcher Robert Gallo. Global summary of the AIDS epidemic, December 2008 Number of people living with HIV in 2008 Total Adults Women Children under 15 years 34.4 million [31.1 – 35.8 million] 31.3 million [29.2 – 33.7 million] 15.7 million [14.2 – 17.2 million] 2.1 million [1.2 – 2.49 million] People newly infected with HIV in 2008 Total Adults Children under 15 years 2.7 million [2.4 – 3.0 million] 2.3 million [2.0 – 2.5 million] 430 000 [240 000 – 610 000] AIDS deaths in 2008 Total Adults Children under 15 years 2.0 million [1.7 – 2.4 million] 1.7 million [1.4 – 2.1 million] 280 000 [150 000 – 410 000] At the end of 2007, the CDC estimates that there were 571,378 people living with HIV/AIDS in the 39 states and dependent areas that have a history of confidential name-based HIV reporting, based on reported diagnoses and deaths. However, the total number of people living in the USA with HIV/AIDS is thought to be around 1.1 million. HIV infection and AIDS • AIDS is caused by Human Immunodeficiency Virus (HIV) which is found in all cases of the disease. • The primary targets of HIV are activated CD4+ T4 helper lymphocytes but the virus can also infect several other cell types including macrophages. It is the loss of T4 helper lymphocytes that leads to immunosuppression in the patient and the consequent opportunistic infections. • HIV is a lentivirus (slow virus), a class of retrovirus. These viruses take a long time to cause overt disease. • Most lentiviruses target cells of the immune system so disease is manifested as immunodeficiency. Life-cycle of HIV-1 • The cell primary receptor is the CD4 molecule. • Entry into the cytoplasm initiates the disassemble of the HIV core. • The uncoated HIV-1 reverse transcribes its genomic RNA in the cytoplasm into a DNA copy which is transported into the nucleus for integration into host chromosomes. • The provirus is transcribed by the cell’s RNA polymerase II machinery. • Viral mRNA enters the cytoplasm and uses the host's cellular machinery to manufacture virus proteins. • The viral components then gather at the cell membrane and immature viruses bud off the cell. • Core proteins are produced as part of long polypeptides, which must be cut into smaller fragments by a protease to form functional proteins. Figure 1 from BMC Medicine 2008, 6:31 What are the symptoms of AIDS? Early symptoms Some people have flu like illness within a month or two after exposure to the virus They may have fever, headache, malaise and enlarged lymph nodes These symptoms usually disappear within a week More persistent and severe symptoms may not surface for a decade or more after HIV first enters the body in adults: Diarrhea for more than one month Dry mouth and skin rushes Severe headache Dry cough AIDS: this term applies to the most advanced stages of HIV infection. All HIV-infected people who have fewer than 200 CD4+ T cells Opportunistic Infections Most AIDS-defining conditions are opportunistic infections, which rarely cause harm in healthy individuals. In people with AIDS, these infections are often severe Bacteria: • Mycobacterium Avium Complex • Mycobacterium Tuberculosis Viruses: • Varicella-Zoster Virus • Herpes Simplex Virus • Cytomegalovirus Protozoa: • Coccidiosis (Cryptosporidiosis, Cyclosporiasis, and Isosporiasis) • Toxoplasmosis • Leishmaniasis (not in the U.S., but in Southern Europe and in many other parts of the world) • Chagas • Malaria Fungi: • Pneumocystis carinii Pneumonia • Candidiasis • Aspergillosis • Cryptococcosis • Histoplasmosis • Coccidioidomycosis • Microsporidiosis Opportunistic Infections Why do AIDS patients show infections with a special set of (opportunistic) pathogens? What do the AIDS associated infections share? • Usually benign but persistent infections • Protection against the disease is mediated by the cellular arm of the immune system • No vaccination AIDS treatment Antiretroviral treatment: more than 20 drugs approved. HAART: highly active antiretroviral Therapy combines three or more anti-HIV medications daily. Anti-HIV medications do not cure HIV infection. Four classes of Anti-HIV drugs approved by the U.S. Food and Drug Administration (FDA): 1. Non-nucleoside Reverse Transcriptase Inhibitors (NNRTIs):Efavirenz (Sustiva) binds to and block the action of reverse transcriptase. 2. Nucleoside Reverse Transcriptase Inhibitors (NRTIs): zidovudine (Retrovir), tenofovir DF (Viread), and stavudine (Zerit), are nucleotide analogues. They inhibit reproduction of the virus. 