* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download MEDICAL GRANDROUNDS
Yellow fever wikipedia , lookup
Orthohantavirus wikipedia , lookup
Ebola virus disease wikipedia , lookup
Schistosomiasis wikipedia , lookup
Neonatal infection wikipedia , lookup
Rocky Mountain spotted fever wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
West Nile fever wikipedia , lookup
Henipavirus wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
Herpes simplex virus wikipedia , lookup
Leptospirosis wikipedia , lookup
Gastroenteritis wikipedia , lookup
Oesophagostomum wikipedia , lookup
Marburg virus disease wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Hepatitis C wikipedia , lookup
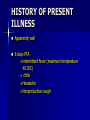
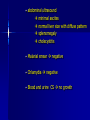
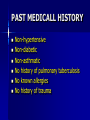
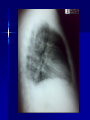
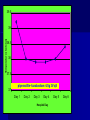
MEDICAL GRANDROUNDS IVY KATHRYN ILAGAN, MD August 21, 2008 OBJECTIVES To discuss an unusual presentation of infectious mononucleosis. GENERAL DATA RC 35 year old male Married Filipino CHIEF COMPLAINT FEVER HISTORY OF PRESENT ILLNESS Apparently well 8 days PTA intermittent fever (maximum temperature 40.30C) chills Headache Nonproductive cough 6 days PTA Consult done CBC normal systemic viral illness sent home 5 days PTA still has intermittent fever epigastric pain Vomiting Loose watery stool, 4x 4 days PTA Admitted in a private hospital Work-ups done: • CBC leukocytosis, predominance of lymphocytes • CXR bibasal pneumonia with minimal pleural effusion, left • abdominal ultrasound minimal ascites normal liver size with diffuse pattern splenomegaly cholecystitis • Malarial smear negative • Chlamydia negative • Blood and urine CS no growth Treated as pneumonia and acute gastroenteritis Fever, epigastric pain, vomiting, and diarrhea persisted, hence transferred in this institution REVIEW OF SYSTEMS General (-) weight loss Head and neck (-) blurring (-) visual changes (-) sorethroat Chest and Lungs (-) dyspnea Cardiovascular (-) (-) (-) (-) chest pain palpitations easy fatigability orthopnea Gastrointestinal (-) hematemesis (-) hematochezia (-) melena Genitourinary (-) dysuria (-) hematuria Hematologic (-) easy bruisability Neurologic (-) changes in behavior PAST MEDICALL HISTORY Non-hypertensive Non-diabetic Non-asthmatic No history of pulmonary tuberculosis No known allergies No history of trauma FAMILY HISTORY Hypertension - paternal side Diabetes mellitus – maternal side Asthma - maternal side No history of blood dyscrasia PERSONAL AND SOCIAL Unemployed 15-pack year history of smoking Occasional alcoholic beverage drinker PHYSICAL EXAMINATION GENERAL SURVEY Awake, conscious, coherent, not in respiratory distress. VITAL SIGNS BP 130/80mmHg HR 90bpm RR 20cpm T 39.2C SKIN/HEAD/EYES/EARS/NOSE/NECK/THROAT Good skin turgor Pink palpebral conjunctiva, icteric sclerae no tonsillopharyngeal congestion no cervical lymphadenopathy CHEST AND LUNGS Symmetrical chest expansion, no retractions Crepitant rales, bibasal area Decreased breath sounds, right lung base No wheezes CVS – Normal rate, regular rhythm, S1>S2 apex, S2>S1 base, no murmurs, no S3, no S4 ABDOMEN – Flabby – Normoactive bowel sounds – Soft – direct tenderness, epigastric area – palpable liver, up to 4 cm from subcostal line – dullness on 9th – 11th ICS (obliterated traube’s space) EXTREMITIES – No gross lesions – No