* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Function Nervous System Endocrine System
Survey
Document related concepts
Transcript
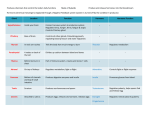
Endocrine System Carl B. Goodman, Ph.D. College of Pharmacy & Pharmaceutical Sciences Florida A&M University 308E FSH-SRC 599-3128 [email protected] Endocrine System: Homeostasis Hormone - Regulatory molecules secreted into blood stream Endocrine Gland - Ductless glands contains secretory cells - Synthesis or produce hormones Effector - Target cells or tissues - Contains receptors to produce some physiological response Endocrine System vs Nervous System Function Secretory Cells Nervous System Neuron Endocrine System Glandular Epithelial Cells & Neurosecretory Cells Distance Short (Synapse) Long (Blood) Location of Receptors In Effector Cells Plasma Membrane Plasma Membrane & Within the Cell Characteristics of Regulatory Effects Appears Rapid, Short Lived Slow, Long Lasting Diagram Pre & Post Neurons Synaptic Target Cells Endocrine System vs Nervous System Function Overall Function Nervous System Regulate Effectors *HOMEOSTASIS Endocrine System Regulate Effectors *HOMEOSTASIS Control Feedback Loop Yes (Nervous Reflex) Yes (Endocrine Reflex) Chemical Messenger Neurotransmitter Hormone (Proteins or Steroids) Effector Tissues Muscle & Glandular Tissues All Cell Types *Muscles, Bones, Glandular Effector Cells Post Synaptic Neurons Target Cells Endocrine Action Endocrine System Endocrine Glands CNS: Pituitary Gland Periphery: Pancreas, Thyroid, Parathyroid, Adrenal, Testes and Ovaries Organs with Partial Endocrine Functions Hypothalamus, Pineal Gland, Stomach, Duodenum, Liver, Thymus, Heart, Skin, Kidney, Lung and Placenta Types of Hormones: Lipid Soluble Steroids - Cortisol - Aldosterone - Androgens - Estrogen/Progesterone - Testosterone - Calcitrol (Kidney) Gas - Nitric Oxide (NO) Thyroids - Triiodothyronine (T3) - Thyroxine (T4) Types of Hormones: Water Soluble Glycoproteins - Follicle Stimulating Hormone (FSH) - Luteinizing Hormone (LH) - Thyroid Stimulating Hormone (TSH) Peptides - Anti-diuretic Hormone (ADH) (8 AA) - Oxytocin (8 AA) - Melanocyte Stimulating Hormone (MSH) - Thyroid Releasing Hormone (TRH) Proteins - Growth Hormone (191), Calcitonin (32 AA), Prolactin, Insulin (21 & 30 AA), ACTH (39 AA), Parathyroid Hormone (84 AA) Fatty Acids (Arachidonic acid) - Leukotrienes - Prostaglandins - Thromboxanes - Prostacyclins Types of Hormones: Amino Acids Amines (Water Soluble) - Norepinephrine (Tyrosine) - Epinephrine (Tyrosine) - Melatonin (Tryptophan) - Serotonin (Tryptophan) - Histamine (Histadine) Iodinated Amino Acid - Thyroxine (T4) - Triiodothyronine (T3) Hormone Circulation Endocrine Action: hormone is distributed in blood and binds to distant target cell Paracrine Action: hormone acts locally by diffusing from its source to target cells in the neighborhood Autocrine Action: hormone acts on the same cell that produced it Hormone Transport in Blood Protein hormones circulate in free form in blood Steroid (lipid) & thyroid hormones must attach to transport proteins (Carrier Molecules) synthesized by liver – improve transport by making them water-soluble – slow loss of hormone by filtration within kidney – create reserve of hormone • only .1 to 10% of hormone is not bound to transport protein = free fraction Synthesis and Metabolism General Mechanisms of Hormone Action Hormone binds to cell surface or receptor inside target cell Cell may then: – synthesize new molecules (Protein Synthesis) – change permeability of membrane (Ion channels) – alter rates of reactions (Enzymes) Each target cell responds to hormone differently – Liver cells: insulin stimulates glycogen synthesis – Adipose: insulin stimulates triglyceride