* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download ADI EHDI 2-19-04 version for website and handout
Specific language impairment wikipedia , lookup
Speech perception wikipedia , lookup
Telecommunications relay service wikipedia , lookup
McGurk effect wikipedia , lookup
Evolution of mammalian auditory ossicles wikipedia , lookup
Sound localization wikipedia , lookup
Hearing loss wikipedia , lookup
Olivocochlear system wikipedia , lookup
Noise-induced hearing loss wikipedia , lookup
Sensorineural hearing loss wikipedia , lookup
Auditory processing disorder wikipedia , lookup
Audiology and hearing health professionals in developed and developing countries wikipedia , lookup
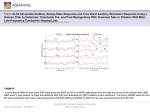
Auditory Dys-Synchrony of Infancy: Best Practices for Diagnosis, Monitoring and Guidance Marilyn Neault, Ph.D., CCC-A February 19, 2004 Thanks to the audiology and otolaryngology staff at Children’s Hospital Boston What is auditory dys-synchrony? • Presence of cochlear hair cell activity - cochlear microphonic in ABR - otoacoustic emissions (may disappear) • Absence of auditory nerve response - no Wave I (no compound action potential) - no ABR waves • Behavioral hearing discrepant from ABR - idiosyncratic, fluctuating responses - audiogram may range normal to profound a.k.a. (also known as…) • • • • Auditory neuropathy Primary auditory neuropathy (Shivashankar) Auditory dys-synchrony Auditory neuropathy “sensu stricto” (Rapin and Gravel) • Peri-synaptic audiopathy • Persistent outer hair cell function (Not all the same – will break down into categories as we learn more) • Your entry? Why do children with auditory dys-synchrony drive audiologists crazy? • Pure tone audiogram and ability to detect sounds in everyday life is often better than the absence of ABR would predict • Word recognition ability is worse than the pure tone audiogram would predict • Functional hearing ability fluctuates and may improve • Expected benefit from hearing aids rarely realized Possible sites of abnormality • Inner hair cells • Synaptic junction between inner hair cells and auditory neurons • Dendrites • Spiral ganglion cells • Axons Heterogeneous disorder with different possible sites Drawing from Takasaka (1993) Other findings in auditory dys-synchrony • Absent acoustic (stapedial) reflexes • OAE’s, if present, are not suppressed by contralateral stimulation • Poor word recognition ability, especially in noise • Poor temporal resolution • Poor low frequency discrimination • Limited or no benefit from hearing aids Concomitant conditions • Half of newborns have NICU histories • One-third of children (80% of adults) have other neuropathies • Sural nerve biopsy may show abnormal myelinization • Charcot-Marie-Tooth (hereditary sensorimotor neuropathy) • Friedrich’s Ataxia • More than one child in family may have auditory dys-synchrony with no concomitant conditions. Mutations in the otoferlin gene may be involved (Varga, J. Med Gen. 2003) “Auditory Dys-Synchrony of Infancy” (“ADI”) • Manifestation of cochlear activity in response to sounds without evidence of neural synchrony, in infancy • Term implies neither etiology nor prognosis Problems with ADI #1. Some get better, some do not, no way (yet) to predict outcome #2. Newborns with auditory dyssynchrony pass OAE screen Parent’s viewpoint • “What kind of a mother would take ‘I don’t know yet if your baby will be able to use his hearing to understand speech’ for an answer?” • Why would they screen newborns with a method that misses my baby’s problem? • Nebulous diagnosis with unknown cause and unknown prognosis • Encourages shopping • Some audiologists not familiar with the condition • Conflicting opinions about use of hearing aids, FM amplification Incidence of auditory dys-synchrony? From Sininger’s literature review: 3.1 / 1000 high risk infants 1/10 children with congenital hearing loss L clicks 20dBHL R clicks 20dBHL L 4000Hz 20dBHL R 4000Hz 20dBHL L 2000Hz 20dBHL L 1000Hz 20dBHL 15ms 20ms R 2000Hz 20dBHL R 1000Hz 20dBHL Typical normal ABR tracings near threshold levels Rarefaction clicks, 90 dBHL Condensation clicks, 90 dBHL 9 month old former 25 week premie, passed newborn OAE screen but parents think she has a hearing loss Rarefaction clicks, 90 dBHL Condensation