hematoma, petechiae, purpura – No cyanosis – No edema – Full and equal peripheral pulses SALIENT FEATURES 35 year old male Previously treated in another hospital as pneumonia and acute gastroenteritis Abdominal ultrasound done revealed ascitis, cholecystitis, and splenomegaly On PE, – Febrile – Icteric – crepitant rales, bibasal area; decreased breath sounds, right lung base – palpable liver, up to 4 cm from subcostal line, dullness on 9th-11th ICS INITIAL IMPRESSION Community acquired pneumonia Hepatosplenomegaly, etiology to be determined Cholecystitis COURSE IN THE WARDS ABG at room air, RR24 pO2 81.1 pH 7.5 pCO2 31.6 HCO3 24.8 O2 sat 97% BE +2.6 TCO2 25.8 - respiratory alkalosis CXR – pneumonia, both lower lobes – minimal pleural effusion – mild left ventricular enlargement Pneumonia 5-Jun Alkaline Phosphatase 543 TB 1.7 DB – IB 1.3 – 0.4 Na 0.8 Lipase 224 Amylase 28 CT scan of the whole abdomen – Hepatosplenomegaly – Consider splenic infarctions – Minimal ascites – Prominent retroperitoneal lymph nodes, which may be reactive in nature – Minimal bilateral pleural effusion with compressive atelectasis in both lower lobes CT scan of the whole abdomen – Hepatosplenomegaly – Consider splenic infarctions Lipase 224 Amylase 28 Alpha fetoprotein negative Pneumonia Hepatosplenomegaly Acute Cholecystitis Pneumonia Hepatosplenomegaly Pneumonia Hepatosplenomegaly Splenic Infarct Pneumonia Hepatosplenomegaly Splenic Infarct Hematologic Infectious Autoimmune Malignancy Pneumonia Hepatosplenomegaly Splenic Infarct Hematologic Hepatosplenomegaly Splenic Infarct Infectious Autoimmune Hematologic Hepatosplenomegaly Splenic Infarct Infectious Autoimmune Infective Endocarditis Atrial Fibrillation Hematologic Leukemia Polycythemia Vera Hepatosplenomegaly Protein C&S Deficiency Infectious Salmonellosis Infectious Mononucleosis Splenic Infarct Autoimmune SLE Infective Endocarditis Atrial Fibrillation Hematologic Leukemia Polycythemia Vera Hepatosplenomegaly Protein C&S Deficiency Infectious Salmonellosis Infectious Mononucleosis Splenic Infarct Autoimmune SLE Infective Endocarditis Day 2 6-Jun Hgb Hct WBC Seg 11.7 36.9 8.96 26 Lympho 56 Mono Platelet ct 17 173T MCV MCH 83.9 26.6 Alkaline phosphatase TB DB – IB Na Day 1 Day 2 5-Jun 543 6-Jun 439 1.7 1.3 – 0.4 0.8 1.2 K BUN Creatinine CO2 Lipase Amylase 141 3.3 6 0.8 29 224 28 Day 1 Day 2 5-Jun 6-Jun SGOT 115 SGPT 129 Albumin 2.4 Corrected Ca 9.26 Glucose 89.91 Cholesterol 119.09 Day 1 Day 2 5-Jun 543 6-Jun 439 Alkaline phosphatase TB 1.7 DB – IB 1.2 1.3 – 0.4 SGOT 115 SGPT 129 Hepatocellular/ Cholestatic Viral Hepatitis Infectious Mononucleosis Pneumonia Hepatosplenomegaly Splenic Infarct Hepatocellular/ Cholestatic Viral Hepatitis Infectious Mononucleosis Alkaline phosphatase Day 1 Day 2 5-Jun 543 6-Jun 439 Heat fractionation of alkaline phosphatase 45% Heated alkaline phosphatase at 560C: 216 U/L <25% osteoblastic >25% hepatic Hgb Hct Day 2 Day 4 6-Jun 11.7 36.9 8-Jun 11.7 36.3 Hematologic Leukemia Polycythemia Vera Hepatosplenomegaly Protein C&S Deficiency Infectious Splenic Infarct Salmonellosis Infectious Mononucleosis Autoimmune SLE Hepatocellular/ Cholestatic Viral Hepatitis Infectious Mononucleosis Protein C normal 4.15 Protein S normal 17 Hematologic Leukemia Hepatosplenomegaly Protein C&S Deficiency Infectious Splenic Infarct Salmonellosis Infectious Mononucleosis Autoimmune SLE Hepatocellular/ Cholestatic Viral Hepatitis