* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Diplopia-strabismus_ppt_talk_10-2010
Survey
Document related concepts
Transcript
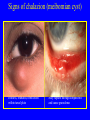
DOUBLE VISION, ACQUIRED, and CONGENITAL STRABISMUS Robert Cordero, M.D., F.A.C.S Central Florida Eye Specialists, P.L. October 30, 2010 • www.theeyespecialists.com • www.aapos • www.aao • Google 22 New, Updated, Revised, Better • • • • • • • potions, purification, diet, lancets Hammurabi’s Code 1800 B.C. Egyptian Papyrus 1600 - 1300 B.C. Susruta father of Hindu surgery Hebrew Talmud 1300 B.C.- 70 A.D. Greece, Alexandria, and Rome Middle Ages (395-1492) and Renaissance 14-16th century 3 Georg Bartisch (1535-1606) Chevalier John Taylor 1739 5 First Muscle Operations • 1838 Stromeyer, an Orthopedic surgeon on a cadaver Hanover, Germany • 1839 J.F. Diffenbach in Berlin, by 1842 had done 1,200 strabismus operations, which consisted of tenotomy of the medial rectus muscle 6 7 Eye Massager 1890 8 Double Vision=/=Diplopia • Diplopia = Seeing one object as two. Must rule out Vertigo, Syncope, Hysteria, etc. • Double the Time • Double the Effort • Double the Cost • Double the reward Questions to Ask • • • • • • • Does the DV go away by covering one eye Abnormal head posture seen in old photos Pain, facial numbness, circulatory issues Eyelid malposition and endocrine disease Fatigability, dysarthria, dysphagia, SOB FH, Meds, MH, SH, smoking, ETOH, etc Compliance and socioeconomic 10 Work-up Diplopia • • • • • • History, History, Histroy Old Records and Studies Compare Measurements Impression(s) Plan: Short and Long Term Communication Tools of the Trade • • • • • • Patience, Efficiency and Insight Lensometer readings Best Corrected Vision, Pinhole Stereopsis Prism Bars, Occluder, Pupil Light Clip-ons, Trial Set, Cycloplegia Basic Review • • • • • • Anatomy Eye Movements Binocular Vision Strabismus Motor Evaluation Sensory Evaluation 15 16 17 18 19 20 SENSORY • Simultaneous perception- brains ability to perceive images from OU at same time • Suppression-brain shuts off information • Fusion- cortical integration of separate retinal images into single sensory perception • Stereopsis- to perceive the relative distance of objects • Tests for stereopsis Titmus • • Polaroid spectacles Figures seen in 3-D TNO random dot test • • Red-green spectacles ‘Hidden’ shapes seen Lang Frisby • • No spectacles ‘Hidden’ circle seen • • No spectacles Shapes seen Tests for sensory anomalies Worth four-dot test a - Prior to use of glasses b - Normal or ARC c - Left suppression d - Right suppression e - Diplopia Bagolini striated glasses a - Normal or ARC b- Diplopia c - Suppression d - Small suppression scotoma Synoptophore • • • • Grading of binocular vision Detection of suppression and ARC Measurement of angle Measurement of fusional amplitudes Hirschberg test • Rough measure of deviation • Note location of corneal light reflex • 1 mm = 7 or 15 Reflex at border of pupil = 15 Reflex at limbus = 75 26 27 28 Motility tests • • Tests versions and ductions Grades under/overaction Left inferior oblique overaction Left lateral rectus underaction Cover tests • Cover test detects heterotropia • Uncover test detects heterophoria • Prism cover test measures tropia • Alternate measures total tropia and phoria • Alternate cover test detects total deviation Amblyopia • • • • • • • Strabismus Anisometropic (sph or cyl) > 1.5 D Deprivation (media opacity >1 mm in size or ptosis < 1 mm margin reflex distance) Cost Effectiveness Tx gain from $2053 to $2509 ($/ QALY) <20K especially good www:aao.org/ppp cost-utility analysis The Pediatric Eye Disease Investigator Group (PEDIG) • • • • • Randomized multicenter clinical study Patching regimens part vs full time 2 hr/day for moderate