* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
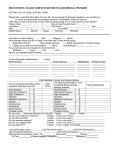
Download CPC # 2 October 12, 2004
Survey
Document related concepts
Transcript
CPC # 2 Infectious Disease October 7, 2008 Lisa L. Maragakis, MD MPH Important Features of the Case • 58 yo man with a history of alcoholism, smoking, hypertension and chronic pain • Presents with 5 days of cough and fever with progressive dyspnea and “weakness” • Confusion and slurred speech is also reported by the patient’s wife • Other symtoms include: – headache – Pleuritic chest pain (R) – Urinary incontinence (new) Important Features of the Case • No recent medical care and not taking antihypertensive meds • Upon admission: – BP=133/94, P=125, RR=24, afebrile; – Moderate respiratory distress; 95% on 6L NC; wheezing and rhonchi – Alert, not oriented to date, slurred speech • WBC=1.1, Hct (50%), ↓Plt (55k), ALT (141), Tbili (2.1) ↓TP/alb, PT/PTT, lactate (12.6), BUN (48), Cr (4.0), ammonia=33 • Imaging shows multi-lobar dense consolidation and cavitation of RUL, lymphadenopathy • Head CT essentially negative Summary of the Case • Alcoholic man presents with an acute illness characterized by multi-lobar pneumonia, hepatic encephalopathy, lactic acidosis, coagulopathy and renal failure • Rapidly developed hypotension, respiratory failure, and expired within 36 hours Possible Etiologies of the Elevated Ammonia level • • • • • • • Hepatic encephalopathy Shock ETOH Renal disease GI bleeding Salicylate intoxication Ethylene glycol Possible Etiologies of the Elevated Lactate level • Severe hypoxemia • Shock • Decrease in lactate utilization due to ETOH and liver disease Community-Acquired Pneumonia, Sepsis and Multi-organ Failure • Approximately 10% of CA pneumonia requires ICU care and mechanical ventilation • Risk factors – – – – Advanced age Comorbid disease DM ETOH Community-Acquired Pneumonia, Sepsis and Multi-organ Failure – Severe CAP defined by • RR>30, PaO2/FIO2<250, need for mechanical ventilation, multi-lobar pneumonia, increased size of infiltrate up to 50% in 48 hrs, BP<90/60, pressor requirement, acute renal failure – Mortality rates 20-53% (as opposed to 2-30% for “regular” CAP) Community-Acquired Pneumonia, Sepsis and Multi-organ Failure – S. pneumoniae and L. pneumophila are the most common etiologies – Gram negative bacilli, especially Klebsiella, occur in patients with DM, COPD, and ETOH abuse (this patient) Community-Acquired Pneumonia, Sepsis and Multi-organ Failure – Initial presentation of CAP in older adults can present as • • • • • Decline in functional status Weakness Mental status changes Anorexia Abdominal pain Differential Diagnosis of Community Acquired Pneumonia • S. pneumoniae accounts for 20-60% of cases • H. influenzae causes 7-11% • Older and debilitated patients more likely to have GNB colonizing oropharynx • Group A and B streptococci • M. cattarhalis • Legionella • Atypicals: M. pneumoniae, Clamydyia • Viral pneumonia: RSV, influenza, parainfluenza • Aspiration pneumonia Differential Diagnosis of Community Acquired Pneumonia • Aspiration – Silent vs witnessed – ETOH is a risk factor – Chemical pneumonitis – Mixed flora + anaerobes – Upper lobe atypical but not impossible Differential Diagnosis of Community Acquired Pneumonia • Atypical pneumonia syndromes – M. pneumoniae – C. pneumoniae – Legionella – Francisella tularensis – M. TB – Coxiella burnetii – Pneumocystis Differential Diagnosis of Community Acquired Pneumonia • • • • S. aureus Not on the traditional lists of CAP etiology Seen increasingly as causing CAP Can cause necrotizing, cavitary pneumonia with rapidly progressive sepsis as seen in this case Diagnosis • Send sputum and blood cultures BEFORE antimicrobials are started • Legionella urinary antigen (only detects serogroup 1) • Consider NP aspirate during flu season • Consider anthrax if widened mediastinum • Bronchoscopy, open lung biopsy Therapy for CAP • Not in the ICU – Ceftriaxone PLUS Azithromycin or – Moxifloxacin • In the ICU – Same as above or – Cover for Pseudomonas if at risk • Cefipime PLUS Azithromycin • Moxifloxacin PLUS Aztreonam Risks for Pseudomonas • • • • • • Prolonged hospital or LTCF stay (>5d) Structural lung disease Steroid therapy Broad-spectrum ABX in past month AIDS Neutropenia Therapy for CAP • Aspiration – Clindamycin can be added to cover anaerobes • CA-MRSA – Linezolid can be added to cover empirically while awaiting culture data Therapy for CAP • If you have the luxury of tailoring therapy – Base ABX treatment choice on organism that grows from sputum and/or blood In this case… • Treated with moxifloxacin (appropriate) • If I had to bet, I would say this patient had CA-MRSA necrotizing pneumonia and sepsis with multi-organ failure