* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download infarcts
Cardiovascular disease wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Cardiac surgery wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Coronary artery disease wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
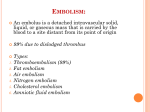
Hemostasis and Thrombosis We are not composed of static pipes that transmit blood, so we have to understand how the normal vessel constituents interact with blood normally!!!! Hemostasis is natural process that maintains blood fluidity while also controlling vascular injury repair producing a local hemostatic plug PLUMBER’S TOOL Hemostasis Integrity of small blood vessels Adequate numbers of platelets Normal amounts of coagulation factors Normal amounts of coagulation inhibitors Adequate amounts of calcium ions in the blood Role of endothelium in hemostasis Antiplatelet properties • physical barrier • Prostacyclin synthesis • Nitric oxide synthesis Anticoagulant properties • Heparin-like molecules (+antithrombin III inactivate thrombin) • Thrombomodulin (+thrombin activates Protein C that digests factors V and VII) Fibrinolytic properties • Synthesis of t-PA Pro thrombotic properties • Synthesis of von Willebrand factor vWF • Cytokine (Il-1, TNF) stimulation causes release of tissue factor which in turn activates extrinsic clotting factors • Synthesis of plasminogen activator inhibitors (PAIs) Role of platelets in hemostasis: Note: Platelets contain 2 types of storage granules: Alpha granules store fibrinogen, PDGF, coagulation factors V and VIII. Dense or delta granules contain ADP, ATP, ionized calcium, histamine, serotonin, and epinephrine. Platelet adhesion: reaction between platelet surface receptors, vWF, and collagen Platelet secretion: release of granule secretory products that promote platelet-plug formation Platelet aggregation: ADP and thromboxane promote primary hemostasis. Platelet contraction and fibrin formation lead to secondary hemostatic plug Role of coagulation cascade Coagulation factor activation occurs on phospholipid surfaces derived from endothelial cell injury. This helps to localize the reaction. Extrinsic vs. Intrinsic coagulation distinctions are not clear in vivo. Inhibition of coagulation activation is extremely important and highly dependent on endothelial integrity. Sequence of events: • Initial injury • Arteriolar vasoconstriction Neurogenic reflexes Local endothelin release (endothelium) • Exposure of subendothelial matrix (collagen) and platelet activation (primary hemostasis) • Tissue factor release (phospholipids) stimulates the coagulation cascade with net fibrin deposition (secondary hemostasis) • Fibrin-platelet plug is formed. Plasmin activation helps limit plug extension Downloaded from: Robbins & Cotran Pathologic Basis of Disease Downloaded from: Robbins & Cotran Pathologic Basis of Disease Downloaded from: Robbins & Cotran Pathologic Basis of Disease Thrombosis Inappropriate activation of the hemostatic process in uninjuried vasculature or formation of thrombus in the setting of relatively minimal vascular injury Virchow's Triad –predisposing factors Downloaded from: Robbins & Cotran Pathologic Basis of Disease Factors predisposing to thrombosis Hypercoagulability Any alteration of the coagulation pathways that predispose to thrombosis • Primary (genetic) Factor V and prothrombin gene mutations most frequent • Factor V becomes resistant to protein C inactivation • Prothrombin levels elevated • Secondary (acquired) • Bed rest – immobilization, obesity, cancer, atrial fibrillation, myocardial infarction, tissue damage (surgery, burns) Abnormalities of blood flow – turbulence Endothelial injury Local areas of stasis Disrupt laminar flow • Moves platelets from center of flow to the vessel wall • Prevent dilution of activated clotting factors by flowing blood • Slow down the inflow of clotting factor inhibitors • Promotes endothelial cell activation Thrombus morphology Arterial thrombus: • • • • Begin at points of injury or areas of turbulence. Extend in a retrograde fashion Mural thrombi form in heart or large vessels Lines of Zahn are indicative of arterial thrombi (adherent masses of blood that demonstrate areas of pale alternating with areas of red) • Arterial thrombi may or may not be occlusive Venous thrombus: • • • • • Begin in areas of stasis Extend in a antegrade fashion Are almost always occlusive Contain lots of RBC’s Long - forming a cast of vein with markings on them from venous valves Venous Thrombi: Clinical Venous trombus Arterial thrombus Arterial Thrombi Morphology Arterial trombus Downloaded from: Robbins & Cotran Pathologic Basis of Disease Cardiac thrombi Thrombi may form in any chamber of the heart on the valve cusps More common in the atrial appendadages, especclially of the right atrium, and on mitral and aortic valvescalled vegetations which may be seen in infective endocarditis and non – bacterial endocarditis Are mural (non – oclusive) as are the mural thrombi encountered in the aorta in atherosclerosis and in aneurysmal dilatations Fate of a thrombus (venous or arterial) Propagation: continued growth may obstruct critical vessel. Embolization: dislodgement of thrombus or parts of it may cause obstruction downstream. Dissolution: fibrinolysis may dissolve clot. Organization: thrombus induced injury leads to inflammation and fibrosis. Recanalization may re-establish some vascular flow. Venous thrombi fates Effects of thrombosis Ischemia Congestion Heart valve disease DIC Embolism Disseminated Intravascular Coagulation Sudden onset of fibrin thrombi in the microcirculation with consumption of coagulation factors and formation of fibrin degradation products A potential complication of any disease state/process associated with the widespread activation of thrombin Not usually visible “grossly”, readily apparent microscopically and can cause diffuse circulatory insufficiency, particularly in the brain, lungs, heart, and kidneys development of the multiple thrombi rapid concurrent consumption of platelets and coagulation proteins (synonym consumption coagulopathy); at the same time, fibrinolytic mechanisms are activated bleeding disorder. DIC Obstetrical complications Infection trauma, burn, surgery) Vasculitis and vascular malformations promielocytic leucemia Tissue injuryies pancreatic, prostate, lung, stomach carcinoma Sanguine disorders gram negative, meningococc, aspergillosis, malaria Neoplasm abruptio placentae, ritention of death fetus, septic abortion, amniotic liquid embolism hemangiom, anevrism) Varies intravascular hemolisis, hepatopaties Pathophysiology of disseminated intravascular coagulation. Downloaded from: Robbins & Cotran Pathologic Basis of Disease DIC Embolism Embolism is the process of partial or complete obstruction of some part of the cardiovascular system by any mass carried in the circulation. The transported intravascular mass detached from its site of origin is called embolus ( solid, liquid, or gaseous mass). 90% of all emboli are derived from a thrombus. Types of emboli A. Depending upon the matter in the emboli: Solid – detached thorombi, atheromatous materal, tissue fragments, parasites, foreign bodies Liquid – fat globules, amniotic fluid, bone marrow Gaseous- air, other gases B. Depending upon wheter infected or not Bland, when sterile Septic, when infected C. Depending upon source of emboli Cardiac emboli Arterial emboli Venous emboli Lymphatic emboli D. Depending upon the flow of blood Paradoxical embolism : In patients with persistent oval hole, embolism from the venous system can pass from the right to the left side of the heart and reach the systemic circulation. Retrograde embolism: circulating emboli in the reverse sense of blood flow - e.g. metastatic deposits in the spine from prostate carcinoma (the spread ooccurs by retrograde embolism through intraspinal which carry tumour emboli from large thoracic and abdominal veins veins due to increased pressure in body cavities). Direct or ortograde embolism: emboli originating from the left heart and systemic circulation reach to cerebral, renal or splenic arteries; embolism from leg veins reach the lung Paradoxical emboli • arise in venous system and pass through a hole in interventricular septum of the heart and end up in the arterial system (possible stroke). Sources of artherial and venous emboli Concequences of embolism Obstruction of a vessel ->ischemia (with the instalation of stroke, gangrene or swelling of the brain, e.g) Infarction of the organ or its affected part – ischaemic necrsis in the lower limbs, spleen, brain, intestine septicemia (septic emboli) Sudden death by massive pulmonary embolism, coronary embolism, embolism in the middle cerebral artery Arteritis or mycotic aneurysm formation from bacterial endocarditis Myocardial infarction Pulmonary Thromboembolism • 10% of hospital patients die from this (50,000/yr). • 95% originate in the deep veins of the legs above knee. • Saddle embolus is one that lodges at the common iliac bifurcation. • Most are asymptomatic due to small size. • With greater than 60% of pulmonary arterial system blocked patients develop sudden cardiac death, cor pulmonale, or shock. • Multiple emboli may result in pulmonary hypertension. PULMONARY EMBOLISM Concequences of pulmonary embolism Thromboembolus in a large pulmonary artery Hhromboembolus small peripheral artery Systemic Thromboembolism Arterial emboli 80% arise in the heart (mural thrombi). Major lodgment sites include lower extremities (75%) and brain (10%). Intestines, kidneys, and spleen are also targets. Consequences dependent on size of emboli, caliber of vessel, collateral circulation, and tissue sensitivity to ischemia Bone marrow embolus in the pulmonary circulation Downloaded from: Robbins & Cotran Pathologic Basis of Disease Other types of emboli Fat Emboli • Major source is long bone fracture. • They develop in 90% of severe fractures but most are asymptomatic. • In cases of significant emboli development consequences include pulmonary insufficiency, stroke, anemia, and thrombocytopenia. (10% fatal) Air Emboli • • • • Causes include chest wall injury or obstetric procedures. 