cases(20/40-80) Atropine 1% vs patching(6hr/day) ages 3- 7 24% recurrence < 8 years age within one year cessation either method • 27% improvement age 3-7 anisometropia Rx • 50% >2 lines age 7 to 12 either method, age 32 Types of Turns • • • • ESODEVIATION EXODEVIATION A and V Patterns Cyclovertical Monocular Diplopia Signs of chalazion (meibomian cyst) Painless, roundish, firm lesion within tarsal plate May rupture through conjunctiva and cause granuloma Morphological classification of keratoconus Nipple cone Oval cone Small and steep curvature Larger and ellipsoidal Globus cone Largest Progressive iris atrophy Progressive stromal iris atrophy Broad-based PAS Displacement of pupil towards PAS Isolated familial ectopia lentis Autosomal recessive Pupil may be normal Pupil may be displaced in opposite direction (ectopia lentis et pupillae) Classification according to maturity Immature Hypermature Mature Morgagnian Implant displacement Decentration • May occur if one haptic is inserted into sulcus and other into bag • Remove and replace if severe Optic capture • Reposition may be necessary Binocular Diplopia No Misalignment INCOMITANT Mechanical (Restrictive) Diplopia • • • • • • Grave’s Ophthalmopathy Brown’s Syndrome Orbital Pseudotumor Ocular Myositis Orbital Mass Lesions Orbital Trauma Signs of eyelid retraction Occurs in about 50% • Bilateral lid retraction • No associated proptosis • Bilateral lid retraction • Bilateral proptosis • Unilateral lid retraction • Unilateral proptosis • Lid lag in downgaze Restrictive myopathy • Occurs in about 40% • Due to fibrotic contracture Elevation defect - most common Depression defect - uncommon Abduction defect - less common Adduction defect - rare Optic neuropathy • Occurs in about 5% • Early defective colour vision • Usually normal disc appearance Caused by optic nerve compression at orbital apex by enlarged recti Often occurs in absence of significant proptosis Brown syndrome (right) Normal elevation in abduction Straight in primary position Limited elevation in adduction Idiopathic orbital inflammatory disease (IOID) • Non-neoplastic, non-infectious orbital lesion (pseudotumour) • Involves any or all soft-tissue components • Presentation - 20 to 50 years with abrupt painful onset • • • • Usually unilateral Periorbital swelling and chemosis Proptosis Ophthalmoplegia Clinical course and treatment of IOID 1. Early spontaneous remission without sequelae Treatment - nil 2. Prolonged intermittent activity with eventual remission Treatment options - steroids, radiotherapy or cytotoxics 3. Severe prolonged activity causing a ‘frozen orbit’ Left involvement resulting in ophthalmoplegia and ptosis Orbital myositis • • • • Subtype of IOID Involvement of one or more extraocular muscles Clinical course is usually short - treat with NSAIDs Presentation - sudden onset of pain on ocular movement • Underaction of left lateral rectus • Worsening of pain on attempted left gaze • CT shows fusiform enlargement of left lateral rectus Cavernous haemangioma • Most common benign orbital tumour in adults • Usually located just behind globe • Female preponderance - 70% • Presents - 4th to 5th decade Slowly progressive axial proptosis May cause choroidal folds Treatment - surgical excision Pleomorphic Lacrimal Gland Adenoma Presents - 4th to 5th decade • Painless and very slow- • Posterior extension may • Smooth, encapsulated growing, smooth mass in cause proptosis and outline ophthalmoplegia lacrimal fossa • Excavation of lacrimal gland • Inferonasal globe fossa without destruction displacement Lacrimal gland carcinoma • Presents - 4th to 6th decades • Very poor prognosis Posterior extension may cause proptosis, ophthalmoplegia and episcleral congestion • Trigeminal hypoaesthesia in 