* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Calcium and its significance in the bone metabolism
Survey
Document related concepts
Transcript
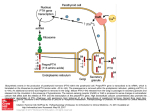
Calcium and its significance in the bone metabolism Romana Šlamberová, MD PhD Department of Normal, Pathological and Clinical Physiology CALCIUM 2% of body weight 99% in bones 1% in body fluids Plasma (Extracellular fluid) 2.25 – 2.75 mmol/l Cell (Intracellular fluid) 10-8 – 10-7 mol/l = 10-5 – 10-4 mmol/l PLASMA CALCIUM diffusible 48% (50%) Ca2+ ionized 6% (10%) combined with anions (citrate, phosphate) – non-dissociated nondiffusible 46% (40%) combined with plasma proteins combination with proteins depends on pH 0.2 mmol/l Ca2+ on each pH unit ROLE OF CALCIUM excitability of cell membranes neuromuscular transmission and muscle contraction releasing of transmitters from synapses “second messenger” stimulates secretory activity of exocrine glands and releasing of hormones contractility of myocard blood coagulation PHOSPHATES 80% bones and teeth 10% blood and muscles 10% different chemical complexes Plasma (ECF) 0.65 – 1.62 mmol/l Cell (ICF) 65 mmol/l (including organic P) PHOSPHATES (2) calcium phosphate, hydroxyapatite (bone) inorganic anions: HPO32-, H2PO3organic:DNA, phospholipids ATP, cAMP, creatinphosphate molecules with metabolic significance Ca, P rates of intake 1g/day Bones – reservoir of calcium 99% of skeletal calcium forms stable bone (not exchangeable with the Ca in extracellular fluid) 1% is in the form of releasable pool of Ca Balance of deposition and resorption Osteoblasts – bone-forming cells responsible for bone deposition Secrete type I collagen Differentiate into osteosytes Osteoclasts – “bone-eating” cells that resorb the previously formed bone Regulation of osteoblasts function Stimulation PTH (fast reaction - activation of calcium pump ? – pumping Ca to ECF) 1,25 Dihydrocholecalciferol IL-1 T3, T4 hGH, IGF-1 (insuline-like growth factor) PGE2 (prostaglandine) TNF (tumor necrosis factor) Estrogens ? Inhibition Corticosteroids Regulation of osteoclasts function Stimulation PTH (not directly – through stimulation of osteoblasts) 1,25 Dihydrocholecalciferol (not directly – through stimulation of osteoblasts) IL-6, IL-11 Inhibition Calcitonin (directly – receptors) Estrogens (by inhibiting production of certain cytokines) TGF-β (tranforming growth factor) PGE2(prostaglandine) Bone structure Due to Copyright rules it is impossible to publish pictures that were used in this lecture. Therefore, all slides that contained pictures are blank. Thank you for understanding. From Ganong Sex differences From Ganong Thyroid and Parathyroid glands Calcium metabolism From Guyton and Hall Regulation of calcium metabolism 1. 2. 3. Parathyroid hormone Calcitonin Vitamin D PARATHORMON Parathyroid glands polypeptide of 84 amino acids stimulus for secretion – low plasma calcium function – to INCREASE plasma calcium activation of osteoclasts – stimulates absorption of Ca, P from bones decreases excretion of Ca by kidneys increases excretion of P by kidneys stimulates conversion of vitamin D to calcitriol (vitamin D hormon) in kidneys Relation - plasma Ca2+ concentration x hormones CALCITONIN Parafollicular cells of thyroid gland (C-cells) peptide of 32 amino acids stimulus for secretion – high plasma calcium (food intake – gastrin, CCK, glucagon) function – to DECREASE plasma calcium and phosphates inhibits osteolysis – decreases absorption of Ca, P from bones stimulates incorporation of Ca, P to bones decreases absorption of Ca, P in kidneys decreases the effect of PTH on bones – PTH antagonist CALCITRIOL vitamin D hormone Skin: preprovitamin D (7-dehydrocholesterol ergosterol) - UV irradiation: cholecalciferol (D3), ergocalciferol (D2) - Liver:25hydroxycholecalciferol - Kidneys:1,25dihydroxycholecalciferol (conversion is mediated by PTH) function – to INCREASE plasma calcium increases absorption of Ca in intestines stimulates formation of calcium-binding protein in epithelial cells promotes bone calcification and deposition inhibits secretion of PTH CALCITRIOL vitamin D hormone (2) Changes in Ca2+ plasma level Hypocalcemia Muscle tetany carpopedal spasm Dilatation of heart Increased cell membrane permeability Impaired blood clotting Hypercalcemia Depression of nervous system, reflex activity, Increased heart contractility Formation of calcium phosphate crystalls Carpopedal spasm From Guyton and Hall Changes in PTH plasma level Hypoparathyroidism Muscle tetany Hyperparathyroidism Decalification of bones Multiple fractures (Osteitis fibrosa cystica) Kidney stones Changes in vitamine D plasma level Hypovitaminosis RICKETS (rachitis)– children OSTEOMALACIA - adults Attention! – Osteoporosis is decrease of bone mass (matrix and minerals) Hypervitaminosis Tissue and organs calcification Lost of body weight Kidney function failure Basic functions of plasma membrane 1. 2. 3. 4. Transport Membrane potential Ion channels Mechanism of secretion Structure of the plasma membrane Ionic composition of ICF and ECF Ion ECF ICF mmol/l mmol/l equilibrium potential Na+ 136-146 20 +53 mV K+ 3.8-5.4 150 -97 mV 2.05-2.65 c. 10-4 +120mV 97-109 3 -97 mV 22-26 10 -30 mV Ca2+ ClHCO3- Nernst



























![Poster ECE`14 PsedohipoPTH [Modo de compatibilidad]](http://s1.studyres.com/store/data/007957322_1-13955f29e92676d795b568b8e6827da6-150x150.png)
![sodium metabolism and hypertension 2[Autosaved]](http://s1.studyres.com/store/data/001592752_1-daeec6c754fcef654257413902c3eb98-150x150.png)