* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Tissue: The Living Fabric
Embryonic stem cell wikipedia , lookup
Cell culture wikipedia , lookup
Wound healing wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Chimera (genetics) wikipedia , lookup
Cell theory wikipedia , lookup
Neuronal lineage marker wikipedia , lookup
Nerve guidance conduit wikipedia , lookup
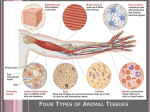
Human embryogenesis wikipedia , lookup
Tissue: The Living Fabric Chapter 4 Chapter Outline Epithelia Tissue Connective Tissue Epithelial Membranes Nervous Tissue Muscle Tissue Tissue Repair Developmental Aspects of Tissue Introduction to Tissue The human body is a multicellular organism – Its cells form tight communities that have similar functions – Cell specialization allows for division of labor – However, the risk is that loss of specialized cells means the loss of that function and potentially the individual Tissue Groups of closely associated cells that are similar in structure and function are called tissues Four primary tissues interweave to form the “fabric” of the body – – – – Epithelial Connective Muscle Nervous (covering) (support) (movement) (control) Organs Tissues are organized into organs – Most organs contain all four tissue types – However, most organs will have one predominant tissue type present – The arrangement and proportion of tissues present determines the function of the organ SECTION I EPITHELIAL TISSUE Epithelial Tissue Epithelial tissue is a sheet of cells that covers a body surface, a body cavity, or has a glandular function Epithelia form the boundaries between environments Epithelial has many functions including; protection, absorption, filtration, excretion, secretion, and sensory reception Special Characteristics of Epithelium Cellularity Epithelial tissue is composed almost entirely of close packed cells with little extracellular material lying in the space between them Specialized Cells form continuous sheets. contacts Adjacent cells are bound together at many points by lateral contacts including, tight junctions and desmosomes Junctions & Desmosomes Tight junctions occur where protein molecules in adjacent cells fuse together to form an impermeable junction Desmosomes are anchoring junctions that bind adjoining cells and prevent their separation Gap Junctions Gap junctions allow chemical substances to pass to adjacent cells Cells connected by hollow connexons Found in electrically excitable tissues (heart and smooth muscle) Ion passage from one cell to another helps to synchronize electrical activity Special Characteristics of Epithelium Polarity – All epithelial tissue has an apical surface exposed to the body exterior or an internal cavity – All epithelia exhibit polarity where the cells near the apical surface differ from those at the basal surface – Apical surfaces can be smooth, most have microvilli, and some have cilia – The basal surface of epithelium is called the basal lamina, which acts as a selective filter that determines which molecules are allowed to enter the epithelium Special Characteristics of Epithelium Supported by connective tissue – All epithelial tissue sheets rest upon and are supported by connective tissue – Deep to the basal lamina is the reticular lamina, a layer of extracellular material containing a fine network of collagen fibers from the underlying connective tissue – Together the basal and reticular lamina form the basement membrane – The basement membrane reinforces the epithelial sheet enabling it to resist stretching and tearing – It also defines the epithelial boundary Special Characteristics of Epithelium Innervated but avascular – Epithelial tissues are supplied with nerve cells – Epithelial tissues contain no blood vessels • Epithelial tissue receive nutrients by substances diffusing from blood vessels in the underlying connective tissue layers Special Characteristics of Epithelium Regeneration – Epithelial cells have a high regenerative capacity – Epithelial cells are exposed to friction, others are damaged by hostile substances in their environment – If nourished adequately, epithelial tissue can replace lost cells rapidly by cell division Classification of Epithelia Each epithelium is given two names: – The first name references the number of epithelial cell layers present • Simple • Stratified – The second name describes the shape of the cells present in the epithelial cell layer • Squamous • Cuboidal • Columnar Simple and Stratified Epithelium Simple epithelium is composed of a single tissue layer – It is usually found where absorption and filtration occur, thus a thin layer facilitates these processes Stratified epithelium consists of two or more layers stacked one upon the other – It is usually found in areas of high abrasion and functions