Infectious Mononucleosis p-ANCA negative Cryoglobulin negative Hematologic Leukemia Hepatosplenomegaly Infectious Splenic Infarct Salmonellosis Infectious Mononucleosis Autoimmune SLE Hepatocellular/ Cholestatic Viral Hepatitis Infectious Mononucleosis HbsAg negatve Anti HCV non reactive Hematologic Leukemia Hepatosplenomegaly Infectious Splenic Infarct Salmonellosis Infectious Mononucleosis Hepatocellular/ Cholestatic Infectious Mononucleosis Peripheral blood smear – WBCs with atypical forms, platelets appear increased and in clumps with some giant platelets noted. Bone marrrow culture – no growth Bone marrow biopsy - normal Hematologic Pneumonia Leukemia Hepatosplenomegaly Infectious Splenic Infarct Salmonellosis Infectious Mononucleosis Hepatocellular/ Cholestatic Infectious Mononucleosis Hepatosplenomegaly Infectious Splenic Infarct Salmonellosis Infectious Mononucleosis Hepatocellular/ Cholestatic Infectious Mononucleosis Hepatosplenomegaly Hematologic Infectious Autoimmune Splenic Infarct Infective Endocarditis Blood culture - Streptococcus viridans C reactive protein - positive up to 1:8 serum dilutions 2D Echocardiography with color flow and Doppler study - Normal, EF 70%. Mitral and tricuspid regurgitation are trivial. Transesophageal echocardiography – No echocardiographic evidence of endocardial vegetations on the aortic, pulmonic, mitral and tricuspid valves. – Intact interatrial septum. – No intracardiac thrombus formation. The diagnosis of infective endocarditis is established with certainty only when vegetations obtained at cardiac surgery, at autopsy, or from an artery (an embolus) are examined histologically and microbiologically. The Duke criteria—has been developed on the basis of clinical, laboratory, and echocardiographic findings. Documentation of two major criteria, of one major and three minor criteria, or of five minor criteria allows a clinical diagnosis of definite endocarditis. The Duke criteria Major Criteria 1. Positive blood culture Viridans streptococci Streptococcus , bovis, HACEK group, Staphylococcus aureus, community-acquired enterococci in the absence of a primary focus 2. Evidence of endocardial involvement - Positive echocardiogram - New valvular regurgitation Minor Criteria 1. Predisposition: predisposing heart condition or injection drug use 2. Fever 38.0°C 3. Vascular phenomena: major arterial emboli, septic pulmonary infarcts, mycotic aneurysm, intracranial hemorrhage, conjunctival hemorrhages, Janeway lesions 4. Immunologic phenomena: glomerulonephritis, Osler's nodes, Roth's spots, rheumatoid factor 5. Microbiologic evidence: positive blood culture but not meeting major criterion as noted previously or serologic evidence of active infection with organism consistent with infective endocarditis. Hepatosplenomegaly Infectious Splenic Infarct Salmonellosis Infectious Mononucleosis Hepatocellular/ Cholestatic Infectious Mononucleosis Hepatosplenomegaly Infectious Splenic Infarct Infectious Mononucleosis Hepatocellular/ Cholestatic Infectious Mononucleosis Hepatosplenomegaly Splenic Infarct Hepatocellular/ Cholestatic Infectious Infectious Mononucleosis Monospot test - positive Started on – piperacillin-tazobactam 4.5g IV q8 – metronidazole 500 mg IV q8 – vancomycin 1g IV q12 5th HOSPITAL DAY Blood CS - Streptococcus viridans Sensitive to penicillin and ampicillin Resistant vancomycin Vancomycin and metronidazole was then discontinued. Temperature (Celcius) 39.5 39 38.5 38 37.5 piperacillin-tazobactam 4.5g IV q8 37 Day 1 Day 2 Day 3 Hospital Day Day 4 Day 5 Repeat CXR – partial resolution of the bibasal pleural effusion – subsegemntal atelectasis are now seen at right paracardiac and left basal regions 6th HOSPITAL DAY Tazocin was discontinued Penicillin G 3M units IV every 4 hours Gentamicin 70 mg IV every 8 hours. 