* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
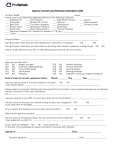
Download Occupational Health Program for Employees with Animal Exposures
Ebola virus disease wikipedia , lookup
Herpes simplex virus wikipedia , lookup
Cryptosporidiosis wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Oesophagostomum wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
West Nile fever wikipedia , lookup
Trichinosis wikipedia , lookup
Brucellosis wikipedia , lookup
Schistosomiasis wikipedia , lookup
Toxoplasmosis wikipedia , lookup
Marburg virus disease wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Henipavirus wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Hepatitis B wikipedia , lookup
Hepatitis C wikipedia , lookup
DLAM ZOONOSES AND LAB ANIMAL ALLERGY TRAINING Purpose of Program •This training is intended for research animal handlers and animal caretakers who are consistently in physical contact with the animals in DLAM facilities. •These employees are required to participate in an annual occupational health surveillance program for animal handlers. •This training is required annually. Possible Hazards in DLAM Facilities Allergic responses Animal bites, scratches, or other trauma Zoonotic diseases Animals and Health Risks LABORATORY ANIMAL ALLERGIES 15% of the general population is allergic to animals. •30 – 50% of those without a previous allergy history will develop an allergy to lab animals while working in that environment. •10 – 15% of these allergic workers will develop asthma. • Risk Factors for Development of Laboratory Animal Allergies Exposure to allergens Duration Frequency Intensity Previous allergic conditions Personal history of allergies/atopy/eczema Other predisposing conditions Illness Immunocompromised Pets Family history Common Lab Animal Allergy Sources Rats/ Mice--major allergens in urine/saliva Cats--sebaceous glands, hair, saliva Dogs--saliva, hair, skin Rabbits--fur, saliva, urine Birds--droppings Bedding Allergy Symptoms • • • • • Red, itchy, watery eyes, runny nose1 Sneezing, itchy, runny nose, congestion1 Red itching skin, welts, hives2 Asthma3 – cough (can be late-phase with symptoms starting several hours after leaving the animal facility), wheezing, chest tightness, shortness of breath Anaphylaxis4 – itching, hives, throat tightness, fainting, nausea, vomiting, diarrhea 1 = common, 2 = somewhat common, 3 = about 15 – 30%, 4 = rare Prevention of Lab Animal Associated Allergies Biosafety cabinets Filter top cages Ventilated cage racks Biobubble Choice of bedding Reduce time with animals Wash hands frequently Animal density Proper housekeeping practices Proper humidity Personal protective equipment (masks, respirator) Treatment of Lab Animal Associated Allergies Prevention is preferred Education of employees Proper use of personal protective equipment Re-assign employees when needed Medical treatment to reduce symptoms If you develop allergy symptoms to lab animals, contact University Employee Occupational Health Clinic (UEOHC at 966-9119) for an appointment for a medical evaluation Knowledge Review 1. Risk factors for developing laboratory animal allergies include: a. Amount of time spent around laboratory animals b. Family history of allergies c. Whether or not you have pets d. All of the above e. None of the above 2. Laboratory animal allergies can be prevented by using of which of the following? a. Good hygiene practices b. Biosafety Cabinets c. Respirators d. A & C e. All of the above Zoonoses Research personnel who handle animals and/or animal tissues are at risk for zoonotic disease transmission. • Zoonotic agents are infectious agents capable of being transmitted from animals to humans or from humans to animals. (TB to monkeys, flu to people) • •Zoonoses can cause minor or serious illness. In some cases, zoonotically infected individuals do not become ill. •On the other hand, some zoonoses can be extremely dangerous to people, especially those with a weakened immune system. Zoonoses Bacteria Exposure to feces/urine (e.g. Salmonella, Shigella, E. coli, Leptospira) Bites/scratches: Bartonella (cat scratch disease), Rat Bite Fever-Spirillum minor, Streptobaccilis moniliformis, Leptospirosis Viruses Herpes B virus from Macaques – potentially fatal to humans Rabies virus – potentially fatal to humans Lymphocytic Choriomeningitis Virus (LCMV)– rodents Parasites Gastrointestinal – Giardiasis, cryptosporidium, tapeworms (in urine and feces) Systemic – Toxoplasma (fatal defects in the