to protect underlying cell layers Epithelial cells All epithelial cells are hexagon shaped This shape allows the cells to be tightly packed with little wasted space Epithelial cells look like a honeycomb Epithelial cells vary in height and are named on the basis of shape – Squamous cells are flattened and scalelike – Cuboidal cells are boxlike in appearance – Columnar cells are tall and column shaped Epithelial shape Squamous - flat and scale-like Cuboidal - boxlike Columnar - tall and column shaped Simple Epithelia All the cells in the layer have the same shape There are four major classes of simple epithelia – – – – Simple squamous Simple cuboidal Simple columnar Pseudostratified columnar (Highly modified simple epithelium) Stratified Epithelia There are also four major classes of stratified epithelia – – – – Stratified squamous Stratified cuboidal Stratified columnar Transitional epithelium (a modified stratified squamous epithelium) Simple Squamous Epithelium The simplest form of epithelium A single layer of flattened cells Thin and permeable, this type is often found where filtration or diffusion is a priority Two simple squamous epithelium have special names related to their location – Endothelium (lining blood vessels) – Mesothelium (found in serous membranes) Simple Epithelia Simple Squamous Epithelium Simple squamous epithelium forming walls of alveoli (air sacs) of the lung Simple Epithelium: Simple Cuboidal Epithelium Single layer of cube like cells Important functions are secretion and absorption It forms ducts and secretary portions of small glands Simple Epithelium: Simple Cuboidal Epithelium Simple cuboidal epithelium in kidney tubules Simple Epithelium: Simple Columnar Epithelium Consists of a single layer of tall, closely packed cells Important functions are secretion and absorption In glands it forms the secretory portion of the gland and portions of the ducts Simple Epithelia: Simple Columnar Epithelium Consists of a single layer of tall cells – unciliated in the digestive tract • associated with absorption and secretion • mircovilli add surface area and aid absorption • globlet cells secret protective lubricants – ciliated in the respiratory passages • cilia “sweep” or propel mucus by ciliary action Simple Epithelium: Simple columnar epithelium Simple columnar epithelium of the stomach mucosa Simple Epithelium: Pseudostratified Columnar Epithelium Single layer of cells of differing heights The cell nuclei are located at differing levels above the basement membrane giving the false (pseudo) impression of multiple cell layers Ciliated in the upper respiratory tracts Nonciliated in large body ducts Simple Epithelium: Pseudostratified Epithelium Pseudostratified ciliated epithelium lining the human trachea Stratified Epithelium: Stratified Squamous Epithelium Thick membrane composed of several cell layers Surface cells are flattened (squamous) while deeper cell layers are cuboidal Surface cells are full of keratin and dead, while basal cells are alive and active in cell mitosis Protective in function, these cells are found in areas subjected to abrasion Stratified Epithelium: Stratified Squamous Epithelium Stratified squamous epithelium lining the esophagus Stratified Epithelium: Stratified Cuboidal Epithelium Generally two layers of cube-shaped cells Form large ducts of some glands Function to protect Relatively rare tissue type Stratified Epithelium: Stratified Cuboidal Epithelium Stratified cuboidal forming a salivary duct Stratified Epithelium: Stratified Columnar Epithelia Several Cell layers present Basal cells are cuboidal while superficial cells are columnar Rare in the body; found in the large ducts of some glands and in the male urethra Functions include protection and secretion Stratified Epithelium: Stratified Columnar Epithelium Several cell layers thick Rare in the body it is found in large ducts and the male urethra Functions are to provide protection and secretion Stratified Epithelium: Stratified Columnar Epithelium Stratified columnar epithelium lining the male urethra Stratified Epithelium: Transitional Epithelium Forms the lining urinary organs Resembles both stratified squamous and cuboidal The cells vary in appearance depending on the degree of distension of the organ The ability of the epithelium to thin under pressure allows for a greater volume of urine Transitional Epithelium Transitional epithelium lining of the bladder, relaxed state Glandular Epithelia A gland consists of one or more cells that make a secretion Secretions are usually water based fluids containing proteins Glands are classified by route of secretion: – endocrine – exocrine (internal secretion) (external secretion) Glands are classified by number of cells: – unicellular exocrine glands – multicellular exocrine glands