synthesis Circadian Rhythm for all Hormones (Basal Level) - Ex. Cortisol: increased daytime and decreased at night Hormone Interaction Synergistic Permissive- a second hormone, strengthens the effects of the first Ex. thyroid strengthens epinephrine’s effect upon lipolysis or Estrogen and Progesterone are need for maturation of follicle Antagonistic ex. Insulin and Glucagon Prehormone ex. T4 converted to T3 ex. Vitamin D3 converted to 1,25 dihydroxyvitamin D3 Role of Hormone Receptors Constantly being synthesized & broken down A range of 2,000-100,000 receptors / target cell Down-regulation (Hypersecretion of Hormone) – excess hormone, produces a decrease in number of receptors • receptors undergo Endocytosis and are degraded – decreases sensitivity of target cell to hormone Up-regulation (Hyposecretion of Hormone) – deficiency of hormone, produces an increase in the number of receptors – target tissue more sensitive to the hormone H + R = HR Complex Intracellular Chemical Signal Autocrine: secreted in a local area ex. Prostaglandins Paracrine: neighboring cell ex. Histamine, Prostaglandins Hormone: secreted in blood… ex. Insulin, T4, and T3 Neurohormone: produced by neurons ex. Oxytocin, ADH Neurotransmitter or Neurohumor: Pheromone: produced by neurons and secreted into synapse ex. Acetylcholine and Epinephrine pheromones secreted in environment, modifies behavior ex. Sex Hormone Signal Transduction Pathway Steroids Hormone Protein Hormone Second Messengers cAMP cGMP Phospholipase C Ca++ Opposing 2nd Messenger System with Same Hormone Beta Adrenergic Receptors - Relaxation/Dilation = cAMP Alpha Adrenergic Receptors - Constriction = Phospholipase C Feedback Control System Negative Feedback Positive Feedback Hypothalamic-Pituitary System Neurohypophysis Adenohypophysis Pituitary Gland = Hypophysis Hypothalamic-Pituitary System Pars Tuberalis Pars Nervosa Pars Distalis Pars Intermedia Posterior Pituitary Gland: Neurohormones Anti-diuretic Hormone (ADH) or Vasopressin Osmoreceptors near Supraoptic Nucleus (Dehydration) (Alcohol) H2O is reabsorbed from the tubules of the kidney and returned to the blood instead of the urine (H20 is conserved) Decrease in rate of perspiration during dehydration Raises Blood Pressure by constricting Arterioles Oxytocin Stimulate contraction of uterine muscle (smooth muscle) Initiate milk ejection from the Alveolar Cells into the ducts of the breast in lactating women Melanocyte-Stimulating Hormone (MSH) Pars Intermedia (Corticotroph cells) Melanocytes - Melanin (Darkening of Skin) Pre-proopiomelanocortin 2o Addision’s Disease (skin darkening) Estrogen/Progesterone (skin darkening) Anterior Pituitary Gland Growth Hormone (Somatotrophin) Prolactin Tropic Hormones Adenocorticotrophic Hormone (ACTH) Thyroid Stimulating Hormone (TSH) Luteinizing Hormone (LH) Follicle Stimulating Hormone (FSH) Growth Hormone Produced by somatotrophs (191AA) Within target cells increases synthesis of Somatomedins and Insulin-like Growth Factors that act locally or enter bloodstream – common target cells are liver, skeletal muscle, cartilage and bone – increases cell growth & cell division by increasing their uptake of amino acids & synthesis of proteins – stimulate lipolysis in adipose so fatty acids used for ATP – retard use of glucose for ATP production so blood glucose levels remain high enough to supply brain Abnormal Levels of Growth Hormone Hypersecretion of GH Hyposecretion of GH During the growth years before ossification of Epiphyseal plates, causes increase in rate of skeletal growth = Gigantism After the growth years = Acromegaly -Excess cartilage growth forming new bones. -Enlarged hands, feet, jaws, separation of teeth, -*Soft Tissue (forehead and nose) During the growth years, results