* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Slide 1 - World Allergy Organization
Survey
Document related concepts
Transcript
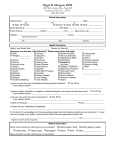
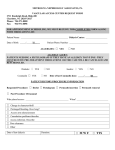
GLORIA Module 11: Drug Allergy (Part 1) Definition, Epidemiology and Pathogenesis of Drug Allergy an educational program of Updated: June 2011 Sponsored by an unrestricted educational grant from Global Resources in Allergy (GLORIA™) Global Resources In Allergy (GLORIA™) is the flagship program of the World Allergy Organization (WAO). Its curriculum educates medical professionals worldwide through regional and national presentations and local training programs. GLORIA modules are created from established guidelines and recommendations to address different aspects of allergy-related patient care. US GLORIA Program In conjunction with the American College of Allergy, Asthma and Immunology (ACAAI), GLORIA is now presented for CME Credit in the US to Regional, State and Local Societies. The GLORIA educational materials are available for download on WAO’s website www.worldallergy.org/gloria World Allergy Organization (WAO) The World Allergy Organization is an international coalition of 89 regional and national allergy and clinical immunology societies. WAO’s Mission WAO’s mission is to be a global resource and advocate in the field of allergy, advancing excellence in clinical care, education, research and training through a world-wide alliance of allergy and clinical immunology societies GLORIA MODULE 11: Drug Allergy (Part 1) Definition, Epidemiology and Pathogeneses of Drug Allergy Authors Werner Pichler, Switzerland Bernard Thong, Singapore Learning Objectives • Understand the difference between – Adverse drug reaction – Drug hypersensitivity – Drug allergy • Understand the epidemiology and risk factors for drug allergy • Understand the pathogenesis and immunological mechanisms underlying the different phenotypes of drug allergy Drug related side effects • Potentially dangerous – 4th leading cause of death in the USA Lazaru J. et al. JAMA (1998) 279: 200-205) • Altogether frequent – but rare for each drug • Very heterogeneous clinical symptoms – affecting quasi all organs – often mild, sometimes life threatening Classification of adverse drug reactions • Type A: predictable; strictly dose dependent – 80% of all side effects – Pharmacological side effects (e.g. gastrointestinal bleeding under treatment with NSAID) • Type B: not predictable; usually not dose dependent, and sometimes reactions to very small amounts – – – – 15-20% of all side effects Immunologic/allergic Non-immune mediated, “pseudoallergic” Idiosyncratic Nomenclature • Immune mediated drug hypersensitivity (drug allergy) – Clinical symptoms due to different types of specific immune reactions (T-cell & B-cell/Ig mediated) • Non immune mediated drug hypersensitivity (non-allergic drug hypersensitivity) – Symptoms and signs similar to immune mediated hypersensitivity, but failure to demonstrate a specific immune process to the drug – Older term: “pseudoallergy” • Idiosyncrasy – symptoms and signs due to some genetic alterations, e.g. an enzyme deficiency: e.g. hemolytic anaemia due to certain drugs in patients with G-6P-deficiency Johansson SGO, Bieber T, Dahl R, Friedmann PS, Lanier BQ, Lockey RF, et al. Revised nomenclature for allergy for global use: Report of the Nomenclature Review Committee of the World Allergy Organization, October 2003. J Allergy Clin Immunol 2004;113:832-6 Nomenclature Drug hypersensitivity Drug allergy IgE-mediated drug allergy Non-allergic hypersensitivity Non IgE mediated drug allergy eg: Non-specific histamine release, Arachidonic acid pathway activation, Bradykinin pathway alteration, Complement activation Johansson SGO, Bieber T, Dahl R, Friedmann PS, Lanier BQ, Lockey RF, et al. Revised nomenclature for allergy for global use: Report of the Nomenclature Review Committee of the World Allergy Organization, October 2003. J Allergy Clin Immunol 2004;113:832-6 Epidemiology • Adverse drug reactions (ADRs) have been reported to account for 3 to 6% of all hospital admissions and occur