clicks, 90 dBHL Responses to both polarities superimposed Alternating polarity (CM not observable) Rarefaction clicks, insert phone tubing pinched to check for stimulus artifact 90 dBHL click stimuli 102 dBHL 90 dBHL 80 dBHL 70 dBHL 60 dBHL (Note that the cochlear microphonic does not have a longer latency at lower intensities) Audiogram by Visual Reinforcement Audiometry with insert earphones, on the same day as the ABR. Tympanograms: normal, OAEs: absent bilaterally (though present at newborn screen). Challenge to audiologists: • We need to test in such a way that we’ll see the auditory dys-synchrony of infancy (ADI) • We need to recognize the signs of ADI when they are staring us in the face (a prolonged CM in response to clicks is not just a stimulus artifact!) • We need not to overdiagnose ADI – CM followed by typical ABR waves is not ADI ---we all have cochlear microphonics! – Recognize other reasons why a child might have OAEs but act deaf From an audiologist on a learning curve: • “Because the ABR response did not show polarity inversion when ipsilaterally and contralaterally recorded tracings were superimposed, there is no evidence of auditory neuropathy.” (huh?) From another audiologist on a learning curve: (well, aren’t we all…) • “A polarity-inverting cochlear microphonic response was seen on superimposed rarefaction and condensation click tracings, indicating absence of auditory neuropathy.” (huh?) N3 Potential in a toddler who is deaf May have vestibular origin Not a cochlear microphonic; NOT dys-synchrony Does not reverse polarity Does have a latency-intensity function KNOW THY STIMULUS ARTIFACT Stimulus artifact generated by insert earphone and recorded by ABR electrodes 1000Hz, 100dBHL, single polarity stimulus Overlaid ABR stimulus artifacts from 1000Hz tone bursts, recorded from joined electrodes (no head) and from a profoundly deaf infant. Why did we not see auditory dys-synchrony pre-1990’s? • We did -- we just didn’t know it • Reports of patients with ABR results poorer than behavioral audiogram appeared by 1979 • By mid-1990’s, widespread availability of otoacoustic emissions equipment AND use of insert earphones for ABR testing (insert earphones allow observation of cochlear microphonic response in patients with absent ABR) How do children with auditory dys-synchrony present to the audiology clinic? • Referred on newborn ABR hearing screen • Passed newborn OAE hearing screen but parents suspect child is deaf • A few may have passed ABR screen but then developed auditory dys-synchrony, or had a false negative result on their screen • Toddler with delayed receptive language development seen for VRA (WE NEED TO TEST ACOUSTIC REFLEXES FOR THESE CHILDREN) • Older hearing aid user with fluctuating hearing levels and limited hearing aid benefit for degree of loss Joint Committee on Infant Hearing Year 2000 Position Statement Acknowledges that cases of auditory dyssynchrony may be missed by accepted screening protocols Diagnostic audiology protocol includes ways to detect auditory dys-synchrony Problem: auditory dys-synchrony cases may not reach diagnostic evaluation if screened by OAE What should a UNHS program do about auditory dys-synchrony? • Analyze the consequences of doing automated ABR rather than either ABR or OAE for initial screening? (auditory dyssynchrony passes OAE screen at birth) • Educate audiologists to look for it • Educate early intervention providers: – Nature of parent experience – Typical behaviors of the children – Communication and therapy methods – Approach toward hearing aids and cochlear implant issues Audiological / Educational Management of Infants with Auditory Dys-synchrony • Benefit from visual language system • Encourage speechreading (lipreading) • Some (about 50%) benefit from hearing aids; perhaps in one ear • Beware of hair cell damage from hearing aid amplification, at least while OAEs are present • Consider sound field FM amplification • Language stimulation in quiet background; acoustic highlighting • Monitor behavioral audiogram and OAEs; “hearing” may improve or decline Try a hearing aid or not? • Beware of hair cell damage if OAEs are still present. Presence of OAEs suggests normal cochlear amplifier function. • If OAEs have disappeared, try testing speech