25% • • • Painful, fast-growing mass in lacrimal fossa Infero-nasal globe displacement Management • • Biopsy Radical surgery and radiotherapy Optic nerve glioma • Typically affects young girls • Associated neurofibromatosis -1 is common • Presents - end of first decade with gradual visual loss Gradually progressive proptosis Optic atrophy Treatment • Observation - no growth, good vision and good cosmesis • Excision - poor vision and poor cosmesis • Radiotherapy - intracranial extension Sphenoidal ridge meningioma Presents with gradual visual loss and reactive hyperostosis Proptosis Fullness in temporal fossa Hyperostosis on plain x-ray Lymphoma Presents - 6th to 8th decades Affects any part of orbit and Anterior lesions are rubbery May be confined to may be bilateral on palpitation lacrimal glands Treatment • • Radiotherapy - localized lesions Chemotherapy - disseminated disease Direct carotid-cavernous fistula • Defect in intracavernous part of internal carotid • Rapid flow shunt Causes • Head trauma - most common • Spontaneous rupture - in hypertensive females • Ptosis, chemosis and conjunctival injection • Ophthalmoplegia • Raised intraocular pressure Direct carotid-cavernous fistula • Pulsatile proptosis with bruit • Retinal venous congestion and haemorrhages and thrill • Abolished by ipsilateral carotid compression Indirect carotid-cavernous fistula (dural shunt) • Indirect communication between meningeal branches of internal or external carotids and cavernous sinus • Slow flow shunt Causes • Congenital malformations • Spontaneous rupture • Dilated episcleral vessels • Raised intraocular pressure with wide pulsation • Occasional ophthalmoplegia and mild proptosis Incomitant Misalignment Tensilon Test • Tensilon (Edrophonium HCL) 10 mg/ml fast acting anti-cholinesterase • Neostigmine (Prostigmin) IM (0.02mg/kg) alternative • Have injectable Atropine Sulfate ready Ophthalmic Signs of Myasthenia Gravis • • • • • • • • Ptosis EOM Palsies Pseudogaze Palsies Pseudointernuclear Ophthalmoplegia Pseudoconvergence Paresis Lid Twitch Quiver Movements Orbicularis Weakness Myasthenia Gravis 1. Clinical features • • • Uncommon, typically affects young women Weakness and fatiguability of voluntary musculature Types: Neonatal, Congenital, Ocular, System 2. Investigations ICE Test •Tensilon test (edrophonium) or Prostigmine • Antibodies to acetylcholine receptors 3 types, MuSK (muscle-specific receptor tyrosine kinase) • CT or MRI for presence of thymoma • 3. Treatment options • • Medical - AChE inhibitor, steroids, immunomodulators Thymectomy, prisms, strabismus surgery Ocular myasthenia Ptosis • • • Insidious, bilateral but asymmetrical Worse with fatigue and in upgaze Ptotic lid may show ‘twitch’ and ‘hop’ signs Diplopia • Intermittent and usually vertical Edrophonium test Before injection • Measure amount of ptosis or diplopia before injection • Inject i.v. atropine 0.3 mg Positive result • • Inject i.v. test dose of edrophonium (0.2 ml-2 mg) Inject remaining (0.8 ml-8 mg) if no hypersensitivity Cranial Neuropathy • • • • Oculomotor (3rd) Cranial Nerve Trochlear (4th) Cranial Nerve Abducen (6th) Cranial Nerve Adult, Child, TITS Anatomy of third nerve Oculomotor nucleus Pituitary gland Red nucleus Carotid artery Cavernous sinus Pons III nerve Post cerebral artery Clivus Basilar artery Applied anatomy of pupillomotor nerve fibres Blood vessels on pia mater supply surface of the nerve including pupillary fibres ( damaged by compressive lesions ) Vasa nervorum supply part of nerve but not pupillary fibres ( damaged by medical lesions ) Pupillary fibres lie dorsal and peripheral Signs of right third nerve palsy • Ptosis, mydriasis and cycloplegia • Normal abduction • Abduction in primary position • Limited adduction • Intorsion on