in 10 to 15% of hospitalized patients. • Drug allergy has been estimated to account for up to a third of all ADRs. • Most epidemiologic studies have dealt with ADRs or adverse drug events, with few focusing on drug allergy alone. • In hospitalized patients, the incidence of cutaneous allergic reactions from the rates of hospitalization for ADRs, disclosed an estimated rate of 2.2 per 100 patients and 3 per 1,000 courses of drug therapy. • The true incidence of drug-induced anaphylaxis is also unknown, as most studies have been based on all causes of anaphylaxis or all causes (both allergic and nonallergic) of ADRs. • The estimated incidence of Stevens-Johnson Syndrome (SJS), which may occur secondary to ADR, is 0.4 to 1.2 per 1 million people per year; the estimated incidence for TEN is 1.2 to 6 per 1 million people per year. Epidemiology • Limitations of current epidemiological data – Includes all ADR – Does not differentiate immunologically and nonimmunologically mediated drug hypersensitivity – Different study populations • Inpatients or outpatients – Different methodologies – Different methods of assessing drug imputability – Different methods of data analyses Gomes ER, et al. Curr Opin Allergy Clin Immunol 2005;5:309-16 Risk factors • Drug-related factors – – – – Nature of the drug Degree of exposure (dose, duration, frequency) Route of administration Cross-sensitization • Host-related factors – – – – Age Sex Genetic factors (HLA type, Acetylator status) Concurrent medical illness (e.g. Ebstein-Barr Virus (EBV), human immunodeficiency virus (HIV), asthma) – Previous drug reaction – Multiple allergy syndrome Drug-related risk factors • Nature of the drug – Hapten concept (intrinsically reactive) – Pro-hapten concept (requires conversion to reactive intermediates) – Danger concept (drug related cytotoxicity enhancing immune response) – Pharmacological interaction concept (direct non-covalent binding to immune receptors, T-cell receptors, MHC) • Degree of exposure – Dose, duration, frequency, intermittent repeated administration • Route – Topical, oral, parenteral • Cross-sensitization – Reactivity either to drugs with a close structural chemical relationship or to immunochemically similar metabolites. Host-related risk factors • Age – Most of the studies among children and adults not comparable • Sex – No evidence, with the possible exception of cutaneous reactions, that allergic drug reactions are more common in females than in males. • Genetic factors (HLA type, Acetylator status) • Concurrent medical illness (e.g. Ebstein-Barr Virus (EBV), human immunodeficiency virus (HIV), asthma) • Previous drug reaction • Multiple allergy syndrome – May have a predilection to more than one non-cross-reacting medication, but the existence of this condition is controversial. Genetic risk factors Immunogenetic disposition together with race: 1. HLA-B*1502: Carbamazepine: SJS/TEN, DRESS; Han Chinese but not Caucasians 2. HLA-B*5801: Allopurinol: DHS/DRESS like, Han Chinese 3. HLA-B*5701: Abacavir: DRESS like, Caucasians, but not Hispanics or Africans Viral infections & autoimmunity Viral infections & autoimmunity: Generalized immune stimulation in the frame of • Acute EBV infections: maculopapular exanthem with aminopenicillins • HIV infections: – Sulfonamides: MPE, SJS/TEN, DRESS – SJS/TEN to various drugs is 500 fold more frequent – Nevirapine and abacavir: frequent side effects • Drug induced autoimmunity: – Drug-induced Lupus – Drug-induced vasculitis Pathophysiology of drug reactions • Antigenicity of drugs – Hapten concept – Prohapten concept – p-i (pharmacological interaction with immune receptors) concept • Classification of drug reactions – Type I – Type II – Type III – Type IV • a, b, c, d reactions • Hapten Hapten, prohapten and p-i concept – chemically reactive drug – able to bind covalently to proteins • Prohapten – chemically non reactive drug – becomes reactive upon metabolism (transformation of prohapten hapten) • p-i concept – parent, chemically non reactive drug – unable to bind covalently to proteins – can nevertheless interact with “immune receptors” like T-cell receptors