perception in each ear separately at elevated intensities. If the child understands words better at a higher than conversational intensity, try a hearing aid in that ear (or ears). Audiological / Educational Management of Infants with Auditory Dys-synchrony, continued • Let parents know that a cochlear implant may help, if hearing does not improve and hearing aids don’t help • Help connect parents with other parents of children with the same condition Auditory Neuropathy Information Homepage (with links including parent listserv) http://auditoryneuropathy.com Why might a CI help a child with auditory dys-synchrony? • The child’s auditory nerve cells do not fire in tempo with incoming sounds. • The cochlear implant may act as a drill sergeant for auditory nerve fibers, stimulating them to fire in synchrony and to keep tempo with incoming sounds. “Problem solving is an important skill in any professional, yet it can be counterproductive if applied too early in a goalsetting endeavor, especially if done for the family rather than with them.” D. Bailey Typical candidacy to benefit from a cochlear implant • Age 12 months and up with profound bilateral hearing loss • OR age 25 months and up with severe or profound hearing loss and poor ability to recognize words through hearing aids “profound” means average hearing thresholds >90dBHL at 500, 1000 and 2000Hz, unaided; “severe” means 70-90dBHL, unaided; “poor” means no more than 30% correct repetition of one-syllable word list without clues at 57dBHL, with terrific hearing aids Cochlear implant candidacy for a child with auditory dys-synchrony • Same as “typical” candidacy EXCEPT: – Allow enough time to know whether hearing will improve or even recover – Pure tone hearing levels are not the determining factor; a child may show a mild-moderate loss on the audiogram but may still benefit from a cochlear implant, if the child can not learn to recognize words without looking – Assess the reason for the condition, to assess the risk that the auditory nerve is truly “pathological” or may deteriorate in function over time Is anything different about the CI candidacy workup for a child with auditory dys-synchrony? • Should have MRI of the inner ears / auditory nerve (not just a CT scan). Consider MRI of the whole brain as well. • Should be evaluated by a neurologist for other peripheral neuropathies • Should monitor functional use of hearing in case ADI is resolving • Should have ABR, OAE, acoustic reflex tests repeated just prior to surgery • Consider Auditory Steady State Response (ASSR) to assist in ear determination • As for any CI candidate, parents should accept that outcomes are variable and not always predictable. What do you have to lose? (by implanting a child with auditory dys-synchrony) • Ability to hear in the implanted ear when not using the speech processor • Ability to determine the extent to which hearing may improve or resolve on its own • Any ability the child might have had to localize the direction of a sound source What do you have to gain? (by implanting a child with auditory dys-synchrony) • Likelihood of auditory synchrony on one side • Likelihood of stable hearing • Potential to learn to recognize spoken words and sentences in quiet without looking • Byproducts of better hearing: better speech and better language Why might someone with auditory dys-synchrony have a particularly good CI outcome? • Language base in visual language system prior to CI; may not have been severely language-deprived prior to implant. • Has had and will have intense therapy and vigilant attention to communication. • Most have had some auditory experience prior to implant. • ?? May have cellular or neural elements in the cochlea in better supply than in some types of sensorineural hearing loss?? Why might someone with auditory dys-synchrony have a particularly limited CI outcome? • Cochlear implant may not succeed in driving the auditory nerve fibers to fire in synchrony. • If a degenerative nerve condition is present, such as in some mitochondrial disoders, performance with the CI could decline over time. • Child may have other challenges which would have made it difficult for him to learn to understand speech and to speak, even if he had had normal hearing. Before and after