Endocrine Glands All endocrine glands eventually lose their ducts and are considered to be ductless Endocrine glands produce hormones that regulate body functions These glands secret directly into the extracellular space The hormones then enter the blood or lymphatic fluid – Pituitary, Thyroid, Parathyroid, Adrenal, Thymus,, and others Exocrine Glands Exocrine glands are far more numerous than endocrine These glands secret their products through a duct onto a body surface or into a body cavity These glands secret mucous, sweat, oil, saliva, bile, digestive enzymes, and many other substances Multicellular Exocrine Glands Multicellular exocrince glands have two common structural elements – An epithelium derived duct – A secretory unit consisting of secreting cells In all but the simplest glands connective tissue surrounds the secretory unit supplying it with blood an nerve fibers Often the connective tissue forms a fibrous capsule and may subdivide the gland into lobes Glandular Epithelium: Multicellular Exocrine Glands There are two categories of Multicellular glands based on their duct structures – Simple glands have an unbranched duct – Compound glands have a branched duct The glands are also described by the structure of their secretory parts (tubular, alveolar or tuboloalveolar) The glands are also described by the way a gland secrets its products (merocrine, holocrine, aprocrine) Glandular Epithelium: Modes of Secretion Merocrine glands (salivary) – Secret their products by exocytosis Holocrine glands (sebaceous) – The entire cell ruptures releasing the secretions Apocrine glands (mammary) – The apex of the secretory cell pinches off and release its secretion Chief Modes of Secretion Mode of Secretion: Apocrine Unicellular Exocrine Glands These are single cells interposed in an epithelial sheet between cells with other functions These glands produce mucin which dissolves in water to form mucus These cells are secreted by the goblet cells of the respiratory and digestive tracts Goblet cells Found in columnar epithelium cells lining the intestinal and respiratory tract CONNECTIVE TISSUE SECTION II Connective Tissue: An Introduction Connective tissue is found everywhere in the body but the proportion present in a tissue varies Its major functions are: – – – – support and binding protection insulation transportation Common Characteristics Common origin – All tissue arise from mesenchyme layer Varying degrees of vascularity – Tissue vary from rich vascular supply to avascular Extracellular matrix – The living cells are widely distributed within a matrix of nonliving substances – The matrix creates the ability to bear weight, withstand tension, and abrasion Connective Tissue: Model Structural Elements Any connective tissue is made up of three elements; ground substance, fibers, and cells The composition and arrangement of extracellular elements yields the diversity of connective tissues It can be delicate and fragile, or thick, dense and strong Ground Substance Ground substance is an unstructured material that fills the space between cells and contain the fibers It is composed of interstitial fluid, cell adhesion proteins, and proteoglycans The ground substance holds fluid and functions as a medium through which nutrients and substances can diffuse between blood vessels and cells Adhesion Proteins Adhesion proteins serve as the “glue” that allows connective tissue cells to attach to matrix elements Adhesion proteins include: – Fibronectin – Laminin Proteoglycans Proteoglycans consist of a protein core to which (GAGs) attach GAG’s (glycoaminoglycans) are large, negatively charged polysaccharides that attach to the core protein The polysaccharides trap water and determine the properties of the matrix The matrix may vary from fluid to a semi stiff gel Connective Tissue: Fibers The fibers within connective tissue provide support Three type of fibers are found in connective tissue matrix – Collagen – Elastic – Reticular Collagen Fibers Collagen fibers are extremely tough and have a high tensile strength Fibers are able to withstand great longitudinal stresses Collagen fibers align along lines of stress Collagen fibers are located wherever support is needed to reinforce an organ or joint Elastic Fibers Elastin has a randomly coiled structure that allows it to stretch and recoil Elastin in the matrix gives it a resilient quality Collagen fibers limit distension of the tissue and elastin fibers return the tissue to its normal length and shape Found where elasticity is needed – Skin, lungs, walls of blood vessels Reticular Fibers Fine collagen fibers Form branching networks of delicate fibers that surround blood vessels and support soft tissue of organs Very apparent where connective tissue abuts other tissue types – Basement membranes