* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download infectious disease conference
Middle East respiratory syndrome wikipedia , lookup
Sarcocystis wikipedia , lookup
Oesophagostomum wikipedia , lookup
Leptospirosis wikipedia , lookup
Foodborne illness wikipedia , lookup
Antibiotics wikipedia , lookup
Typhoid fever wikipedia , lookup
Cryptosporidiosis wikipedia , lookup
Schistosomiasis wikipedia , lookup
Pathogenic Escherichia coli wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
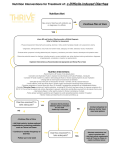
INFECTIOUS DISEASE CONFERENCE MENDOZA, DONNE MENDOZA, GRACIELLE MENDOZA, TRISHA MINDANAO, MALVIN ACE O.P. 7 months, male August 20, 2010 157-2 M. Dela Fuente St. Sampaloc, Manila Roman Catholic Informant: Parents Reliability: Good DIARRHEA HISTORY OF PRESENT ILLNESS 1 hr PTA 30 min PTA ADMISSION 3 episodes of vomiting •amounting to 15mL/episode - 4 episodes of loose, mucoid, yellowish stool, altogether amounting to 200mL - Noted to be weak-looking, w/ cold clammy skin REVIEW OF SYSTEMS Cutaneous: (-) rashes, (-) pruritus HEENT: (-) nasoaural discharge, (-) eye discharge, (-) sore throat Respiratory: (-) dyspnea, (-) chest pain Cardiovascular: (-) palpitations, (-) cyanosis, (-) easy fatigability Gastrointestinal: SEE HPI REVIEW OF SYSTEMS Genitourinary: (-) dysuria (-) hematuria Musculoskeletal: (-) weakness, (-)swelling Hematopoietic: (-) easy bruisability, (-) bleeding Endocrine: (-) polyuria, polydipsia, polyphagia Nervous/Behavior: (-) headache, (-) seizures, (-)tremors, (-) loss of consciousness GESTATIONAL HISTORY Born to a 22 y/o G1P0 mother with a common law 27 y/o policeman partner Regular prenatal check-up since 5 mo AOG Hep B screening and OGCT were not done No history of alcohol intake, smoking or exposure to radiation No illnesses noted during pregnancy NEONATAL HISTORY Born at 39-40 weeks AOG Live, singleton, delivered via NSD APGAR score 8-9 Birth weight = 2.7 kg Birth length – unrecalled 1-day stay at the nursery No complications noted during delivery FEEDING HISTORY Breastfed exclusively for 1 month More than 8 times per day or everytime child cries Shifted to milk formula Mother claimed she was not producing enough milk Bottlefed since 2 months until present 2-5 months: S26 – 1:2 dilution, 4 oz per feeding, 6x /day 6 months to present: Bonamil – 1:2 dilution, 8 oz per feeding, 4-5x/day Complementary feeding started at 6 months Cerelac and pureed food 24 – HR FOOD RECALL Macronutrients Amount BREAKFAST Milk 1:2 8 oz Total CHO (4 cal/g) CHON (4 cal/g) Fats (9 cal/g) Kilocalories 12 8 10 170 12 12 8 3 10 2,5 170 83 12 8 10 170 12 8 10 170 763 SNACK LUNCH Milk Cerelac SNACK Milk DINNER Milk ACI RENI % 720 106% DEVELOPMENT/BEHAVIORAL HISOTRY Gross motor With good head control, can crawl, rolls over, sits with support Fine motor Transfers object from 1 hand to another Language Imitates speech sounds Personal Social Laughs and plays with examiner IMMUNIZATIONS HEALTH CENTER BCG – 1 dose Hep B – 1 dose DPT – 3 doses OPV – 3 doses Hib – 1 dose PAST MEDICAL HISTORY October 2010 – Pneumonia January 2011 - Diarrhea FAMILY HISTORY (+) HPN – maternal grandmother (-) DM, goiter, asthma, cancer, TB FAMILY PROFILE Age Educational Attainment Occupation Health Mother 22 High school graduate none Healthy Father 27 College graduate Policeman Healthy Relation PERSONAL, SOCIOECONIMIC AND ENVIRONMENTAL HISTORY Apartment with both parents Well-ventilated, well-lit Drinking water is purified Garbage is not segregated but collected everyday No nearby factories, no pets PHYSICAL EXAMINATION Alert, awake, weak-looking, with moderate signs of dehydration, drinks eagerly, not in cardiorespiratory distress VS: CR 160 RR 40 T 36.9 Wt 6 kg. (z= 0) Lt. 73 cm (z= 0) AC: 43 cm BMI 11 (z= below -3) wt. for Ht. (z= below -3) PHYSICAL EXAMINATION Warm, dry skin, no active dermatoses Pink palpebral conjunctiva, anicteric sclerae, (+) sunken eyeballs No tragal tenderness, non-hyperemic EAC, (+) retained cerumen, AU, intact tympanic membrane, no aural discharge AU Midline septum, turbinates