fetus may occur if pregnant women are exposed to shedding cats) Dermatomycosis (ringworm) can be spread by contact with infected animal Transmission of zoonotic diseases can be prevented by prompt recognition and isolation of any ill animal Cats Cat scratch disease--Bartonella henselae Toxoplasmosis---Toxoplasma gondii Prevention--good hygiene Toxoplasmosis---Toxoplasma gondii Toxoplasmosis is caused by the protozoan parasite Toxoplasma gondii. Cats play an important role in the spread of toxoplasmosis. They become infected by eating infected rodents, birds, or other small animals. The parasite is then passed in the cat's feces in an oocyst form, which is microscopic. Kittens and cats can shed millions of oocysts in their feces for as long as 3 weeks after infection. A Toxoplasma-infected cat that is shedding the parasite in its feces contaminates the litter box or if allowed outside, can contaminate the soil or water in the environment as well. Toxoplasmosis---Toxoplasma gondii Toxoplasmosis is not passed from person-to-person, except in instances of mother-to-child (congenital) transmission and blood transfusion or organ transplantation. People can be infected by: Accidental ingestion of oocysts after cleaning a cat's litter box when the cat has shed Toxoplasma in its feces Accidental ingestion of oocysts after touching or ingesting anything that has come into contact with a cat's feces that contain Toxoplasma Drinking water contaminated with the Toxoplasma parasite Toxoplasmosis---Toxoplasma gondii Pregnant Women Mother-to-child (congenital) transmission A woman who is newly infected with Toxoplasma during pregnancy can pass the infection to her unborn child (congenital infection). The woman may not have symptoms, but there can be severe consequences for the unborn child, such as diseases of the nervous system and eyes. If you are pregnant or thinking about becoming pregnant and you work with cats, please contact EHS for a risk assessment. SheepQ Fever • • Q fever is a zoonotic disease caused by the organism Coxiella burnetii. Individuals acquire this infection by inhaling aerosols and contaminated dusts generated by animals or animal products. Q fever can also be contracted via: • • Direct or indirect contact with infected animal Contact with contaminated surfaces, clothing, equipment, bedding, etc Prior to working with or around sheep PAPR respirators or N95 masks are required to enter the animal housing area and laboratory that contain sheep. This requires annual training (EHS) and medical clearance and fit testing at UEOHC annually. The following should contact UEOHC for a medical screening and/or EHS for a risk assessment : Immunocompromised individuals and those with pre-existing heart valve conditions are at higher risk of infection and should be fully informed of the increased risks. Pregnant women or women who are considering becoming pregnant should also be fully informed of the increased risks. Swine Infected swine can transmit diseases to humans via the fecal-oral route, urine or contaminated water splashes, or direct contact Colibacteriosis (E. coli) Salmonella (Non-typhoidal) Leptospirosis Ringworm Rodents Rat Bite FeverSpirillum minor, Streptobaccilis moniliformis Leptospirosis Lymphocytic Choriomeningitis Virus (LCMV) Parasites Yersinia pestis--fleas from cats/ rodents in southwest Borrelia burgdorferi (Lyme Disease)- transmitted to animals/humans by infected ticks Non- Human Primates (NHP) Zoonotic hazards Herpes B virus (Macaques) Salmonella Tuberculosis Simian Immunodeficiency Syndrome (SIV), Simian T-Cell Lymphotropic Virus (STLV) Endogenous retroviruses Hepatitis A Hepatitis B Shigella dysenteriae Rabies Virus Feral animals represent the greatest risk Acquire animals that have been documented free of disease Post bite evaluation for need for Rabies booster, wound prophylaxis, tetanus Herpes B Virus (Cercopithecine Herpesvirus 1) Naturally occurring infection seen only in genus Macaca (rhesus, cynomolgus, pig-tailed, others). 