CI with auditory dys-synchrony BEFORE Pure tone audiogram mild to profound, fluctuating, moderately severe most common. No nerve action potential (Wave I). No ABR response. No acoustic reflexes. AFTER Sound field pure tone audiogram predictable at about 30dBHL, 2506000Hz. Nerve action potential seen on neural response telemetry. EABR response + Acoustic reflex stimulable using cochlear implant. vV Electrically evoked Auditory Brainstem Response stimulated through the cochlear implant in the operating room Electrically elicited acoustic reflex stimulated by presenting a signal through the cochlear implant Models of auditory dys-synchrony • Temporal bones of expired premies with outer hair cells but no inner hair cells (Amatuzzi et al., Arch. Oto. HNS 2001) • Carboplatin causes selective loss of inner hair cells (but have acoustic reflexes) • Mouse strain with no inner hair cells • Mouse strain with early degeneration of cells that support the spiral ganglion cells Research questions: • Need better way to differentiate which cases will improve or resolve – Catalog and monitor our series • Serial test measures • Infant auditory development scales – Additional electrophysiological measures? • Some patients have ASSR and some have cortical auditory evoked potentials, despite absence of ABR Research questions • Can people with auditory dys-synchrony localize sound? • Does ABR or ASSR improve as pure tone audiogram and functional use of hearing improve? • Is true resolution possible? (study “resolved” cases for acoustic reflexes, gap detection, discrimination in noise) • Performance with cochlear implants • What happens to the unimplanted ear over time? Neault and Kenna (study in progress, 2004) Subjects: • 50 children with ADI whose hearing loss was evident during the first few months of life, seen at Children’s Hospital Boston • Excluded: later onset auditory dyssynchrony Unilateral vs. Bilateral Of 50 children with ADI as of 2/04, 40 (80%) with bilateral ADI (14 of these now have cochlear implants) 8 (16%) with one ear ADI, one ear normal hearing 2 (4%) with one ear ADI, one ear typical sensorineural hearing loss (one now has a cochlear implant) How They Came to Us (N = 50) • 30: Followup for newborn ABR screen referral • 6: Passed newborn OAE but parents suspected deafness (dx’d at 6-27 months) • 3: Passed newborn ABR screen but suspected deaf within first few months of life (two a real pass, ? one bogus) • 6: Not screened; parents suspected hearing loss • 5: Newborn screening data not confirmed Characteristics of 50 Children with ADI • Of 23 who had CT and/or MRI of inner ears so far, 5 showed abnormalities of cochlea or nerve (2 have normal cochlear turns, stenotic IAC, no cochlear nerve) • 1 has optic nerve hypoplasia • 9 have abnomalities on MRI of brain What Happened to the 50 Children So Far • 14 with bilateral ADI now have cochlear implant • 1 with unilateral ADI, unilateral typical SNHL now has a cochlear implant • 6 with bilateral ADI resolved to normal hearing findings • 29 “other” (some still very young, some planning implantation, some developing usable but not normal hearing, all receiving habilitation, nearly all have at least somevisual language support) Cochlear Implant Group (the first 11 of those implanted) • Preoperative hearing levels: ranged from moderately severe to profound; poorer ear implanted • Age at implantation: Median 22 months Mean 30 months Range 14 to 62 months Cochlear Implant Group (N = 11) • Progress typical of children with cochlear implants • Progress commensurate with their developmental abilities • Those who are developmentally able to demonstrate open set speech recognition have done so Cochlear Implant Group: What Happened to the Unimplanted Ear? • One improved from very profound to severe by age 42 months • Two dropped from severe to profound range, one at age 2 years and one at age 4 years • One uses hearing aid consistently in unimplanted ear • One uses hearing aid sporadically in unimplanted ear • None have word recognition ability beyond pattern perception in the unimplanted ear Caveat Implantor • Does the child have a cochlear nerve? ( One child with unilateral and one child with bilateral ADI in our series showed absence of cochlear nerves ) Caveat Implantor • Six of 50 