not congested, no nasal discharge PHYSICAL EXAMINATION Dry buccal mucosa, no oral lesions, to non- hyperemic posterior pharyngeal wall, tonsils not enlarged Supple neck, no palpable cervical lymphadenopathies or anterior neck masses Symmetrical chest expansion, no retractions, clear breath sounds Adynamic precordium, apex beat 4th LICS MCL, no heaves, thrills, murmurs PHYSICAL EXAMINATION Globular abdomen, NABS, soft, non- tender, no mass palpated Pulses full and equal, no cyanosis, no edema No genital lesions, no phimosis DRE: tight sphincteric tone, no tenderness, no masses, brown fecal material on tactating finger, non-blood tinged NEUROLOGIC EXAMINATION Mental Status: alert, awake Cranial Nerves are intact: intact EOM; no ptosis; no jaw deviation; smiles, open and close his eyes, no facial asymmetry; midline uvula, no tongue atrophy, no fasciculations, no deviation No Babinski, no nuchal rigidity SALIENT FEATURES POSITIVE 7 mo/male Diarrhea – mucoid stools Vomiting Weak-looking, with cold clammy skin Past medical history of diarrhea (+) sunken eyeballs dry buccal mucosa drinks eagerly NEGATIVE (-) fever (-) abdominal pain ADMITTING IMPRESSION DIARRHEA APPROACH TO DIAGNOSIS Look for a symptom, sign, or laboratory finding pointing to a group of diseases COURSE IN THE WARDS DAY 1 CBC with platelet count and fecalysis were done. CBC showed normal results, while fecalysis showed pus cells of over 100/hpf, RBC of (+), and macrophage of (+), and stool culture was then requested. ORS 75 to replace losses volume per volume Zinc sulfate 10mg/ml, 2ml once a day for 14 days IVF started at D5 0.3% NaCl 100%. DAY 2 & DAY 3 Ciprofloxacin 16.6 mg/kg/day given for 3 days. IVF given was D5 0.3 NaCl at 100%. DAY 4 & DAY 5 Discharged improved and stable Diarrhea: definition Increased total daily stool output, usually associated with increased stool water content Stool output more than 10g/kg/24hr or more than the adult limit of 200 g/24hr Results from altered intestinal water and electrolyte transport GIT of infant handles approx 285 ml/kg/24hr of fluid (intake plus intestinal secretion) with a stool output of 5-10g/kg/24hr Diarrhea: chronicity Acute Chronic/Persistent Less than 2 weeks More than two weeks Diarrhea: pathophysiology Osmotic Secretory Increased/decreased intestinal motility Decreased surface area Diarrhea: pathophysiology PRIMARY MECHANISM DEFECT STOOL EXAMINATION Secretory Decreased absorption, increased secretion, electrolyte transport Watery, normal osmolality; osmoles = 2 × (Na+ + K+) Osmotic Maldigestion, transport defects ingestion of unabsorbable Watery, acidic, and reducing substances; increased osmolality; osmoles >2 × (Na+ + K+) EXAMPLES COMMENT Cholera, Persists during toxigenic E. coli; fasting; bile salt carcinoid, VIP, malabsorption neuroblastoma, may also increase congenital intestinal water chloride secretion; no diarrhea, stool leukocytes Clostridium difficile, cryptosporidiosis (AIDS) Lactase Stops with deficiency, fasting; increased glucose-galactose breath hydrogen malabsorption, with lactulose, carbohydrate laxative abuse malabsorption; no stool leukocytes PRIMARY MECHANISM DEFECT STOOL EXAMINATION Increased motility Decreased transit Loose to normaltime appearing stool, stimulated by gastrocolic reflex Decreased motility Defect in neuromuscular unit(s) Stasis (bacterial overgrowth) Decreased functional capacity EXAMPLES COMMENT Irritable bowel Infection may syndrome, also contribute to thyrotoxicosis, increased postvagotomy motility dumping syndrome Loose to normal Pseudoobstructio Possible bacterial appearing stool n, blind loop overgrowth Decreased Watery surface area (osmotic, motility) Mucosal invasion Inflammation, Blood and decreased colonic increased WBCs reabsorption, in stool increased motility Short bowel May require syndrome, celiac elemental diet disease, rotavirus plus parenteral enteritis alimentation Salmonella, Dysentery Shigella, evident in blood, infection; mucus, and amebiasis; WBCs Yersinia, Campylobacter infections Diarrhea: pathophysiology