attempted downgaze • Limited elevation • Limited depression Important causes of isolated third nerve palsy Idiopathic - about 25% Vascular disease - hypertension, diabetes Trauma Posterior communicating aneurysm Extradural haematoma Aneurysm Chiasm Midbrain pushed across Edge of tentorium Prolapsing temporal lobe Posterior cerebral artery Third nerve Anatomy of fourth nerve Internal carotid artery Postr. communicating artery III VI Postr.cerebral artery Supr.cerebellar artery Basilar artery IV • • • Only cranial nerve to emerge dorsally Crossed cranial nerve Very long and slender Signs of right fourth nerve palsy • • Right hyperdeviation in primary position when left eye fixating Excyclotorsion • • • Right underaction on depression in adduction Vertical diplopia Right overaction on left gaze Positive Bielschowsky test in right fourth nerve pal Increase in right hyperdeviation on ipsilateral head tilt Absence of right hyperdeviation on contralateral head tilt Anatomy of sixth nerve Basilar artery Medial lemniscus Pituitary gland Carotid artery 4th ventricle Cavernous sinus Petroclinoid ligament Vestibular nucleus Clivus VI nerve Pyramidal tract Old right sixth nerve palsy Straight in primary position due to partial recovery Limitation of right abduction and horizontal diplopia Normal right adduction Important causes of isolated sixth nerve palsy Vascular - hypertension, diabetes Raised intracranial pressure Acoustic neuroma Dilated ventricles Petrous tip Brainstem pushed downwards SUPRANUCLEAR DISORDERS OF EYE MOVEMENT 1. Horizontal gaze palsies • Internuclear ophthalmoplegia • Combined internuclear and PPRF (‘one-and-a-half syndrome’) MLF 2. Vertical gaze palsies • Parinaud dorsal midbrain syndrome • Progressive supranuclear palsy 79 Internuclear ophthalmoplegia Lesion involving left MLF Defective left adduction and ataxic nystagmus of right eye Normal left gaze Convergence intact if lesion discrete Important causes • • • Demylination - usually bilateral Vascular disease Tumours of brainstem ‘One-and-a-half syndrome ’ Combined lesion of left MLF and PPRF Paralytic Pontine Exotropia • Ipsilateral (left) gaze palsy • Defective left adduction • Normal right abduction with ataxic nystagmus Parinaud dorsal midbrain syndrome • Supranuclear upgaze palsy • Large pupils with light-near dissociation • Convergence weakness • Lid retracton (Collier sign) • • Normal downgaze Convergence-retraction nystagmus Important causes • • • In children: aqueduct stenosis, meningitis and pinealoma In young adults: demylination, trauma and a-v malformations In elderly: vascular accidents and posterior fossa aneurysms Progressive supranuclear palsy ( Steele-Richardson-Olszewski syndrome ) • Affects elderly • Pseudobulbar palsy • Extrapyramidal rigidity • Gait ataxia • Dementia Initially involves downgaze Subsequent defective up and horizontal gaze Medial wall blow-out fracture Signs Periorbital subcutaneous emphysema Ophthalmoplegia - adduction and abduction if medial rectus muscle is entrapped Treatment • Release of entrapped tissue • Repair of bony defect COMITANT • • • • • • • • Review History Decompensated Phoria Accomodative Esotropia Acute Esotropia of Childhood Vergence Paresis Skew Deviation Foveal Displacement Syndrome Central Disruption of Fusion Decompensated Phoria • latent ocular misalignment due to lose of single binocular fusion • associated with febrile illness, head trauma, changing refractive needs, asthenopia • presence of adaptive head posture and large fusional amplitudes 86 Refractive accommodative esotropia • • • • Presents between 18 months - 3years Initially intermittent Normal AC/A ratio Excessive hypermetropia Fully accommodative Partially accommodative Esotropia greater for near Straight for distance Straight