of epithelial cells Connective Tissue: Cells Each major class of connective tissue has a fundamental cell type Active mitotic cells are called blasts which implies a forming cell The primary cells types of connective tissue are: – – – – fibroblast - connective tissue chondroblast - cartilage osteoblast - bone hemocytoblast - blood Cells (con’t) Once the blast cells have synthesized the matrix they become less active and are referred to (chrondocyte) Mature cells maintain the health of the matrix If the tissue is damaged they become active to repair and regenerate the matrix Cells (con’t) Connective tissue also harbor an assortment of other cell types – white blood cells - infection – mast cells - detect foreign substances – macrophages - phagocytize a broad variety of foreign molecules and bacteria Connective Tissue: Mesenchyme Mesenchyme tissue is the first tissue formed from the mesodermal germ layer It is made up of star shaped mesenchymal cells It is a gel-like ground substance containing fine fibers During embryonic development other tissues differentiate from it Mesenchyme Mesenchyme Connective Tissue: Connective Tissue Proper Loose Connective Tissue – Areolar – Adipose – Reticular Dense Connective Tissue – Dense Regular – Dense Irregular – Elastic Areolar Connective Tissue A gel-like matrix with a loose arrangement of all three fiber types Contains cells, fibroblasts, macrophages, mast cells, and some white blood cells Because of the loose nature of the tissue it serves as a reservoir for water and salt for the surrounding tissues Areolar: Location Most widely distributed type of connective tissue Serves as the universal packing material between tissues Packages organs Surrounds capillaries Forms subcutaneous tissue Present in all mucus membranes Areolar Tissue Areolar Tissue: Function Wraps and cushions organs Macrophages phagocytize bacteria Plays important role in inflammation Holds and conveys fluid Areolar Tissue Adipose (fat) Tissue Adipose tissue is basically areolar connective tissue in which the nutrient storing functioning is greatly increased Adipocytes predominate tissue as little matrix is present Oil (fat) occupies most of cell volume Compression of the cell nucleus to one side gives it a name of “signet” cells Tissue is richly vascular owing to high metabolic activity Adipose Tissue: Location Under skin Around kidneys and eyeballs In bones Within abdomen Within breasts Adipose Tissue Adipose Tissue: Function Provides reserve food source for fuel Insulates against heat loss Supports and protects organs Adipose Tissue Reticular connective tissue Reticular connective tissue resembles areolar tissue, but the only fibers in the matrix are reticular Fibers form a delicate internal network along which fibroblasts are distributed Widely distributed in the body, the tissue provides internal support for many lymphocytes within lymphatic tissues such as lymph nodes, the spleen, and bone marrow Reticular Connective Tissue: Location Lymphoid organs – Lymph nodes – Bone marrow – spleen Reticular Connective Tissue Reticular Connective Tissue: Function Fibers form the soft internal skeleton (stroma) that supports other cell types Supports many free blood cells in lymphatic tissue Reticular Connective Tissue Dense Regular Connective Tissue A type of connective tissue consisting of dense bundles of collagen fibers Collagen fibers are arranged in parallel that lie in the direction of pull or stress Great resistance to tension Slightly wavy alignment allows for some degree of stretch Has few other cells and is poorly vascularized Dense Regular Connective Tissue: Location Dense regular connective tissue forms: – Tendons – Aponeuroses – Ligaments Muscle to bone Muscle to muscle or bone Bone to bone Ligaments have a little stretch, tendons very little Dense Regular Connective Tissue Dense Regular Connective Tissue: Function Attaches muscle to bones or to muscles Attaches bones to bones Withstands great tensile stress when pulling force is applied in one direction Dense Regular Connective Tissue Dense Irregular Connective Tissue Same structural components as regular variety Dense bundles of collagen fibers are thicker and arranged with fibers flowing in more than one plane Fibers form sheets of tissue that cope with tension from a variety of directions Dense Irregular Connective Tissue: Location Dermis of the skin Submucosa of digestive tract Fibrous capsules of organs and joints Dense Irregular Connective Tissue Dense Irregular Connective Tissue: Function Able to withstand tension exerted in many directions Provides structural strength to many diverse tissues and organs Dense Irregular Connective Tissue Cartilage Has qualities that intermediate between dense connective tissue and bone It is tough but flexible, providing a resilient