children with ADI in our series resolved to NORMAL behavioral and/or electrophysiological measures of hearing • All six showed signs that their hearing was improving (behaviorally or electrophysiologically) by 12 months of age, but you had to look for it Resolved ADI • 2 sisters with no other conditions • 1 boy with hyperbilirubinemia (to 44) • 1 boy whose mother had viral meningitis during pregnancy • 1 boy whose mother had Lyme disease and had Bell’s Palsy 4 days before delivery; baby negative for Lyme • 1 boy who was a 35 week premie, HIFI vent • All had maintained robust OAEs Resolving auditory dys-synchrony Sibling of girl with resolved ADI Age 3 weeks: no ABR waves, robust OAEs Mother: “She acts deaf the way her sister did.” Age 3 months: Wave V present 80dB +, no reflexes Age 14 months: Normal behavioral audiogram Age 30 months: Normal audiogram, reflexes present AU, 92% PBK score in each ear FREQUENCY IN HERTZ (Hz) 125 250 500 750 1000 1500 2000 3000 4000 6000 8000 KEY -10 R L HEARING LEVEL (HL) IN DECIBELS (dB) 0 AC (AIR) 10 20 30 X X X X Age 26 months 60 70 80 DPOAE: robust AU Tympanograms: normal 90 100 110 120 UNMASKED MASKED BC (BONE) UNMASKED 40 50 X Ipsilateral acoustic reflexes: normal AD, absent AS MASKED SOUND FIELD S SPEECH AUDIOMETRY R L SDT SRT SPEECH DISCRIM. (WORD RECOG.) 20 20 92% in SF (ESP Monosyl.) One month old boy with peak bilirubin 44. By five months, he had ABR waves down to 30dB left and 20dB right, only at slow stim. rate. By 14 months, ABR waves down to 20dB in each ear; morphology best at slow rate. LEFT Clicks 20dBHL RIGHT Clicks 20dBHL 4000Hz 20dBHL 4000Hz 20dBHL 2000Hz 20dBHL 2000Hz 20dBHL 1000Hz 20dBHL 1000Hz 20dBHL Resolved ADI. ABR of 17 month old boy who had no ABR waves at birth. Still has some difficulty localizing sound. LEFT Clicks 90dBHL Clicks 20dBHL RIGHT Clicks 90dBHL Clicks 20dBHL Same 17 month old with resolving ADI; cochlear microphonic remains unusually large. What about children whose ADI does not “resolve” but they do develop usable hearing? 25 week premie; still no ABR waves at 2 yrs. 8 months Speaks in clear 4-word sentences. Uses MicroEar BTE FM in mainstreamed preschool; comprehends speech well. Some typical things that partially hearing toddlers and preschoolers with auditory dyssynchrony do • Respond to intonation • Talker-specific understanding • Localize sounds poorly • Develop articulation out of the usual order for sensorineural hearing loss – Vowel distortions (poor low freq discrimination) – May have unvoiced plosives in their speech and be able to imitate them • May benefit inconsistently from hearing aids How can a child with no ABR synchrony develop “hearing?” Perhaps … “…The brain ingeniously builds an accurate clock from an enormous number of sloppy ones….” --Steven Strogatz (2003) SYNC: The Emerging Science of Spontaneous Order (Strogatz, 2003) “ ….Left to their own devices, this motley bunch of neural oscillators would fire off impulses at disparate rates, producing an electrical racket akin to the sound of an orchestra tuning up before a performance. To work together as an accurate clock, these hypothetical oscillators would need to cooperate, to sense one another’s electrical rhythms so as to stay in step.” Conclusions Regarding Auditory Dys-Synchrony of Infancy (ADI) • Infants with ADI are not always good implant candidates – 2/50 had no cochlear nerve – 6/50 resolved – A few will develop enough usable hearing that CI surgery may not be necessary – Those who prove to be good candidates benefit greatly from cochlear implantation, in a manner typical of other deaf children with the same cognitive abilities and pre-implant language base Conclusions Regarding Auditory Dys-Synchrony of Infancy (ADI) • Those who are going to resolve start developing ABR waves by 12 months • BUT you have to look for it; may need to slow the stimulus repetition rate • Repeat ABR and monitor functional hearing again just before early CI surgery for a child with auditory dyssynchrony Additional Thoughts • Children with “resolved” ADI missed out on a few months of good hearing and should not be cut off from early intervention • Parents may have much invested in acceptance of hearing disorder • Children may still have subtle auditory disorders and should be watched