3. Protease Inhibitors (PIs): lopinavir/ritonavir (Kaletra) 4. Fusion Inhibitors: enfuvirtide (Fuzeon), are newer treatments that work by blocking HIV entry into cells Core proteins of HIV-1 are produced as part of long polypeptides that are cut into smaller pieces by protease to create functional and mature proteins. Protease inhibitors bind to the active site, where protein cleavage occurs. With the inhibition of protease, new viral particles cannot mature and do not become infectious. This figure is Fig. 3 from Nature Medicine, 2003, 9:867 HAART resulted in further declines in rates of PCP and other opportunistic infections Yearly opportunistic infection rates per 1,000 person-years, CDC Adult and Adolescent Spectrum of Disease Project, 1994–2001. CMV, cytomegalovirus; HAART, highly active antiretroviral therapy; KS, Kaposi's sarcoma; MAC, Mycobacterium avium complex; PCP, Pneumocystis pneumonia. Data are standardized to the population of AIDS cases reported nationally in the same year by age, sex, race, HIV exposure mode, country of origin, and CD4+ lymphocyte count. Emerging Inf. Dis. 10:1713 Opportunistic infections: Pneumocystis carinii • First identified in 1909 in a They can be stained by a number of tissue stains, like this silver stain showing the typical black cup-shaped appearance makes them stand out against a paler background. trypanosome-infected animal lung • Was long thought to be a protozoan but molecular phylogeny identifies it as fungus • The number of cases exploded in the 1980s as PCP became one of the hallmark manifestations of AIDS • Ubiquitous organism in the environment • Most important transmission route is airborne • Subclinical infection during childhood which is usually well contained Cases of PCP reported to the CDC in the pre-AIDS era compared with the AIDS era. Horizontal bars at the top indicate the period during which prophylaxis to prevent PCP and HAART were available. The arrow indicates the time of publication of guidelines by the US Public Health Service for prevention of PCP in (HIV)–infected patients. JAMA 2001, Vol. 286:2450 Pneumocystis pneumonia Chest radiograph of a patient with PCP demonstrating diffuse bilateral infiltrates. JAMA 2001, Vol. 286:2450 • P. carinni causes clinically apparent Hematoxylin-eosin–stained section of lung from an HIVinfected patient with PCP. An acellular eosinophilic exudate characteristic of PCP can be seen filling the alveoli. JAMA 2001, Vol. 286:2450 Detection of human-derived P carinii by immunofluorescence using monoclonal antibodies. JAMA 2001, Vol. 286:2450 pneumonia virtually exclusively in immunosuppresed patiens. • Seen in patients with CD4 counts below 200 • Fever, nonproductive cough, chest tightness, shortness of breath • Diagnosis by x-ray (but 20% undetected), or better by detection of organisms in induced sputum or bronchial lavage • Chemoprophylaxis has been successful. Sulfa drugs for treatment and prophylaxis Cell Biology of Pneumocystis carinii Electron micrograph illustrates both cysts (white arrowheads) and trophozoites (black arrowheads). • Four morphological forms: trophozoites, cysts, precysts, and sporozoites (intracysts bodies). Kovacs, J. A. et al. JAMA 2001;286:2450-2460. • Trophozoites are pleomorphic and form clusters. Their cytoplasm is poor in organelles. • Trophozoites interact with the surface of pneumocytes. Attachment to host cells is required for survival. • The cyst is the diagnostic form. Copyright restrictions may apply. Thin section showing several trophozoites. A thick surface coat is evident, especially in cross sections of the surface projections (arrows). N, nucleus; T, trophozoite. Bar = 200 nm. Mem. Inst. Osw. Cruz 100: 903 Cryptosporidia and cryptosporidiosis • Apicomplexan parasite described in 1907 by Tyzzer in gastric gland of mice Cryptosporidia (hidden sporocst) • Pathogenic significance unclear until 1955-Slavin described infection in turkeys (C. meleagridis) • Low mortality but severe diarrhea • 1970s infections in intestines of calves • 1976 infections reported in two human patients-severe watery diarrhea • 1982-present-mortalities in AIDS patients and worldwide infections in both immunocompromised and immunocompetent people Milwaukee skyline 1993 • C. parvum has caused a series of massive waterborne outbreaks in the US • Infection with C. parvum results in severe diarrhea, which can be lifethreatening in AIDS patients and malnourished children C. parvum has high attack rates Year Location People exposed People infected Cause 1984 Braun Station, TX 5900 2006 Sewage contaminated well 1987 Carrollton, GA 32,400 12,960 Treatment deficiencies 1991 