Volume of stool OSMOTIC DIARRHEA <200 mL/24 hr SECRETORY DIARRHEA >200 mL/24 hr Response to fasting Diarrhea stops Diarrhea continues Stool Na+ <70 mEq/L >70 mEq/L Reducing substances[*] Positive Negative Stool pH <5 >6 fasting stops persists example Lactose intolerance Cholera, ETEC Acute diarrhea Infectious Bacteria B. cereus C. jejuni C. perfringens E. Coli (STEC, EIEC) Salmonella spp Shigella spp S. aureus V. cholerae V. parahaemolyticus V. vulnificus Virus Norovirus Calicivirus Rotavirus Astrovirus Adenovirus Parvovirus Protozoa G. Lamblia Non-infectious Protein intolerance Intussusception Meckel’s diverticulum Food hypersensitivity Food-induced enterocolitis Ciguater fish poisoning Mushroom poisoning Nitrite poisoning Organophosphates Puffer fish (tetrodotoxin) Scombroid (histamine) Shellfish poisoning Heavy metals Sb, As, Cd, Cu, Hg, Zn, Th Acute infectious diarrhea Inflammatory Usually bacteria that directly invades the intestines or produce cytotoxins with consequent fluid, protein and cells that enter the intestinal lumen Presents as bloody mucoid stool Fecalysis: + fecal leukocytes Non-inflammatory Enterotoxin production by some bacteria (cholera), destruction of villous cells by viruses (rotavirus), adherence by parasites (G lamblia), and adherence and or translocation by bacteria Acute infectious inflammatory diarrhea Shigella Salmonella E coli: EPEC, EIEC, EAEC, ETEC, STEC C jejuni INCUBATIO ETIOLOGY N PERIOD Campylobacter 2–5 days jejuni SIGNS AND SYMPTOMS Diarrhea, cramps, fever, and vomiting; diarrhea may be bloody. DURATION ASSOCIATED LABORATOR OF ILLNESS FOODS Y TESTING 2–10 days Raw and Routine stool undercooked culture; poultry, Campylobacter unpasturized requires special milk, media and contaminated incubation at water 42°C to grow. Enterotoxigenic 1–3 days E. coli (ETEC) Watery diarrhea, abdominal cramps, some vomiting 3 to >7 days Water or food contaminated with human feces Stool culture. ETEC requires special laboratory techniques for identification. If suspected, must request specific testing. TREATMENT Supportive care. For severe cases, antibiotics such as erythromycin and quinolones may be indicated early in the diarrheal disease. Guillain-Barré syndrome can be a sequela. Supportive care. Antibiotics are rarely needed except in severe cases. Recommended antibiotics include TMPSMX and quinolones. INCUBATIO SIGNS AND ETIOLOGY N PERIOD SYMPTOMS Enterohemor 1–8 days rhagic E. coli (EHEC) including E. coli O157 : H7 and other Shiga toxin– producing E. coli (STEC) DURATION ASSOCIATED LABORATOR OF ILLNESS FOODS Y TESTING TREATMENT Severe 5–10 days diarrhea that is often bloody, abdominal pain and vomiting. Usually, little or no fever is present. More common in children <4 yr old. Undercooked beef especially hamburger, unpasteurized milk and juice, raw fruits and vegetables (e.g., sprouts), salami (rarely), and contaminated water Stool culture; Supportive E. coli O157 : care, monitor H7 requires renal function, special media hemoglobin, to grow. If E. and platelets coli O157 : H7 closely. E. coli is suspected, O157 : H7 specific testing infection is must be also associated requested. with hemolytic Shiga toxin uremic testing may be syndrome done using (HUS), which commercial can cause kits; positive lifelong isolates should complications. be forwarded Studies to public indicate that health antibiotics laboratories may promote for the confirmation development and of HUS. serotyping. INCUBATIO N PERIOD ETIOLOGY Salmonella spp. 1–3 days Shigella spp. 24–48 hr SIGNS AND SYMPTOMS DURATION ASSOCIATED LABORATOR OF ILLNESS FOODS Y TESTING TREATMENT Diarrhea, fever, 4–7 days abdominal cramps, vomiting. S. typhi and S. paratyphi produce typhoid with insidious onset characterized by fever, headache, constipation, malaise, chills, and myalgia; diarrhea is uncommon, and vomiting is not usually severe. Contaminated Routine stool eggs, poultry, cultures unpasteurized milk or juice, cheese, contaminated raw fruits and vegetables (alfalfa sprouts, melons). S. typhi epidemics are often