39.5 Temperature (Celcius) 39 38.5 38 37.5 37 piperacillin-tazobactam 4.5g IV q8 Day 1 Day 2 Day 3 Day 4 Hospital Day Day 5 Day 6 39.5 Temperature (Celcius) 39 38.5 38 Pen G 3M U IV q4 Gentamycin 70mg IV q8 37.5 37 Day 1 Day 2 Day 3 Day 4 Hospital Day Day 5 Day 6 8th HOSPITAL DAY Day-1 afebrile No note of recurrence of fever on the subsequent days. 39.5 39 38.5 38 37.5 37 36.5 36 D2- Pen G 35.5 D2- Genta 35 Day 1 Day 2 Day 3 Day 4 Day 5 Day 6 Day 7 Day 8 Hospital Day Day 9 Day 10 Day 11 Day 12 Day 13 Day 2 Day 4 Day 6 Day 7 Day 8 6-Jun 8-Jun 10-Jun 11-Jun 12-Jun Hgb 11.7 11.7 12.2 12.7 12.5 Hct 36.9 36.3 38 40.2 39.5 WBC 8.96 7.05 8.07 9.01 8.79 Seg 26 40 38 41 49 Lympho 56 46 50 49 44 Mono 17 13 11 8 7 Platelet ct 173T 270T 257T 532T 500T MCV 83.9 82.9 83.2 84.1 84.9 MCH 26.6 26.7 26.7 26.6 26.9 Day 1 Day 2 Day 4 Day 8 5-Jun 6-Jun 8-Jun 12-Jun Alkaline 543 phosphatase 439 480 TB 1.7 1.2 1 DB – IB 1.3 – 0.4 Na 0.8 0.5 – 0.5 141 138 135 K 3.3 3.9 3.5 BUN 6 13.01 Creatinine 0.8 1.5 Day 1 Day 2 Day 4 Day 8 Day 12 5-Jun 6-Jun 8-Jun 12-Jun 16-Jun Alkaline 543 phosphatase 439 480 251 TB 1.7 1.2 1 0.7 DB – IB 1.3 – 0.4 0.5 – 0.5 0.2 – 0.5 Na 0.8 141 138 135 136 K 3.3 3.9 3.5 4.1 BUN 6 13.01 16.99 Creatinine 0.8 1.5 1.5 CO2 29 Lipase 224 Amylase 28 SGOT 115 38 SGPT 129 71 FINAL DIAGNOSIS Infectious mononucloesis Streptococcus viridans bacteremia INFECTIOUS MONONUCLEOSIS Pfeiffer's disease Mono – Kissing disease Glandular fever Epstein-Barr virus – The cause of heterophile-positive infectious mononucleosis (IM) – Also associated with several human tumors, including nasopharyngeal carcinoma, Burkitt's lymphoma, Hodgkin's disease, and (in patients with immunodeficiencies) B cell lymphoma. - Family Herpesviridae - Consists of a linear DNA core - Two types of EBV that are widely prevalent in nature are not distinguishable by conventional serologic tests. Epidemiology Occurs worldwide. Most common in early childhood, with a second peak during late adolescence. By adulthood, more than 90% of individuals have been infected and have antibodies to the virus. Spread by contact with oral secretions More than 90% of asymptomatic seropositive individuals shed the virus in oropharyngeal secretions. Manifestations Symptoms Sore throat Malaise Headache Abdominal pain, nausea, or Chills Diarrhea 75 % 47 38 vomiting 17 10 Signs Lymphadenopathy Fever Pharyngitis or tonsillitis Splenomegaly Hepatomegaly Rash Periorbital edema Palatal enanthem Jaundice 95% 93 82 51 11 10 13 7 5 SPLENIC INFARCTION Splenic infarction during IM is very rare; To our knowledge, only five cases have previously been reported The pathogenesis of splenic infarction during IM remains unclear. In one case report of IM associated with splenic infarction, transient elevation of antiphospholipid antibodies was found and thought to be responsible for the splenic infarct. Acute EBV infection should be considered in the differential diagnosis of splenic infarction. This diagnosis should also be considered in patients presenting with