PA NA 551 Treatment deficiencies 1992 Jackson, OR 160,000 15,000 Treatment deficiencies 1993 Milwaukee, WI 1,600,000 403,000 Treatment deficiencies Cryptosporidium parvum life cycle Oocysts excyst in the intestine releasing sporozoites. Sporozoites attach to epithelial cells where they become enclosed within a PV. Zygote undergo asexual development producing a sporulated oocyst with 4 sporozoites. Most oocysts are thick walled and are excreted with feces. Some are thin-walled and excyst within the same host. Trophozoites undergo asexual reproduction by merogony (endopolygeny). Monoxenous life cycle: all stages (asexual and sexual) occur within one host. Two types of meronts: Type I meront form 8 merozoites released from the PV when mature. Type II meront form 4 merozoites which do not undergo further merogony but produce sexual stages (microgamont and macrogamont) Cryptosporidium parvum Electron microscopy shows their intracellular but extra-cytoplasmic location within parasitophorous vacuoles formed by a continuous covering of microvillous membranes. El: attachment zone; Fo: feeder organelle; Ec: electron dense collar; Fl: fibrous layer of the attachment organelle; Pv: parasitophorous vacuole Transmission electron micrographs showing the invasion process of C. parvum into the host cell. C. parvum attaches to a host cell. The microvilli of the host cell elongate along both sides of the parasite (arrows). A dense band (DB) is found under the host cell membrane. From J. Parasitol. 2005, 91:1034 C. parvum is completely covered with the membrane derived from the microvilli. Each parasite is in a parasitophorous vacuole (PV) formed by the microvilli. Membranes surrounding the parasites are composed of double layers. The microvilli (MV) between 2 parasites show remarkable elongation. DB, dense band. From J. Parasitol. 2005, 91:1034 Cryptosporidium induces actin polymerization in the host cell Filamentous actin is found directly under the site of parasite infection. Figure 1 from Infect. Immun. 2000, 68:2315 • As we have seen before T. gondii invasion depends only on parasite actin (there is no difference in infection rate between normal host cells and those with reduced actin polymerization (SCARWA) • For Cryptosporidium however there is clear dependence on host actin Cryptosporidium parvum Oocysts: Lb: lipid body; Ow: oocyst wall; Pv: parasitophorous vacuole; Sp: sporozoite; fo: deeder organelle; Clinical symptoms • Incubation period: 2-14 days • Watery and profuse diarrhea, abdominal cramps, nausea, vomiting, weight loss and low-grade fever. • Self-limited disease in immuno-competent individuals • Prolonged duration in immuno-compromised host. Degree of immunodeficiency correlates with severity: – Self-resolving disease – Chronic diarrhea over months (<50 CD4 count) – Fulminate diarrhea • Malabsorption can contribute to the wasting syndrome in AIDS patients. • Bile duct infection can produce jaundice. Prevalence: Non-AIDS: 4.9% (developed countries); 7.9% (underdeveloped countries) AIDS: 14% (developed countries); 24% (Underdeveloped countries. Mortality: 80% Pathogenesis Histopathological changes: relatively nonspecific Enteric infections: • mild to severe villous atrophy • increased crypt size • inflammation: cellular infiltrated in lamina propria (neutrophils and plasma cells; occasionally macrophages and lymphocytes) Respiratory infections: • Cellular infiltrates with neutrophils and plasma cells in the subepithelial lamina propria together with deciliation, hyperplasty or hyperthrophy of the respiratory epithelium In histological sections parasite appears as small basophilic bodies apparently attached to the surface of the cells, sometimes giving the microvillous brush border a spotted granular appearance DIAGNOSIS • Detection of endogenous developmental stages: Most stages are basophilic and stain well with hematoxylin and eosin or giemsa stains. • TEM helps to confirm the identity of the organisms • Scanning electron microscopy may be used to confirm infections. • Finding oocyst in fecal material. Other body fluids such as bile, sputum, respiratory aspirates may be examined • Immunolabeling techniques have been developed to detect oocysts. Concentration procedures to improve sensitivity: centrifugation, filtration. • Immunoserology: specific antibodies against C. parvum The modified acid-fast methods produce bright red oocysts against a background of blue-green fecal debris and yeasts Oocysts of Cryptosporidium parvum labeled in an indirect immunofluorescence assay (IFA) with monoclonal antibody 