rigidity to the structure it supports Cartilage is avascular and devoid of nerve fibers Ground substance contains large amounts of GAG, a major adhesion protein Cartilage continued Ground substance contain many collagen fibers and in some cases elastic fibers to yield a substance that is quite firm Cartilage matrix is approximately 80%water Movement of tissue fluid in its matrix enables cartilage to rebound after being compressed Movement of tissue fluid helps to nourish cartilage cells Cartilage continued The surfaces of most cartilage structures are surrounded by a well vascularized dense irregular tissue membrane called a perichondrium Nutrients diffuse from the perichondrium to the matrix and then to the chondrocytes Cartilage continued Chondroblasts in growing cartilage produce new matrix that becomes bone – During interstitial growth chondroblasts secrete new matrix to form the cartilage piece from which a bone will develop – During appositional growth chondroblasts secrete new matrix on the superficial surface of the cartilage structure The firm cartilage matrix prevents the cells from becoming widely separated Hyaline Cartilage Hyaline cartilage contains large amounts of collagen fibers formed in an imperceptible network Hyaline cartilage provides firm support with some pliability It has resilient properties that resist compression Matrix appears blue-white with a smooth almost slick surface Hyaline Cartilage: Location Forms most of the embryonic skeleton Covers the ends of long bones in joint cavities Forms costal cartilages of the ribs Cartilages of the nose, trachea, and larynx Hyaline Cartilage Hyaline Cartilage: Function Supports and reinforces with some pliability Has resilient cushioning properties Resists compressive stress Hyaline Cartilage Elastic Cartilage Similar to hyaline cartilage but with more elastic fibers in the matrix Elastic fibers gives this tissue greater resilience to repeated bending Found where the tissue supports the shape of the structure while allowing great flexibility Elastic Cartilage: Location Supports the external ear Epiglottis Elastic Cartilage Elastic Cartilage: Function Maintain shape of structure while allowing great flexibility Elastic Cartilage Fibrocartilage Consists of alternating rows of thick collagen fibers Matrix is similar to hyaline cartilage but less firm It is compressible and resists tension well Located where strong support and the ability to withstand heavy pressure is required Fibrocartilage: Location Intervertebral disks of the vertebral column Pubic symphysis Disks of knee joint Fibrocartilage Fibrocartilage Bone Bone matrix is similar to that of cartilage but is harder and more rigid Differs from cartilage in that it contains more collagen fibers and an added matrix element of inorganic calcium salts Osteoblasts produce the matrix then bone salts are deposited on and between fibers Well supplied with blood vessels Bone: Location All structural elements of the skeletal system Appears as long, flat, short, and irregular bone Includes compact and spongy bone Bone Bone: Function Supports the weight of the body Protects vital organs and structures Provides levels for muscles to act upon Stores calcium, other minerals, and fat Bone marrow is the site for blood cell formation Bone Blood Classified as a connective tissue because it consists of blood cells surrounded by a nonliving matrix The fibers of blood are soluble protein molecules that become visible only during blood clotting Blood: Location Contained within blood vessels of the circulatory system Blood Blood: Function Transport vehicle of the circulatory system Carries nutrients, wastes, respiratory gases, and many other substances throughout the body Blood EPITHELIAL MEMBRANES SECTION III Epithelial Membranes: Epithelial membranes incorporate both connective and epithelial tissues Epithelial membranes are a continuous multicellular sheet composed of at least two primary tissues Can be considered a simple organ The three common forms of epithelial membranes are cutaneous, mucous, and serous Cutaneous membrane It is an organ system consisting of ketatinized stratified squamous epithelium attached to a layer of dense irregular connective tissue A dry membrane Mucous membranes Mucosae line body cavities that are open to the exterior These are moist membranes bathed by secretions Often adapted for absorption and secretion Epithelial Membranes: Serous membranes Moist membranes found in the central body cavities Each consists of a parietal and visceral layer Serous fluid lubricates the two layers NERVOUS TISSUE SECTION IV Nervous Tissue Nervous tissue makes regulates and controls body functions Neurons are highly specialized cells that generate and conduct nerve impulses Support cells are nonconducting tissue that