* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Clostridium difficile
Sarcocystis wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Antibiotics wikipedia , lookup
Onchocerciasis wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Marburg virus disease wikipedia , lookup
Leptospirosis wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Schistosomiasis wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Gastroenteritis wikipedia , lookup
Fasciolosis wikipedia , lookup
Oesophagostomum wikipedia , lookup
Multiple sclerosis wikipedia , lookup
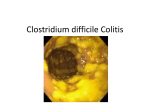
C’est difficile…? Martin Kiernan Nurse Consultant Southport and Ormskirk NHS Trust Vice President, Infection Prevention Society Clostridium difficile 1935 first described by as bacillus difficilis by Hall and O’Toole and classified as a commensal 1977 toxin isolated from stool samples produced a cytopathic effect in cell culture 1978 C. difficile identified as source for toxin and cause of psuedomembranous colitis Microbiology Gram positive, spore forming rod shaped bacillus Obligate anaerobe Produces 2 major toxins toxin A and toxin B both contribute to disease Toxins responsible for manifestation of disease and marker for diagnosis Annual Cases (England) So why are we where we are? The authors of the latest 2009 guidelines considered that ‘it is the failure to implement the guidance described in the 1994 report that has contributed to the recent rise’ Noted by the HPA and the HCC in 2006 Financial Burden of C. difficile Wilcox, Cunniffe et al, JHI; 1996 Cases stay an average of 21.3 days longer Extra costs Treatment, Investigations, ‘Hotel costs’ Total identifiable costs over £4,000 per case 2006 costs My Trust - £400K NW SHA - 6,946 cases - £28 million NHS - 55,681 cases - £222 million NHS lost nearly 1.2 million bed days Risk factors for disease Chang and Nelson (2000) Age > 65 years Antibiotic therapy, particularly cephalosporins, clindamycin Underlying bowel disease Proton pump inhibitors PEG feeds Physical proximity to symptomatic patient C.difficile, ABx, PPIs CDAD Antibiotic x1000 PPI x 1000 60000 50000 40000 30000 20000 10000 0 1997 1998 1999 2000 2001 2002 2003 2004 2005 2006 Case control study of Community CdI Wilcox, Mooney et al (2008) Exposure to Abx in previous 4 weeks esp. multiple agents Half had no abx in the previous month Hospitalisation in previous 6 months A third had neither hospitalisation not ABx Contact with infants >2 years old PPI not significantly more common C. difficile strains 160 ribotypes of C. difficile Type 001 most common in UK hospitals, Community epidemiology differs Type 010 most common All sensitive to metronidazole and vancomycin so far Epidemiology of C. difficile is changing Type 106 C. difficile 027 Hyper-toxin producer 18 base pair deletion ? Red herring 16-20 times more toxin produced Toxin produced earlier in the disease process Overwhelming of immune response Presence of binary toxin ? Red herring Diagnosis of C.difficile Clinical diagnosis sigmoidoscopy radiology Toxin isolation cytotoxin assay 92% sensitivity & specificity expensive and lengthy incubation required culture less efficient rapid immunoassay (less expensive, quick) Smell… Clinical manifestations of C.difficile Asymptomatic carriage 2% healthy adults 16-35% recently treated with antibiotics important reservoir in medical facilities shed organisms, contaminate environment carriage not reduced by treatment with metronidazole or vancomycin Clinical manifestations of C.difficile Antibiotic colitis presents as diarrhoea, lower abdominal pain starts during or shortly after antibiotics commence (a few days) but may present much later (1-2 months) systemic symptoms often absent examination often normal including sigmiodoscopy toxins in stool Clinical manifestations of C.difficile Psuedomembranous colitis symptoms more marked, bloody stools characteristic yellow plaques 2-10mm intervening mucosa mild inflammation plaques may conjoin rectum and sigmoid most common may progress to fulminant colitis Fulminating Disease Five Alerts Abdominal distension and tenderness High (very high) WCC ( can be 40-50 x109/l) Raised CRP/ drop in Hb Non response To oral metronidazole/vancomycin Low albumin all these features could denote the presence of Toxic Mega Colon - IMMEDIATE senior review, abdominal Xray and surgical referral Management of C.difficile Treatment resuscitation stop causative antibiotic (if possible) antibiotics restore normal gut flora Surgery Mortality from surgery 25-100% Low Serum Albumin a good predictor of certain death (<25g/L) or a fall by 11g/L at the onset of infection Saccharomyces boulardii Produces a protease that inhibits effect of toxins A and B in human colonic mucosa colonisation by 72 hours 107-108 cfu cleared when therapy discontinued not absorbed Expensive Different preparations have differing activity Other options? Brewers yeast Saccharomyces cerevisae less expensive than S.boulardii but distinct and not equivalent Faeces from related donors Given as enema or via Nasogastric Tube Not very acceptable to staff or patients Immunoglobulin Transmission Faecal-oral route Environment becomes contaminated by spores Hands become contaminated by spores Vulnerable patients acquire spores after contact with contaminated staff and the environment And then they eat them.. What is Critical? Prevent environmental contamination Consider faecal containment if liquid stool Rapid isolation of the patient Simple things Pulling back the sheets Commode cleaning Side room with toilet No exposed food Careful with that bedding C.difficile spores Environment floors toilets bedpans bedding mops scales Health Care professionals hands rings stethoscopes faecal carriage rare Am J Epidemiology 1988 127:1289-94 Am J Med 1981;70:906 Just how important IS the environment? Samore et al presence on hands correlates with density of environmental contamination (AmJ Med 1996) 0-25%sites + 0% hands + 26-50% + 8% hands + >50% + 36% hands + Fawley (Epid Infect 2001) incidence correlates significantly with level of environmental contamination Isolation Wards They work They also free up isolation capacity elsewhere in the organisation They ensure consistency of care for all patients, whose primary diagnosis should now be considered to be the infection They are not permanent They do allow you to get the situation back under control and draw breath Cross-infection risks Is it only the symptomatic patient? One paper recently published in Clinical Infectious Diseases in October 06 says not 56% of skin tests were positive for C. difficile in the asymptomatic patient Spores present on the skin can be effectively transmitted to HCW hands and the environment Hands must be washed with soap and water after dealing with faecal matter for every patient Efficacy of Alcohol Hand Sanitizers Provide an overall 3-4 log10 (99.9-99.99%) reduction in most bacterial and viral pathogens with a contact time of 15 seconds NOT C. difficile spores NOT Norovirus Norovirus are reduced by only 1-2 log10 (90-99%) with a 30 second contact time C. difficile in the over-65s Quarterly Cases - England, 2006-8 C’est tres difficile Increasing elderly population Average age of inpatients up 1.5 years each year Acute beds falling in numbers Creates a filtered inpatient population Expectation to treat Have sympathy for the poor house officer The ‘old man’s friend’ is now his greatest enemy