8F4 to the inner oocyst wall. The IFA is still the most commonly used technique to assay for oocysts in environmental samples. Metabolic differences with other apicomplexan parasites • • • • Cryptosporidium is quite divergent from the other Apicomplexa It lacks a plastid It has a highly simplified mitochondrion which does no longer perform oxidative phosphorylation It has lost many of its biosynthetic enzyme genes and depends almost completely of host cell derived nutrients Chemotherapy of cryptosporidiosis Latest drug to be used- a nitrothiazole benzamide with broad antimicrobial spectrum Parasite is highly resistant to chemotherapy Drugs with modest activity: Paramomycin, nitaxosanide Chemical structures for nitazoxanide (a) and its first metabolite in human plasma, tizoxanide (b) Giles et al., Trends in Parasitology, 18, 95-97, 2002.. Cryptosporidium is highly drug resistant Drugs with broad activity against apicomplexans that fail in C. parvum: • Antifolates (pyrimethamnine, sulfonamides) • Macrolide antibiotics (clyndamycin, azithromycin) • Atovaquone Drugs with modest activity: • Paramomycin, nitaxosanide Two possible explanations for the drug resistance: 1) Drugs do not reach the parasite because it lives in a specialized compartment 2) The drugs used against other Apicomplexa are metabolically inappropriate Cryptosporidium parvum transmission Fecal-oral spread of oocysts Fecal contamination of drinking water sources is an important vehicle for transmission of oocyst. Also contamination of recreational water Large scale outbreaks have been associated with contamination of community drinking water Zoonotic transmission: General lack of host specificity of C. parvum: animal-to-human or animal-to-animal. Bovine genotype (gt II). Contaminated food: unpasteurized milk, offal and sausages, foods prepared in untreated water or foods grown in soil fertilized in animal/human waste Person-to-person through direct or indirect contact, possibly including sexual activities. Human genotype of C. parvum (C. hominis) Prevention and control Hygiene/disinfection-prevention of oocyst transmission-difficult • Oocyst very stable in aqueous solution; 3 months at 20oC and 1 year at 46oC • Infectivity lost upon heating (65oC, 30 min) or desiccated for 4h or snap freezing • Disinfecting agents-only 5 effective over short exposure periods • 50% ammonia (30 min, 25oC) • 288 mg/ml hydrogen peroxide (30 min) • 10% formalin 1-7 days (< 87%) • Glutaraldehyde (2%, 30 min, 37oC) • Exspor (chlorine dioxide-based sterilant-Alcide Co)- 30 min, 22 oC • Oocide (two phase product producing ammoniaAntec Int. Ltd.)- 5%, 30 min, 22 oC • Oozone (especially for water treatment- 2.5 mg/ml at 22 oC) CYCLOSPOROSIS and RASPBERRIES ATLANTA-Guatemalan raspberries have been fingered as the delectable vehicle of this springユs outbreaks of Cyclospora cayetanensis. And while the epidemiologic links to the caviar of fruit accumulated, a cousin berry was exonerated. Despite much scuttlebutt, the strawberry got a clean bill of health…. Multiple foodborne outbreaks, thousands in US and Canada since 1990: Before 1996: mostly overseas and 3 small US outbreaks May 1996: 55 events (all had raspberries served) of outbreaks in US and Canada 1465 cases, 978 confirmed. Spring 1997: 41 events, 1012 cases. Again the only common food consumed in all events was raspberries from Guatemala May 1998: Ontario, Canada, 315 cases Cyclospora cayetanesis • Countries initially identified as having endemic cyclosporiasis: Haiti, Guatemala, Peru and Nepal • Infection most common in HIV/AIDS patients. • Also important in travelers • Large, multi-state food-borne outbreaks of Cyclospora infection in the USA and Canada during the 1990s. • Cyclospora infects enterocytes of the small bowel. • The main symptom is watery diarrhea, loss of appetite, weight loss, abdominal bloating and cramping, nausea, fatigue and low grade fever. • In the immunocompromised patient, severe diarrhea can last up to 4 months or longer even if treated thus producing a disease syndrome that is debilitating and life threatening • Extra-intestinal infection appears to be more common in AIDS patients Duodenal biopsy showing immature schizonts (broad arrow) and merozoites (arrow) in a parasitophorous vacuole of C. cahetanesis in surface enterocytes. (HE STAIN) Cyclospora cayetanesis life cycle • The oocyst is passed in stools but is not infective. • Sporulation occurs after days or weeks (22°C to 32°C), to form two sporocysts, each containing two sporozoites. • Fresh produce and water can serve as vehicles