for antigen and elicit an immune response How can drugs stimulate the immune system (I)? • Hapten/prohapten concept – The hapten-carrier complex (e.g. penicillin covalently bound to albumin) leads to formation of neoantigens: these will be recognized by the immune system (haptenspecific Ig on B-cells and by T-cells) – The binding of haptens to cellular structures may be associated with stimulation of the innate immune system. This provides “danger signals”, e.g. leading to upregulation of CD40/CD86 on Dendritic Cells Hapten concept: Possible reactive sites of benzylpenicillin Benzylpenicillin (PenG) S 2 O C H2 H N O 1 N H CH3 S CH3 N ONa O Penicilloyl- O C H2 S H N H S N CH3 CH3 O Penicilloate- ONa O PenG is a hapten like drug, as it can rapidly form covalent bonds to other proteins. 1) via the b-lactam ring (1), which opens and tends to form a bridge to lysin: „major determinant“. 2) via the thiazolidin moiety (2) of the penicillin: forming „minor determinant“ Hapten concept O C H2 penicillin H N H S N CH3 CH3 O ONa O Ig processing Binding of a chemically reactive structure to 1) soluble proteins (IgE, IgG) or 2) membrane bound proteins ( IgG + T-cell reactions) or 3/4) the MHC-peptide complexes (I & II) directly ( only T-cells) Distinct clinical consequences of hapten carrier formation depending on binding to soluble or cell bound proteins Drug (hapten) presentation to immune system (B & T cells) • Potentially highly immunogenic • Immunostimulatory properties (activation of dendritic cells) • B and T cell response • Clinical : “everything” binding to cell-bound and soluble proteins Ig: anaphylaxis, hemolytic anemia, thrombocytopenia... T-cell: contact dermatitis, hepatitis, interstitial lung disease, MPE, AGEP, TEN, .... MPE: maculopapular drug exanthema, AGEP: acute generalized exanthematous pustulosis, TEN: Toxic epidermal necrolysis Prohapten - Metabolism required - e.g. Sulfamethoxazole Hypersensitivity R NH R NH SO SO GSH NH2 sulfamethoxazole R= N O Cribb & Spielberg, 1992 Gill et al., 1997 R NH R NH SO SO NO NH S GSH NHOH O sulfamethoxazole hydroxylamine nitroso sulfamethoxazole sulfamethoxazole protein conjugate ANTIGEN PROCESSING CH3 HYPERSENSITIVITY IMMUNE RESPONSE Prohapten concept sulfamethoxazole (SMX) NH2 NO NH2 O S O O S O N O NH R O S O SMX-NO R metabolism inert reactive H3C Metabolism is required to generate reactive compounds, which then behave like haptens and bind to soluble and cell bound proteins. Drug (prohapten) presentation to immune system (B & T cells) • Many drugs are potentially highly immunogenic as they are transformed to chemically active intermediates • Potent and rapid intracellular detoxification mechanism (i.e. GSH) may prevent immunogenicity of the generated reactive metabolites • It is possible that the liver may play a role as a tolerogenic organ ---------------------------------------------------------------------------------------Clinical: potentially immunogenic for B- and T-cells; • Immunogenicity and clinical manifestation might be restricted to the organ where metabolism (generation of hapten and stimulation of innate immunity) takes place, namely the liver (hepatitis) or kidney (interstitial nephritis) How can drugs stimulate the immune system (II) ? • Pharmacological interaction with immune receptors (pi concept) – direct stimulation of T-cells by drugs binding to the T-cell receptors for antigen – no involvement of the innate immune system, and no generation of an own immune response to the drug – stimulation of preactivated T-cells with additional specificity The p-i concept: Pharmacological Interaction of drugs with immune Receptors A chemically inert drug, unable to covalently bind to some proteins, „happens“ to bind to some of the 1012-1015 distinct immune receptors (as it does to other proteins/receptors). This drug-receptor interaction can under certain circumstances activate specific immune cells. The subsequent reaction imitates a specific immune response. The p-i-concept: Pharmacological interaction of drugs with immune receptors* peptide *) elaborated for T-cell receptors (TCR) only a) Binding of the drug to TCR, providing