unexplained acute abdominal pain. -Scottish Medical Journal, 2007 Splenic infarction due to infectious mononucleosis K Ashawesh, R Abdulqawi, BN Chandrappa, K.S. Srinivasan Department of medicine, Princess Royal Hospital, Telford, UK Splenic infarction is a rare feature of infectious mononucleosis Splenic infarction during acute EBV infection associated with the transient induction of antiphospholipid antibodies. Once other more common causes of splenic infarction, such as endocarditis and lymphoma, have been excluded, the possibility of viral-induced antiphospholipid antibodies should be considered. - Journal of clincal virology, 2006 Splenic infarction due to transient antiphospholipid antibodies induced by acute Epstein-Barr virus infection 18 year old Japanese man, with hereditary spherocytosis (HS) known to have developed splenic infarction following infectious mononucleosis (IM). On day 4 of admission, the patient complained of severe abdominal pain. Abdominal CT scan revealed findings of splenic infarction. Two months after the occurrence of splenic infarction, a splenectomy was performed. A pathohistologic examination of the resected spleen revealed no evidence of thrombosis or arterial occlusion. We assume that the cause of splenic infarction was insufficient blood flow to oxygenate the entire spleen during the acute enlargement of the spleen. - Splenic infarction after Epstein-Barr virus infection in a patient with hereditary spherocytosis Suzuki Y, Shichishima T, Mukae M, Ohsaka M, Hayama M, Horie R, Togano T, Miyazaki K, Ichinoe M, Iwabuchi K, Fujii H, Higashihara M. Department of Hematology, Kitasato University School of Medicine, Sagamihara, Japan LABORATORY FINDINGS WBC usually elevated and peaks at 10,000–20,000/L during the second or third week of illness. Lymphocytosis with >10% atypical lymphocytes. Low-grade neutropenia and thrombocytopenia are common during the first month of illness. Liver function is abnormal in >90% of cases. Aminotransferases and alkaline phosphatase are usually mildly elevated. Bilirubin is elevated in ~40% of cases. Monospot test Positive for infectious mononucleosis Specific for heterophile antibodies, not EBV. ~75% sensitive and ~90% specific compared with EBV-specific serologies. Can also be positive in patients with lumphoma, systemic lupus erythematosus, viral hepatitis, malaria, and some GI cancers SPECIFIC TEST FOR EBV Epstein-Barr Virus (EBV) viral capsid antigen IgG and IgM and, EBV nuclear antigen IgG by immunofluorescence Epstein-Barr virus antibody titers to help distinguish acute infection from past infection with EBV TREATMENT Self-limiting Symptomatic and/or supportive treatments Rest is recommended during the acute phase of the infection, but activity should be resumed once acute symptoms have resolved. Nevertheless heavy physical activity and contact sports should be avoided to abrogate the risk of splenic rupture, for at least one month following initial infection and until splenomegaly has resolved, as determined by ultrasound. MORBIDITY AND MORTALITY Fatalities from mononucleosis are near impossible in developed nations. CNS: – Meningitis, encephalitis, hemiplegiaand transverse myelitis. – Proposed as a risk factor for the development of multiple sclerosis, but this has not been affirmed. Hematologic: – Autoimmune hemolytic anemia (direct Coombs test is positive) and various cytopenias. THANK YOU