100 cc or more of air is clinically significant. Bends results from decompression problems. Caisson disease is chronic bends. Amniotic Fluid Emboli • 1/50,000 deliveries • Mortality rate > 80% • Causes include placental tears and uterine vein rupture. AIR EMBOLISM - symptoms AIR EMBOLISM Septic embolism • Causes include IV drug use, right-sided infective endocarditis, and septic thrombophlebitis. • symptoms and signs of pneumonia or sepsis. Foreign body embolism • caused by introduction of particulate matter into the pulmonary arterial system - IV injection of inorganic substances: talc by heroin users or elemental mercury by patients with mental disorders. Tumor embolism • complication of malignancy (usually adenocarcinoma) • neoplastic cells from an organ enter the systemic venous and pulmonary arterial system, where they lodge, proliferate, and obstruct flow. Fatty emboli Metastatic embolus Amniotic Fluid Emboli Atheroemboli (Kidney) Septic embolus Infarction Def.: ischemic necrosis of tissue distal to an area of arterial occlusion or in an area of obstructed venous outflow Most result from atherosclerosis - the major cause of MI and stroke. Commonly seen in kidney, spleen, lung, intestine, heart and brain Usually located beneath the tunica of the organ. Classified: • on the basis of their colour (reflecting the amount of hemorrhage): red (hemorrhagic) white (anemic) • presence or absence of microbial infection: septic bland Influencing Factors • Nature of vascular supply: alternative blood supply is most important (lung and liver) • Rate of development: collateral development limits infarction. • Tissue vulnerability: neurons (3 min), heart (25 min), connective tissue (hours) • Blood oxygen content: patients with anemia or those cyanotic are more susceptible. Morphology Red (hemorrhagic) infarcts occur : • with venous occlusions (ovarian torsion); • in loose tissues (lung), which allow blood to collect in the infarcted zone • in tissues with dual circulations (e.g., lung and small intestine), permitting flow of blood from the unobstructed vessel into the necrotic zone • in tissues that were previously congested because of sluggish venous outflow • when flow is re-established to a site of previous arterial occlusion and necrosis (e.g., following fragmentation of an occlusive embolus or angioplasty of a thrombotic lesion) White (anemic) infarcts occur with arterial occlusions in solid organs with end-arterial circulation (heart, spleen, and kidney), where the solidity of the tissue limits the amount of hemorrhage Shape of infarct • Wedge-shape: infarct of liver, spleen, kidney, lung; • Map-like shape: myocardial infarct; • Segmental shape: intestinal infarct. At early stage, all infarcts are poorly defined. The margins of both types of infarcts tend to become better defined with time by a narrow rim of hyperemia and/or hemorrhage attributable to inflammation at the edge of infarct Histopathology - - - dominant histologic characteristic: • Coagulative necrosis: liver, spleen, kidney, myocardium, lung • Liquefactive necrosis: brain, pancreas The infarct is a kind of tissue necrosis among which pyknosis, karyorrhexis and karyolysis can be seen. The outline of original tissue can be discerned despite that the cells are dead. Anemic infarct contains few RBC; while hemorrhagic infarct has engorgement and hemorrhage; The pathological changes secondary to infarct: hyperemia, hemorrhage, inflammation, organization. Most infarcts are ultimately replaced by scar tissue Infarction Red (Hemorrhagic) Anemic (White) Pulmonary infarct Embolization to the small vessels in lung may cause ischemic necrosis of tissue or infarct Heart infarction Infarction 1 to 2 days in duration contraction band necrosis Infarction is about 3 to 4 days old Infarction of 1 to 2 weeks in age Old infarction Aneurism of ventricle Rupture of the myocardium Intestinal infarction Arterial thrombosis/ embolism Venous thrombosis Nonoclussive ischemia/ Miscellaneous -radiation injury -volvulus -stricture -herniation Liver Infarct Kidney infarct Myocardial Infarction Acute Myocardial Infarction interruption of blood supply to a part of the heart, causing necrosis of heart muscle due to ischemia Mechanism Subendocardial (prologend ischemia caused by partial occlusion of a coronary) Transmural (complete occlusion of a major coronary) Common localisations and the regions involved in myocardial infarction Complications of myocardial infarction Arrrithmias Congestive heart failure Cardiogenic shock Mural thrombosis and thrmboembolism Rupture Cardiac aneurysm Pericarditis Postmyocardial infarction syndrome Shock Shock = Cardiovascular Collapse Results from systemic hypoperfusion due to either a reduction in blood volume or cardiac output. Types of Shock • Cardiogenic: MI, arrhythmia, tamponade, outflow obstruction • Hypovolemic: traumatic hemorrhage, severe burns, disease induced hemorrhage. • Neurogenic: Cord transection (peripheral pooling) • Anaphylactic: IgE mediated vasodilation and edema • Septic: Systemic infection primarily gram-negative (endotoxic). Cytokine mediated vasodilation, myocardial injury, and DIC. Stages of Shock • Initial non progressive stage: tachycardia, vasoconstriction, renal conservation of water. • Progressive stage: lactic acidosis, vasodilation, hypoxia, organ failure. • Irreversible stage: Lysosome release, ischemic bowel syndrome, acute tubular necrosis, death. Clinical Course • Hypovolemic/Cardiogenic: hypotension, weak rapid pulse, tachypnea, cool clammy cyanotic skin. • Septic shock: warm red skin. 80% with hypovolemic shock survive. 80% with cardiogenic or endotoxic shock die. Model of septic shock