* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download PM_HEMODYNAMIC_DYSFUNCTION
Survey
Document related concepts
Transcript
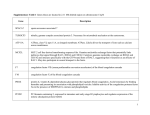
HEMODYNAMIC DYSFUNCTION May 19, 2008 Pathophysiology Premed 2 Dr. ROOPA FLUID DISTRIBUTION 60% of lean body weight is water -2/3 is intracellular -1/3 is extracellular 5% of total body water is in blood plasma DEFINITION OF TERMS Hemmorhage: escape of blood from the vessels -surrounding tissues -body cavity -outside of the body HEMATOMA: THE TISSUE BLOOD TRAPPED WITHIN Hemopericardium Hemoperitoneum Petechiae Purpura Ecchymosis A petechia (pronounced plural petechiae is a small (1-2mm) red or purple spot on the body, caused by a minor hemorrhage (broken capillary blood vessels Purpura (from the Latin, purpura, meaning "purple") is the appearance of red or purple discolorations on the skin that do not blanch on applying pressure. They are caused by bleeding underneath the skin. Purpura measure 0.3-1 cm, whereas petechiae measure less than 3 mm, and ecchymoses greater than 1 cm.[1] An ecchymosis is a spot caused by loss of blood from a vessel. It implies a larger size than a petechia.[1] It has a more diffuse border than purpura.[2] It can be caused by a bruise (which implies trauma), but can also be caused by bleeding diathesis.[ Ecchymosis: The skin discoloration caused by the escape of blood into the tissues from ruptured blood vessels. Ecchymoses can similarly occur in mucous membranes as, for example, in the mouth. INFARCTION An infarction is the process of tissue death caused by blockage of the tissues blood supply.The supplying artery may be blocked by an obstruction. Types: 1. anemic/ white/ pale infarcts - arterial occlusion - heart, spleen and kidney 2. hemorrhagic / red infarct - venous occlusion -intestines and lungs -areas with redundant blood supply NORMAL HEMOSTASIS A well regulated process maintains blood in a fluid, clot free state in normal vessels induces the rapid formation of a localized hemostatic plug at the site of vascular injury NORMAL SEQUENCES OF HEMOSTASIS 1. Arteriolar vasoconstriction 2. Exposure of subendothelial ECM when there is endothelial injury 3. Tissue factor released at site of injury 4. Formation of permanent plug THROMBOSIS Blood coagulates inside the blood vessels Interruption of blood flow Predisposing factors: smoking OCP immobilization sickle cell disease polycythemia cancer congestive heart failure THROMBOGENESIS Formation of a thrombus Depends on: 1. platelets 2. endothelial cells 3. coagulation cascade PLATELET PLUG Injury to the blood vessel exposes collagen in the vessel wall Von Willebrand factor allows the platelets to adhere Conformational change in the platelets Activation of the coagulation cascade Also, formation of TxA2: constricts blood vessels, platelets aggregate Von Willebrand factor (vWF) is a blood glycoprotein involved in hemostasis. PLATELET PLUG Fibrinogen links strengthen the plug Fibrin formation occurs Prostacyclin is secreted by endothelial cells; limit the plug COAGULATION CASCADE 2 pathways. Intrinsic pathway(contact activation pathway) Extrinsic pathway(tissue factor pathway) Lead to fibrin formation Extrinsic pathway -initiated by tissue factor -final product: formation of fibrin -prothrombin time -factors II, V, VII and X -fibrinogen COAGULATION CASCADE Intrinsic pathway Involves all the clotting factors except VII and XIII Involves contact activation with: -Hageman factor (factor XII) -prekallikrein -high molecular weight kininogen(HMWK) -factor XI THROMBOTIC DISORDERS Hereditary thrombophilia Antiphospholipid antibody syndrome Disseminated intravascular coagulopathy HEREDITARY THROMBOPHILIA Adolescents, young women Recurrent venous thrombosis Thromboembolism Deficiency: antithrombin III protein S protein C Most frequent cause: Factor V Leiden DISSEMINATED INTRAVASCULAR COAGULATION Is a pathological activation of coagulation mechanisms that happens in response to a variety of diseases. Consumption of platelets and coagulation factors Widespread thrombosis and hemorrhage Disseminated intravascular coagulation (DIC), is a pathological activation of coagulation (blood clotting) mechanisms that happens in response to a variety of diseases. As its name suggests, it leads to the formation of small blood clots inside the blood vessels throughout the body.