in stunted body growth = Pituitary Dwarfism Prolactin Hypothalamus regulates lactotroph cells Primary function is to generate/initiate milk secretion (Lactation) 1. During Pregnancy, high prolactin promote development of breast for milk secretion 2. At Birth of an Infant, suckling reduces levels of hypothalamic inhibition and prolactin levels rise along with milk production Mammary glands are primed with E/P, Cortisol, GH, T4 and Insulin Nursing ceases & milk production slows Abnormal Levels of Prolactin Hypersecretion of Prolactin Hyposecretion of Prolactin Causes lactation in non-nursing women Disruption of the menstrual cycle (Men) can cause impotence Insignificant except in women, who want to nurse feed their babies ACTH Hypothalamus releasing hormones stimulate corticotrophs Corticotrophs secrete ACTH & MSH ACTH stimulates cells of the adrenal cortex that produce glucocorticoids & TSH Hypothalamus regulates thyrotroph cells Thyrotroph cells produce TSH TSH stimulates the synthesis & secretion of T3 and T4 Metabolic rate stimulated Gonadotrophins Luteinizing Hormone Releasing hormones from hypothalamus stimulate gonadotrophs Gonadotrophs produce LH In females, LH stimulates – secretion of estrogen – ovulation of 2nd oocyte from ovary – formation of corpus luteum – secretion of progesterone In males, stimulates interstitial cells to secrete testosterone Follicle Stimulating Hormone Releasing hormone from hypothalamus controls gonadotrophs Gonadotrophs release follicle stimulating hormone FSH functions – initiates the formation of follicles within the ovary – stimulates follicle cells to secrete estrogen – stimulates sperm production in testes Pathophysiology of HP Axis Hypothalamus Pituitary Gland 1. Tumors - increase release of hormones - destruction of hypothalamus 2. Drugs - increase or decrease hormones release 3. Heavy blow to the head 4. Infarction of the Primary plexus of the hypophyseal portal system 1. Tumors - increase release of hormones - destruction of pituitary gland 2. Drugs - increase or decrease hormones release 3. Infarction of the Secondary plexus of the hypophyseal portal system Target Cell Failure Receptor-associated disorders – Decrease in number of receptors – Impaired receptor function – Presence of antibodies against specific receptors – Antibodies that mimic hormone action – Unusual expression of receptor function Disease of the Posterior Pituitary Syndrome of inappropriate antidiuretic hormone secretion (SIADH) – Hypersecretion of ADH – For diagnosis, normal adrenal and thyroid function must exist – Clinical manifestations are related to enhanced renal water retention, hyponatremia, and hypoosmolarity Disease of the Posterior Pituitary Diabetes Insipidus – Insufficiency of ADH – Polyuria and polydipsia – Partial or total inability to concentrate the urine – Neurogenic • Insufficient amounts of ADH – Nephrogenic • Inadequate response to ADH Disease of the Anterior Pituitary Hypopituitarism – Pituitary infarction • Sheehan syndrome • Hemorrhage • Shock – Others: head trauma, infections, and tumors Disease of the Anterior Pituitary Hypopituitarism – Panhypopituitarism • • • • ACTH deficiency TSH deficiency FSH and LH deficiency GH deficiency Disease of the Anterior Pituitary Hyperpituitarism – Commonly due to a benign, slow-growing pituitary adenoma – Manifestations • Headache and fatigue • Visual changes • Hyposecretion of neighboring anterior pituitary hormones Adrenal Gland Small bilateral structures located superior or at the apex of each kidney Weigh about 5 grams each 2 Major regions: Cortex and Medulla Cross Section & Histology Minerocorticoids Aldosterone 95% of hormonal activity due to aldosterone Functions – increase reabsorption of Na+ with Cl- , bicarbonate