for distance and near Esotropia for near Non-refractive accommodative esotropia • • • Presents between 18 months to 3years High AC/A ratio - due to increased AC (convergence excess) - due to decreased A (hypoaccommodative) No significant refractive error Signs Straight for distance Esotropia for near Recent right sixth nerve palsy Right esotropia in primary position due to unopposed action of right medial rectus Marked limitation of right abduction due to right lateral rectus weakness Skew Deviation • vertical misalignment of visual axes due to imbalance of prenuclear inputs • vertical diplobia cannot be isolated to a single EOM(s) • Hypertropia varies with gaze associated with downbeat nystagmus • brainstem and cerebellar disease, MS, INO, increased ICP 90 Assessment after photocoagulation Poor involution Good involution • Persistent neovascularization • • Haemorrhage • • Re-treatment required • Regression of neovascularization Residual ‘ghost’ vessels or fibrous tissue Disc pallor Choroidal neovascularization (CNV) • • • Less common than atrophic AMD but more serious Metamorphopsia is initial symptom Most lesions are not visible clinically Suspicious clinical signs Pinkish-yellow subretinal lesion with fluid Subretinal blood or lipid Idiopathic premacular fibrosis Macular pucker Cellophane maculopathy • • Translucent epiretinal membrane Fine retinal striae and mild vascular distortion • Severe retinal wrinkling and vascular distortion • Pucker emanating from epicenter • • Opaque epiretinal membrane May be associated with macular pseudo-hole Recession Resection 95 Summary • • • • • • • What is patient’s real complaint ? Disease process, work up, time frame Trial of prisms Is surgery an option? Are other referrals or treatments necessary? Communication between all parties Evidence-Based Medicine Evidence-based Medicine • “ the conscientious, judicious,explicit use of the best available evidence from clinical care research in making health care decisions” • Harvard Health Policy Review 2007: 8:145-155 Montori and Guyatt: Corruption of the evidence as threat and opportunity for evidence-based medicine 97 VISION THERAPY • 1) Orthoptic VT helpful for convergence insufficiency and binocular function • 2) Behavioral-Perception VT unproven for visual processing and perception • 3) Prevention or correction of Myopia unproven • * Eye excercises do not treat learning disabilities 98 Learning Disabilities • 15-20% of the population affected with reading, math, foreign langauge problems, organizing written and spoken language • reading disorder different from dyslexia • 85% have dyslexia, whereby, loosing place reading due to difficulty decoding letter(s) or word combinations and/or lack of comprehension, not because of a “tracking abnormality” 99 References: • Burde RM, Savino PJ, Trobe JD. Cliinical Decisions in NeuroOphthalmology, 2nd ed. St. Louis: Mosby-Year Book Inc., 1992. • Gorin G, History of Ophthalmology. Delaware:Publish or Perish, 1982 • Miller KM, Capo H, Mallette RA, Guyton DL. Ocular Motility and Binocular Vision. St. Louis: C.V. Mosby Co., 1989. • Pediatric Ophthalmology and Strabismus, Section 6, Basic and Clinical Course. San Francisco: American Academy of Ophthalmology,1990-1. • Taylor D. Pediatric Ophthalmology. Cambridge: Blackwell Scientific Publications, Inc, 1990. • Wright KW. Text Book of Ophthalmology. Baltimore: Williams P. Wilkins, 1997. • Kanski JJ, Bolton A. Illustrated Tutorials in Clinical Ophthalmology. • Butterworth-Heinemann, 2001. • American Orthoptic Journal, Volume 60, 2010 • FocalPoints Advances in the Management of Amblyopia, Kerr,NC 2010 • FocalPoints Practical Management of Amblyopia, Keech,RV Mar 2000 • FocalPoints Diplobia:Diagnosis and Management, Lee,MS Dec 2007 101 102 103