an initial signal b) Additional MHC- TCR interaction, supplementing the signal c) Readiness of the T cell to react (low threshold level of activation) T-cell recognition of hapten like drugs: covalent drug binding to MHC-peptide NO Covalent binding (SMX-NO) N O S O NH O H3C T-cell TCR APC (e.g. activated keratinocyte, DC,...) MHC+ peptide „Classical“ immune response to hapten carrier compound Direct stimulation of T-cells by nonhapten like drugs: direct interaction with the TCR NH2 Sulfamethoxalole (SMX) 1 T-cell TCR N O S O NH O APC (e.g. activated keratinocyte) H3C 2 MHC+ peptide Labile, non covalent binding of SMX itself to TCR; This initial stimulation is supplemented by TCR-MHC interaction SUMMARY: “Antigenicity” of drugs NH2 O S O HAPTEN N P-I CONCEPT NH O • • • • • Chemical (hapten) H3C Stable protein/peptide modification (covalent) MHC-APC directed (processing and metabolism) Very heterogeneous and often combined immune responses (Ig, Tcells.....) • • Structural (fitting into TCR) No covalent binding • • • TCR – T cell directed No processing/no metabolism Only T-cell reactions of different types (exanthema, DRESS, AGEP.....) Gell & Coombs Classification of Hypersensitivity reactions Immune reactant Antigen Type I Type II Type III Type IV IgE IgG IgG T cell Soluble antigen Cell- or matrixassociated antigen Soluble antigen Mast-cell activation FcR+ cells (phagocytes, NK cells) FcR+ cells Complement Effector MHC-presented antigen T-cells, via cytokines recrutement of monocytes, eosinophils, neutrophils(?) blood platelets vessel Ab - platelet immune complex Ag Example of hypersen-sitivity reaction Allergic rhinitis, asthma, systemic anaphylaxis Some drug allergies (e.g. penicillin) Serum sickness, Arthus reaction Cytokines cytotoxicity Many different diseases: Different forms of exanthems, eczema, contact dermatitis Delayed reactions • • • • Due to drug specific T cells T-cells secrete different cytokines The cytokines activate and recruit distinct effector cells Cytotoxic mechanism are always involved, in some severe reactions (SJS/TEN) even dominating the clinical symptoms • Similar mechanism in skin as in internal organs (e.g. interstitial nephritis) Mechanism of immune mediated exanthems T-cells recognize the drug and exert, depending on their function, a specific pathology Bullous Exanthem Maculopapular exanthem (MPE) Acute generalized exanthematous pustulosis (AGEP) MPE: infiltration of T cells in dermis and epidermis CD4+ CD8 + Perforin and Granzyme B • Are important for cellmediated cytotoxicity • Are preformed in granules of cytotoxic T-cells (CTLs, NK) • Are released during exocytosis of granules and form pores in the cell membrane of the target cell with subsequent fragmentation of DNA. CTL Killing of e.g. keratinocytes or hepatocytes Perforin+ and Granzyme B+ cells infiltrate into the epidermis Perforin Granzyme B In MPE infiltrating T cells are killing keratinocytes and orchestrate an inflammatory process, which is often eosinophil rich keratinocyte keratinocyte cell necrosis ICD541 hydropic degeneration eosinophils mononuclear cell infiltrate MHC II perforin granzymeB TCR LFA-1 - Drug specific CD4+ T cell Comparison of MPE and Bullous Exanthem • Higher activation of circulating T-cells (CD4 and CD8) in bullous exanthem • Higher activation of CD8+ T-cells in the skin of patients with bullous exanthem Bullous exanthem: CD8 MPE: CD4 Why are cytotoxic CD8+ T cells more dangerous than CD4+ T cells ? CD8 MHC I CD4 Activated, MHC II+ CD8 T cells can kill all cells, not only activated MHC II+ cells T-cells recognize the drug and exert, depending on their function, a specific pathology Bullous exanthem MHC-I (+ MHC-II) CD8+ > CD4+ cytotoxicity (CD8+) IFN ; IL-5 Amoxicillin MPE MHC-II CD4+ cytotoxicity (CD4+) IL-5; IFN AGEP MHC-II + I CD4+ & CD8+ cytotoxicity IL-8; IL-5, IL-17 (?) World Allergy Organization (WAO) For more information on the World Allergy Organization (WAO), please visit www.worldallery.org or contact the: WAO Secretariat 555 East Wells Street, Suite 1100 Milwaukee, WI 53202 United States Tel: +1 414 276 1791 Fax: +1 414 276 3349 Email: [email protected]