and water following it – promotes excretion of K+ and H+ Regulation of Aldosterone Glucocorticoids 95% of hormonal activity is due to cortisol Functions = help regulate metabolism – – – – increase rate of protein catabolism & lipolysis conversion of amino acids to glucose stimulate lipolysis provide resistance to stress by making nutrients available for ATP production – raise BP by vasoconstriction – anti-inflammatory effects reduced (skin cream) • reduce release of histamine from mast cells • decrease capillary permeability • depress phagocytosis Pathophysiology of Adrenal Gland Hypersecretion of Cortisol Cushing’s Disease/Syndrome Central Obesity Moon Face & Buffalo Hump Hypertension & Hypokalemia Hyperglycemia MCC: Lung Cancer secreting ACTH Pathophysiology of Adrenal Gland Hyposecretion Glucocorticoids & Minerocorticoids Addison’s Disease Hypotension Skin Pigmentation Loss of NaCl Muscle Weakness Unable to resist stress MCC: Autoimmune Disease Pathophysiology of Adrenal Gland Hypersecretion of Aldosterone Hypersecretion of Androgens Conn’s Syndrome Hypertension Hypokalemia Metabolic Alkalosis Congential Adrenal Hyperplasia Hirsuitism • Primary hyperaldosteronism (Conn disease) • Secondary hyperaldosteronism MCC: Tumor MCC: Congential Defect Androgens Small amount of male hormone produced – insignificant in males – may contribute to sex drive in females – is converted to estrogen in postmenopausal females Adrenal Medulla Chromaffin cells receive direct innervation from sympathetic nervous system – develop from same tissue as postganglionic neurons Produce Epinephrine (80%) & Norepinephrine (20%) Hormones are sympathomimetic – effects mimic those of sympathetic NS – Ex. Increase if rate/force of contraction, constricts blood vessels, dilation of bronchioles, increase metabolic rate – cause fight-flight behavior (Stress) Short Term (Epi/NE) Long Term (Glucocorticoids) Acetylcholine increase hormone secretion by adrenal medulla Stimuli: Exercise, Emotional stress, Hypoglycemia Pathophysiology of Adrenal Medulla Hypersecretion of Adrenal Medulla Hormones Episodic Hypertension Tumor: Pheochromocytoma Epi/NE from adrenal medulla are hormones and their actions are longer lasting than Epi/NE from the SNS Hyposecretion of Adrenal Medulla Hormones Rare Thyroid Gland Thyroid Hormones & Their Effects T4 (Thyroxine) (Tetra-iodothyronine) 4-Iodine molecules T3 Triiodothyronine 3-Iodine molecules Regulates Body’s Metabolic Rate (Calorigenic Effect) - Increase Oxygen consumption - Increase Heat production (Heart, Muscle, Visceral Tissues) Promote Body Growth/Development - Increase protein synthesis, particularly in muscles and bones - Initiates cell differentiation Cardiovascular Effects - Increase heart rate and contractility - Increase vascular responsiveness to Epi/NE; Increase BP Thyroid Hormones & Their Effects Calcitonin Produced by the Parafollicular cells (C cells) of the thyroid gland Inhibits Osteoclast cells Decrease Ca++ plasma levels Promote bone deposition Increase rate of Ca++ and Phosphorus by kidney Thyroid Hormone Synthesis Iodide trapping by follicular cells Synthesis of thyroglobulin (TGB) Release of TGB into colloid Iodination of tyrosine in colloid Formation of T3 & T4 by combining T1 and T2 together Uptake & digestion of TGB by follicle cells Secretion of T3 & T4 into blood Pathophysiology of Thyroid Gland Hypersecretion of Thyroid Hormones Hyposecretion of Thyroid Hormones Graves’ Disease Increase metabolism Goiters Exophthalamos Cretinism (Children) Mentally retarded Stunted growth, dwarfism Enlarged tongue and abdomen MCC: Congential MCC: Autoimmune Myxedema (Adults) Thick dry skin Weakness, fatigue Delayed tendon reflex Slowed mentation MCC: Hyperthyroid Trxt Parathyroid Gland