support, insulate and protect the delicate neurons Nervous Tissue: Location Brain and spinal cord of the central nervous system (CNS) All cranial and spinal nerves of the peripheral nervous system (PNS) Nervous Tissue Nervous Tissue: Function Transmit electrical signals from sensory receptors to the brain Brain interprets impulse for potential response Signals from brain to effectors (muscles and glands) control response MUSCLE TISSUE SECTION V Muscle Tissue: Muscle tissues are highly cellular, wellvascularized tissue responsible for most types of body movement Muscle provides contractile force by shortening their elongated shape Muscle cells possess myofilaments The three kinds of muscle tissue are skeletal, cardiac and smooth Skeletal muscle Skeletal muscle is wrapped by connective tissue into organs called muscles which attach to bones As skeletal muscle contracts it causes gross body movements Skeletal muscle is identified by its long cylindrical form and obvious striations Voluntary control Skeletal muscle: Location Skeletal muscle attach to bones of the skeletal system Occasionally muscle will attach to skin Skeletal Muscle Skeletal Muscle: Function Produces movement – Locomotion – Manipulation of the environment – Facial expression Maintains posture Stabilizes joints Generates heat Skeletal Muscle Cardiac muscle Occurs in the walls of the heart and no where else in the body Muscle cells are striated Uninucleate cells fit together at unique junctions called intercalated discs Cardiac muscle: Location Found only in the myocardium of the heart Cardiac Muscle Smooth muscle Smooth muscle is so named because its fibers have no visible striations Spindle shaped muscle cells contain one centrally located nuclei Closely arranged to form sheets Smooth muscle: Location Occurs mainly in the walls of hollow organs – digestive tract – blood vessels Smooth Muscle Smooth muscle: Function Act to propel substances or objects along internal passageways – Food – Urine – Baby Involuntary control Long, sustained contractions Smooth Muscle TISSUE REPAIR SECTION VI Tissue Repair Tissue repairs requires cells to divide and migrate in response to hormones released by damaged cells Tissue repair occurs in two major ways: by regeneration and by fibrosis Which healing process to occur depends upon: – The type of tissue damaged – The extent of the injury Tissue Repair Regeneration is the replacement of destroyed tissue with the same kind of tissue Fibrosis involves the proliferation of fibrous connective tissue called scar tissue Tissue Repair: Inflammation Inflammation of injury due to release of histamine Capillaries dilate, become permeable White blood cells, antibodies, clotting proteins arrive Clotting isolates injured area Tissue Repair: Organization Blood clot replaced by granulation tissue Capillary buds invade area Fibroblasts secret collagen fibers Macrophages digest and remove dead cells Tissue Repair: Regeneration Surface epithelium begins to regenerate Granulation tissue is replaced by epithelium Fibrosed area is found deep to epithelium Scar may not be evident Factors Affecting Tissue Repair The type of tissue injured Type of injury and the immediate care received Nutrition Adequacy of blood supply State of health of the individual Age of the individual Tissue Repair: Tissue Type Epithelial tissues regenerate very well Bone and fibrous tissue heal quite well Smooth muscle and dense regular connective tissue have very limited capacity for regeneration Skeletal muscle and cartilage regenerate poorly Cardiac and nerve tissue have no regenerative capacity and are replaced by scar tissue DEVELOPMENTAL ASPECTS OF TISSUES SECTION VII Developmental Aspects of Tissue One of the first events of embryonic development is the formation of the three primary germ layers These three germ layers are the ectoderm, mesoderm and endoderm These primary germ layers begin to form the four primary tissues from which all body organs are derived Tissue Origins Epithelial tissue are formed from all three tissue layers Muscle and connective tissue form from the mesoderm Nervous tissue forms from the ectoderm Embryonic Germ Layers Cell Development By the end of the second month of development, the primary tissues have appeared, and all major organs have been laid down Tissue growth continues on at a rapid rate throughout the embryonic and fetal periods Most tissues cells except neurons continue to undergo cell mitosis until adulthood Adulthood In adulthood only epithelia and blood forming tissue are highly mitotic With increasing age the amount of collagen decreases making tissue repair less efficient Declining circulatory efficiency results in less nutrient delivered to tissue Dietary choices also influences tissue repair TISSUE: THE LIVING FABRIC END OF CHAPTER