80-100% imported adult rhesus macaques are Herpes B positive. In facilities where macaque monkeys are present saliva, genital secretions and conjunctival secretions are considered the primary body fluids associated with transmission Transmission has been documented through handling infected CNS & kidney tissue Feces, urine or other fluids may be contaminated Human disease is rare and has been identified in about 50 cases and well-documented in 26 cases. ~70% case fatality rate in humans Tuberculosis Transmitted to humans through exposure to infected animal/animal tissue. Also a reverse zoonosis, can be spread from humans to primates Screening is done by PPD in arm at UEOHC. Positive Chest tests indicate previous infection. x-rays are then required to rule out active disease. Simian Immunodeficiency (SIV) SIV is a lenti-virus that infects non-human primates in nature. Monkey SIV strains can infect humans, but does not lead to the development of AIDS. Unlike HIV infections in humans, SIV infections in their natural hosts are widely believed to be nonpathogenic. However, if SIV is used to infect an Asian rhesus macaque, for example, the animal will develop an AIDS-like illness similar to HIV infection in humans Hepatitis Viruses Hepatitis A: Enteric (oral/fecal spread) Non chronic carrier state Hepatitis Viruses Hepatitis B Bloodborne pathogen Low mortality (1 % case fatality rate) Up to 10% of those infected become chronic carriers with high incidence of cirrhosis and liver cancer. Vaccine required (or declination) Hepatitis Virus Hepatitis C Bloodborne. Disease is milder in comparison with Hepatitis B, however there is a higher rate of chronic carriers. No vaccine, however, treatment within weeks of infection can prevent chronic disease. Routes of Exposure for Zoonotic Diseases Routes of Exposure • • • Bites and scratches from infected animals Needlestick injuries with contaminated needles or scalpels Eye and mucous membrane exposure to body fluids or particulates from infected animals Percutaneous Exposure Zoonotic diseases are commonly spread percutaneously (bites, scratches, needlesticks): Some organisms are Staphlyloccus aureus, Bartonella henselae Proper wound care/ tetanus immunization Appropriate antibiotic prophylaxis Bacterial Infections from Bite Wounds >200 species of bacteria in the mouths of many animals, including humans. Streptococcal species, staphylococcal species, tetanus. Bite wounds should be thoroughly cleaned. Prophylaxis for moderate to deep bites with Amoxacillin/clavulinic acid (Augmentin). Exposure Procedures Immediate Response: Mucous membrane: flush in an eye wash or potable water for a minimum of 15 minutes. Non-intact skin exposures: Wash with soap and water or antiseptic for 15 minutes. REPORT ANY INJURIES AND ILLNESSES TO PI/LAB SUPERVISOR AND IMMEDIATELY REPORT TO UEOHC (962-9119) Knowledge Review 3. Zoonotic agents are infectious agents capable of being transmitted from animals to humans only? a. True b. False 4. A vaccine for _____________ is available for DLAM employees who work with/around research animals. a. Hepatitis B b. Hepatitis C c. Herpes B d. All of the above 5. Zoonotic diseases cannot be spread by: a. Needlesticks with contaminated needles b. Contaminated materials being splashed into the eyes c. Contaminated materials coming into contact with gloved hands d. Being bitten by an infected animal Access Control and Staff Training Training (more extensive & periodic) Personnel must enroll in medical surveillance program Restricted/controlled access Written emergency response plans Hazardous Agents Used in Research Animals Animals exposed to biological, radiological, or chemical hazards can create a risk of exposure to people. When working with animals that have been exposed to hazardous agents, precautionary measures (use of PPE, engineering and administrative controls) should be taken. Read the Use of Biological, Chemical, Radiation forms posted on the animal room/cubicle doors Minimize Risk Wear proper PPE (respirators, gloves, Tyvek suit, gown, shoe covers, etc.) as indicated by signage. Use gloves when handling animals & change gloves between animals. Wash your hands as soon as possible after removing gloves. No eating, drinking, smoking, applying cosmetics or handling contact lenses in any DLAM facility. Minimize Risk Keep food intended for human consumption separate from animal food. Report any animals that appear to be ill. Report any occupational illness or injury to your lab manager and/or PI and immediately report to UEOHC (919-966-9119, M-F 8:30-4:30) Immunocompromised/Pregnant Individuals Immunocompromised individuals and pregnant women should be aware of the potential zoonotic hazards that may be present in the workplace. If you are undergoing chemotherapy/radiation therapy, being treated with steroids or other drugs that could cause immunosuppression and/or you are pregnant or plan on becoming pregnant, please notify EHS to determine appropriate protective measures and monitoring.