[1] As the small clots consume all the available coagulation proteins and platelets, normal coagulation is disrupted and abnormal bleeding occurs from the skin critically ill, and may participate in the development of multiple organ failure, which may lead to death.[4] KINDS OF THROMBI Arterial thrombi -areas with active blood flow -lines of Zahn Lines of Zahn are a characteristic of thrombi[1] that appear when formed in the heart or aorta. They have visible and microscopic laminations produced by alternating pale layers of platelets mixed with fibrin and darker layer containing red blood cells. Their presence implies thrombosis at a site of rapid blood flow. In veins or smaller arteries, where flow is not as constant, they are less apparent VENOUS THROMBI Areas with less blood flow Veins of lower extremities Venous stasis Dark red; no lines of Zahn EMBOLISM In medicine, an embolism (plural embolisms) occurs when an object migrates from one part of the body (through circulation) and causes a blockage (occlusion) of a blood vessel in another part of the body. PULMONARY EMBOLISM Sudden death Immobilized patients, heart disease (CHF) Saddle emboli: bifurcation of the pulmonary artery Leads to pulmonary infarcts ARTERIAL EMBOLI 1. 2. 3. Originates from a mural thrombus Left atrium: mitral stenosis Left ventricle: Myocardial infarction Sites of arrest: Middle cerebral artery: most common Mesenteric arteries Renal arteries PARADOXICAL EMBOLI Emboli comes from venous side Passes though right-to –left shunt atrial septal defect patent foramen ovale Reaches arterial circulation OTHER FORMS OF EMBOLI Fat emboli: bone marrow particles; fractures -go to brain, lungs, kidney -fat embolism syndrome: difficulty breathing petechiae neurologic manifestations Air emboli: air goes into the blood vessels -trauma to the chest; abortion -decompression sickness: “the bends” or muscle pains -caissons disease: infarcts in the CNS, bones, tissues -due to nitrogen bubbles in the blood Amniotic fluid embolism: amniotic fluid in the blood -can lead to DIC, death EDEMA Abnormal fluid in the interstitial tissues spaces or body cavities Caused by: -increased hydrostatic pressure right sided heart failure: peripheral edema left sided heart failure: pulmonary edema EDEMA Causes: -increased capilary permeability -decreased oncotic pressure -increased sodium retention -blocked lymphatics TYPES OF EDEMA Anasarca: generalized form Hydrothorax Hydropericardium Hydroperitoneum (ascites) Transudate -non inflammatory -abnormal hyrdostatic or osmotic pressure -low protein -sp.gr. < 1.012 -high glucose Exudate -inflammation -increased vascular permeability -high protein content -sp.gr. >1.020 -many WBC -low glucose SHOCK Circulatory collapse Hypoperfusion Decreased oxygenation of tissues Caused by: -decreased cardiac output -widespread peripheral vasodilatation Organ most affected: kidney -acute tubular necrosis TYPES OF SHOCK Hypovolemic shock -loss in blood volume -massive hemorrhage -burns -vomiting, diarrhea Cardiogenic shock -massive MI -pump failure of the left ventricle Septic shock -bacterial infections; endotexemia Neurogenic shock -severe trauma -peripheral vasodilatation STAGES OF SHOCK 1. nonprogressive (early stage) -compensatory mechanisms -increased heart rate; increased peripheral resistance 2. progressive stage -compensatory mechanisms not adequate -tissue hypoperfusion -circulatory and metabolic imbalance 3. Irreversible stage -organ damage -metabolic imbalance -death