related to fecal contamination of water supplies or street-vended foods. Abdominal 4–7 days cramps, fever, and diarrhea. Stools may contain blood and mucus. Food or water Routine stool contaminated with cultures human fecal material. Usually person-to-person spread, fecal-oral transmission. Ready-to-eat foods touched by infected food workers, e.g., raw vegetables, salads, sandwiches. Supportive care. Other than for S. typhi and S. paratyphi, antibiotics are not indicated unless there is extraintestinal spread, or the risk of extra-intestinal spread, of the infection. Consider ampicillin, gentamicin, TMPSMX, or quinolones if indicated. A vaccine exists for S. typhi. Supportive care. TMP-SMX recommended in the U. S. if organism is susceptible; nalidixic acid or other quinolones may be indicated if organism is resistant, especially in developing countries. Escherichia coli Pathotype Epidemiology Type of diarrhea Mechanism of pathogenesis STEC Hemorhagic colitis and HUS in all ages and postdiarrheal thrombotic thrombocytopenic purpura in adults Bloody or non-bloody Large bowel adherence and effacement (AE), shiga toxin production EPEC Acute and chronic endemic and epidemic in infants Watery Small bowel AE ETEC Infantile diarrhea in resource-limited countries and traveler’s diarrhea in all ages Watery Small bowel AE, heat stable/ heat labile enterotoxin production EIEC Diarrhea with fever in all ages Bloody or non-bloody; dysentery Adherence, mucosal invasion and inflammation of large bowel EAEC Acute and chronic diarrhea in all ages Watery, occasionally bloody Small and large bowel adherence, enterotoxin and cytotoxin production DEHYDRATION MINIMAL OR NO DEHYDRATION (<3% LOSS OF BODY WEIGHT) MILD TO MODERATE DEHYDRATION (3–9% LOSS OF BODY WEIGHT) SEVERE DEHYDRATION (>9% LOSS OF BODY WEIGHT) Mental status Well;alert Normal, fatigued or restless, irritable Apathetic, lethargic, unconscious Thirst Drinks normally; might refuse liquids Thirsty;eager to drink Drinks poorly; unable to drink Heart rate Normal Normal to increased Tachycardia, with bradycardia in most severe cases Quality of pulses Normal Normal to decreased Weak, thready, or impalpable Breathing Normal Normal;fast Deep Eyes Normal Slightly sunken Deeply sunken Tears Present Decreased Absent Mouth and tongue Moist Dry Parched Skinfold Instant recoil Recoil in <2 sec Recoil in >2 sec Capillary refill Normal Prolonged Prolonged;minimal Extremities Warm Cool Cold;mottled;cyanotic Urine output Normal to decreased Decreased Minimal SYMPTOM CLINICAL IMPRESSION ACUTE INFECTIOUS DIARRHEA WITH MODERATE SIGNS OF DEHYDRATION CONFIRMATION OF WORKING DIAGNOSIS STOOL EXAMINATION Examine for mucus, blood and leukocytes Fecal leukocytes are indicative of bacterial invasion of colonic mucosa Examine for parasites causing diarrhea such Giardia lamblia and E. histolytica Shouldd be obtained as early in the course of disease as possible from children with bloody diarrhea STOOL CULTURE Should be obtained as early in the course of disease as possible from children with bloody diarrhea in whom stool microscopy indicates fecal leukocytes TREATMENT Principles of Management 1. 2. 3. 4. Oral Rehydration Therapy Enteral feeding and diet selection Zinc supplementation Antibiotic therapy Oral Rehydration Therapy Children especially infants are more susceptible than adults to dehydration because of the greater basal fluid and electrolyte requirements. Dehydration must be evaluated rapidly and corrected 4-6hrs according to the degree of dehydration. Oral Rehydration Therapy Those in shock or unable to tolerate fluids, require initial intravenous rehydration but oral rehydration is the preferred mode of replacing ongoing losses. Risks associated with severe dehydration that necessitate IV resuscitation Age <6mos Prematurity Chronic illness Fever >38C if <3mos or 39C if 3-36mos Bloody diarrhea Persistent emesis Poor urine output Sunken eyes Depressed level of consciousness Oral Rehydration Therapy Decarbonated soda beverages, fruit juices are not suitable for rehydration