Regulated by Ca++ Levels (low levels) Stimulate release of Ca++ from bones Pathophysiology Hypersecretion (Hypercalcemia) - Factures & cysts of bones - Calcium deposits in tissues MMC: Lung Cancer Hyposecretion (Hypocalcemia) – Tetany: Flexion of wrist and joints (Carpopedal spasm) MMC: Removal of thyroid gland Pancreas Pancreatic Cell Types Alpha cells (20%) - Glucagon Beta cells (70%) - Insulin Delta cells (5%) -Somatostatin - Identical to GHIH - Inhibits both insulin and glucagon release (Paracrine action) - Slow absorption of nutrients from GI tract F cells - Pancreatic polypeptide - Inhibits somatostatin secretion, gall bladder contraction and secretion of digestive enzymes by pancreas THE EFFECTS OF INSULIN ON PLASMA GLUCOSE Increase in Plasma Glucose Pancreas Beta Cells-Insulin Adipose Tissue Skeletal Muscle Fat Energy Liver Glycogen Plasma Glucose Levels All people with diabetes have one thing in common: they have too much sugar, or glucose, in their blood. A normal blood sugar level for a person without diabetes is usually about 60-110 milligrams per deciliter (mg/dL). This is the proper level needed for normal body function. When the blood sugar level drops too low (hypoglycemia), a person's ability to reason is impaired; in extreme cases, coma may result. When the blood sugar is consistently too high (hyperglycemia), a diagnosis of diabetes is possible. Diabetes Mellitus Diabetes mellitus are metabolic diseases characterized by hyperglycemia resulting from defects in insulin secretion, insulin action, or both. Type 2 diabetes, the most prevalent form of the disease, is often asymptomatic in its early stages and can remain undiagnosed for many years. Approximately 5.4 million adults in the U.S. have undiagnosed type 2 diabetes. Diabetes Mellitus Type I • Type 2 Results from an autoimmune destruction of pancreatic Beta cells • Insulin is secreted, but it is ineffective in normalizing plasma glucose • Occurs usually at less than 20-30 years of age (Juvenile Onset) • Cardinal finding-increments in plasma insulin do not lead to the expected increases in glucose disposal. This is referred to as “Insulin Resistance” • Cardinal finding-inability to secrete even the modest amount of insulin to suppress ketone formation • People with type 1 diabetes must take daily insulin injections to stay alive. Type 1 diabetes accounts for 5-10 percent of diabetes. • Type 2 diabetes accounts for 9095 percent of diabetes. It is nearing epidemic proportions, due to an increased number of older Americans. Symptoms of DM I & II Type 1 Diabetes: · Frequent urination · Unusual thirst · Extreme hunger · Unusual weight loss · Extreme fatigue · Irritability Type 2 Diabetes: · Any of the type 1 symptoms · Frequent infections · Blurred vision · Cuts/bruises that are slow to heal · Tingling/numbness in the hands or feet · Recurring skin, gum or bladder infections * Often people with Type 2 diabetes have no symptoms. COMPLICATION CAUSED BY TYPE 2 DIABETES Unchecked diabetes can lead to serious conditions. These include: Heart disease, stroke, and blood-vessel (cardiovascular) diseases. Cardiovascular disease is by far the leading cause of death in the United States, but people with diabetes are at much higher risk. Kidney disease. Also called nephropathy, this complication happens when the kidney's "filter mechanism" is damaged and protein leaks into urine in excessive amounts and eventually the kidney fails. Eye diseases. Diabetes is a leading cause of damage to the retina at the back of the eye and also increases risk of cataracts and glaucoma. Nervous-system problems. Nerve damage, especially in the legs and feet, may interfere with the ability to sense pain and contributes to serious infections. Pathogenesis of Type 2 