for transmission and the sporulated oocysts are ingested. • The oocysts excyst in the gastrointestinal tract, releasing sporozoites which invade the epithelial cells of the small intestine. Inside the cells they undergo asexual multiplication and sexual development to mature into oocysts, which will be shed in stools. The relative sizes of various microbes. Giardia lamblia cyst (length from 8 to 19 and averages 11-12 ), a Cyclospora cayetanensis oocyst (8-10 ), and a Cryptosporidium parvum oocyst (4.5 × 5 ). The virus is not drawn to scale. The Cyclospora oocyst shown is fully sporulated it has 2 internal sporocysts, each with 2 sporozoites. Whereas oocysts of Cryptosporidium, are fully sporulated and infectious when excreted, Cyclospora oocysts sporulate in the environment, days to weeks after excretion. Giardia, which is not a coccidian parasite, does not have sporocysts or sporozoites. (Figure courtesy of Dennis D. Juranek.) EPIDEMIOLOGICAL DATA • Co-infection with leishmaniasis and HIV has been reported in 34 countries in Africa, Asia, Europe, and South America. The impact of this health problem is increasingly severe. • In southern Europe, up to 70% of adult cases of visceral leishmaniasis are associated with HIV infection. • Users of injecting drugs are the most seriously affected group. Analysis of trends is facilitated by use of a geographical information system to map and monitor patterns of co-infection. Source:Communicable Disease Surveillance and response.Who http://www.lynx.who.ch/ctd/html/leisepidat.html LEISHMANIASIS-HIV Leishmania/HIV co-infection is emerging as a new disease: • Important epidemiological changes: Humans become reservoirs: Co-infected patients harbor a high number of Leishmania in their blood. This increases the risk of future epidemics. • Atypical manifestations of Leishmaniasis: Leishmania/HIV coinfections modify the traditional patterns of zoonotic VL. VL is the clinical form most frequently associated with HIV/AIDS specially in south-western Europe (some CL have been reported): The geographical distribution of VL and AIDS is increasing because: • the spread of AIDS in suburban and rural areas of the world, • the spread of VL from rural to suburban areas. • In southwestern Europe up to 70% of all adult cases of VL are related to HIV/AIDS. • While the incidence of leishmania/HIV co-infection is increasing en eastern Africa and India, the incidence in Europe has diminished thanks to HAART. TRANSMISSION The diagram suggests a few possible paths of leishmaniasis infection. Female sandflies, vectors for parasites of the genus Leishmania, disseminate to humans mainly from animals. Infected dogs, both symptomatic and asymptomatic, have traditionally been reported to be the reservoir of this disease; foxes, jackals, wolves, raccoons, sloths, hyraxes, rats, and other rodents have been reported as reservoirs. In HIV-Leishmania coinfection, intravenous drug users seem to be human reservoirs. Reports of transmission of leishmaniasis via needle-sharing are increasing. LEISHMANIA/HIV CO-INFECTION • Among immunosuppressed individuals quickly evolve to a full clinical presentation of severe leishmaniasis. • VL quickly accelerates the onset of AIDS and shortens the life expectancy of HIV-infected people. • HIV spurs the spread of VL. AIDS increases the risk of VL by 1001000 times in endemic areas. HIV infection reactivates latent leishmaniasis. • This combination produces cumulative deficiency of the immune response because Leishmania parasites and HIV destroy the same cells, increasing disease severity and consequences. Leishmania and HIV invade and replicate in macrophages. • VL is considered a major contributor to a fatal outcome in co-infected patients. • Leishmaniasis can be transmitted directly person to person through the sharing of needles, as is the case among intravenous drug users. HIV modifies the clinical presentation of leishmaniasis in the co-infected patient Major characteristics for HIV-associated leishmaniasis, all related to the immunologic impairment caused by the virus: (1) Parasitic dissemination, to the skin in DCL, or throughout the reticuloendothelial system in visceral and visceralizing syndromes (2) Atypical locations (3) Chronic and relapsing course, with each patient typically experiencing two or three relapses despite proper treatment (4) Poor response to standard therapy. General treatment of leishmaniasis is indicated for each clinical presentation, although localized cutaneous lesions may benefit from topical and/or intralesional therapy as well.