as they have inappropriately high osmolalities and low sodium concentrations ORS should be given to infants and children slowly, especially if they have emesis It can be given by a dropper, teaspoon or syringe. The volume is increased as tolerated. Enteral Feeding and Diet Selection Continued enteral feeding in diarrhea aids in recovery and age appropriate diet after rehydration is the norm. Once rehydration is complete, food should be reintroduced while oral rehydration can be continued to replace ongoing losses from emesis or stools. Enteral feeding and Diet Selection Breast feeding should be resumed as soon as possible Foods with complex carbohydrates, yogurt, fruits and vegetables are also tolerated Fatty foods or foods high in simple sugars should be avoided. Zinc supplementation Zinc leads to reduced duration and sseverity of diarrhea and could potentially prevent 300,000 deaths. WHO and UNICEF recommend that all children with acute diarrhea should recive oral zinc for 10-14 days during and after diarrhea 10mg/day for infants <6mos 20mg/day >6mos Antibiotic Therapy Timely antibiotic therapy may reduce the duration and severity of diarrhea and prevent complications. While these agents are important to use in specific cases, their widespread and indiscriminate use leads to development of resistance. ORGANISM DRUG OF CHOICE DOSE AND DURATION OF TREATMENT Shigella (severe dysentery and EIEC dysentery) Ciprofloxacin, ampicillin, ceftriaxone, or trimthoprimsulfamethoxazole Ceftriaxone IV, IM 50–100 mg/kg/d qd, bid × 7 d Most strains are resistant to Ciprofloxacin PO 20–30 many antibiotics mg/kg/d bid × 7–10 d 10 mg/kg/d of TMP and 50 mg/kg/d of SMX bid × 5 d Ampicillin PO, IV 50–100 mg/kg/d qid × 7 d EPEC, ETEC, EIEC TMP-SMX or ciprofloxacin 10 mg/kg/d of TMP and 50 mg/kg/d of SMX bid × 5 d Ciprofloxacin PO 20–30 mg/kg/d qid for 5–10 d Salmonella No antibiotics for uncomplicated GASTROENTERITIS Communityacquired Viruses, E. coli Antibiotic therapy strongly discouraged because of increased risk of HUS occurring in patients with E. coli 0157:H7 treated with antibiotics Primary treatment: fluid and electrolyte replacement Salmonella Cefotaxime or Ceftriaxone 10-14 days for infants <6 mo, toxicity or immunocompromised status. Antibiotics generally not indicated otherwise. Shigella TMP/SMX; Alt: Cefixime 5 days GASTROENTERITIS Community acquired Yersinia TMP/SMX, aminoglycosides, cefotaxime, tetracycline (>8 yr). Nosocomial Clostridium difficile Metronidazole Usually no antibiotic therapy is recommended except with bacteremia, extraintestinal infections, or immunocompromis ed hosts. 7 days. Community organisms unlikely after 72 hr of hospitalization. EVALUATION OF YOGHURT EFFECT ON ACUTE DIARRHEA ON 6-24 MONTHS-OLD HOSPITALIZED INFANTS N. PASHAPOUR, S. GOLMAHAMMADLOO PEDIATRICS DEPARTMENT, IMAM HOSPITAL HEALTH DEPARTMENT, KOSAR HOSPITAL, URMIA, IRAN THE TURKISH JOURNAL OF PEDIATRICS 2006; 48: 115-118 OBJECTIVES To determine the efficacy of local factory pasteurized yoghurt consumption in acute nonbloody and mucoid diarrhea on hospitalized 6-24 months infants as compared with that of routine treatment SUBJECTS 6 to 24 months of age children with non-bloody and mucoid diarrhea with less than four days duration hospitalizing in Urmia; Imam Hospital 2 GROUPS (20 EACH) Control group: routine hospital treatment only Case group: received at least 15 ml/kg/day of pasteurized cow milk yogurt orally plus routine hospital treatment Weight gain, period of hospitalization and reduction of diarrhea were compared EXCLUSION Malnutrition Bloody stools Non-alimentary causes RESULTS Mean hospitalization days : 2.85 – 3.1 Mean weight gain : 350 – 287.5 Mean reduction of diarrhea episodes : 4.35 – 3.95 Significant difference (P<0.50) reduction of diarrhea episodes CONCLUSION Use of local pasteurized yoghurt in the treatment of acute diarrhea had positive effects As a probiotic, it can promote recovery from diarrhea in children, mainly non-bloody Universal use of yoghurt is recommended in acute non-bloody diarrhea