DIABETES Progressive metabolic defect whereby a disruption in the delicate balance by which insulin target tissues communicate with the pancreatic beta-cells and vice versa to maintain normal glucose homeostasis Impaired insulin secretion Insulin resistance Increased rate of endogenous hepatic glucose production (HGP) Progression of insulin resistance leads to a compensatory hyperinsulinemia DECREASE INSULIN LEVELS PRODUCES THREE MAJOR EFFECTS IN DIABETICS 1) Decreased utilization of glucose by the body's cells, resulting in elevated blood glucose concentrations; 2) Increased mobilization of fats from storage sites, resulting in abnormal fat metabolism and lipid deposition in the vascular walls, leading to atherosclerosis; and 3) Depletion of proteins in body tissues. HOW DO WE IDENTIFY THOSE PATIENTS WITH HYPERGLYCEMIA? “Blood Glucose Tests” 1) Screening Test 2) Diagnostic Test SCREENING TESTS It is estimated that about 2.5% of the US population may have diabetes that will go undetected unless screening tests are performed. WHO SHOULD BE SCREENED: Persons with a strong family history of diabetes mellitus Persons who are markedly obese Women with an obstetrical history resulting in morbidity or a history of babies of over 9 pounds at birth All women between 24 and 28 weeks of pregnancy Anyone with recurrent skin, genital, or urinary tract infections Persons older than 65 years of age Certain races (American Indian, Hispanic, and African American) Persons who have had previous impaired glucose tolerance Persons who are hypertensive (blood pressure at or above 140/90) Persons who have an HDL cholesterol level (the "good" cholesterol) of 35 mg/dL or lower and/or a triglyceride level of 250 mg/dL or higher The American Diabetes Association Diabetes Risk Test HEMOGLOBIN A1c (HbA1c) BLOOD TEST Measures glycosylated hemoglobin, a molecule that gauges how well diabetics controlled their blood glucose during the previous months. Glycosylated hemoglobin forms when hemoglobin molecules, which are found in red blood cells, link up with glucose molecules. The more glucose in the blood, the more hemoglobin becomes glycosylated. Once glycosylated, hemoglobin stays that way until the red blood cell dies -- about 120 days. The result is given as a percentage. People who don't have diabetes typically have HbA1c readings of about 4% to 5.5%. Fasting Plasma Glucose Test The fasting plasma glucose test is the preferred way to diagnose diabetes. It is easy to perform and convenient. After you have fasted overnight (at least 8 hours), a single sample of your blood is drawn at the doctor’s office and sent to the laboratory for analysis. Normal fasting plasma glucose levels are less than 110 milligrams per deciliter (mg/dL). Fasting plasma glucose levels of more than 126 mg/dL on two or more tests on different days indicate diabetes. INSULIN PREPARATIONS Reaches Blood Peak Duration of Action Rapid-acting (Lispro) 15 minutes 30-90 minutes 5 hours Short-acting (Regular) 30 minutes 2-4 hours 4-8 hours Intermediate-acting (NPH and Lente) 2-6 hours 4-14 hours 14-20 hours Long-acting (Ultralente) 6-14 hours No peak or a small peak 10-16 hours 20-24 hours INSULIN Pineal Gland Located dorsal of the diencephalon region near the 3rd ventricle Comprises 2 systems: 1) NS, receiving visual nerve input -Helps determine: day length- daily and seasonal cycles (time length); lunar cycle-menstrual cycle 2) ES, secretes Melatonin (Induces Sleep) -Support the Biological Clock -Regulates our eating, sleeping, female reproductive cycle and behavior Thymus Gland • Important role in maturation of T cells • Hormones produced by gland promote the proliferation & maturation of T cells – thymosin – thymic humoral factor – thymic factor – thymopoietin