* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Hemodynamic disorders
Survey
Document related concepts
Transcript
HEMODYNAMIC DISORDERS
Manar hajeer, MD
University of jordan
Faculty of medicine, pathology departement
EDEMA
The term edema signifies increased fluid in the
interstitial tissue spaces.
Fluid collections in different body cavities are
variously designated:
Hydrothorax: in the pleural cavity.
Hydropericardium: in the pericardial cavity.
Hydroperitoneum (ascites): in peritoneal cavity.
Anasarca is a severe and generalized edema
with profound subcutaneous tissue swelling.
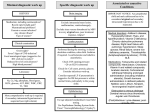
CAUSES OF EDEMA
I. Increased hydrostatic pressure and results from
impaired venous return
1. Local increase: such as deep venous thrombus in the
lower extremity causes edema in the affected leg.
2. Generalized increase in venous pressure, such as in
heart failure.
3
II. Reduced Plasma osmotic pressure
- Causes
1. Loss of albumin from kidney.
2. Reduced albumin synthesis : Occurs in cirrhosis and
protein malnutrition.
3. Protein losing enteropathy.
III. Lymphatic Obstruction:
1. Parasitic infection (filariasis) : causes inguinal lymph
node fibrosis; so results in massive edema of the
lower extremity and external genitalia
(elephantiasis).
2. Axillary lymph node resection in breast cancer can
obstruct lymphatic drainage, resulting in lymphedema of
the arm.
IV. Sodium and water retention:
can occur with any compromise of renal function, as in
poststreptococcal glomerulonephritis and acute renal
failure .
V. Inflammation:
Acute and chronic, due to increase blood flow and
hydrostatic pressure. (Localised edema)
The edema fluid occurring with volume or pressure
overload, or under conditions of reduced plasma protein,
is typically a protein-poor transudate.
Conversely, because of the increased vascular
permeability, inflammatory edema is a protein-rich
exudate.
HYPEREMIA AND CONGESTION
The terms hyperemia and congestion both indicate a
local increased volume of blood in a particular tissue.
1.Hyperemia: is an active process resulting from
augmented blood flow due to arteriolar dilation (e.g., at
sites of inflammation or in skeletal muscle during
exercise).
The affected tissue is redder than normal because of
engorgement with oxygenated blood.
2.Congestion is a passive process resulting from impaired
venous return out of a tissue.
Systemic congestion, as in cardiac failure.
Local congestion, as in isolated venous obstruction.
The tissue has a blue-red color (cyanosis), as worsening
congestion leads to accumulation of deoxygenated
hemoglobin.
HEMORRHAGE
Hemorrhage is extravasation of blood from vessels
into the extravascular space.
May be:
1. External hemorrhage.
2. Within a tissue (hematoma)
3. Large bleeds into body cavities;
a. Hemothorax: Blood in the pleural cavity.
b. Hemopericardium: Blood in pericardium.
c. Hemarthrosis : Blood in in joints.
4. Small bleeds
I. Petechiae are minute 1-2 mm bleeds in skin or mucous membranes,
Causes:
A-Low platelet counts (thrombocytopenia),
B-Defective platelet function (Aspirin)
C-Localy increased intravascular pressure.
D-Clotting factor deficiency.
II. Purpura are 3 to 5 mm bleeds results from above causes in addition
to trauma, vascular inflammation (vasculitis), or increased
vascular fragility.
III. Ecchymoses : Larger (1- to 2-cm) subcutaneous hematomas
(bruises).
CLINICAL SIGNIFICANCE OF HEMORRHAGE
DEPENDS ON:
1. The volume of and Rate of bleeding
a. Rapid loss of up to 20% of the blood
volume, or slow losses of even of larger amounts, may
be insignificant.
b. Greater losses can cause hemorrhagic (hypovolemic)
shock .
2. Site of bleeding:
Bleeding that would be trivial in the subcutaneous tissues can
cause death if located in the brain .
Note: Chronic or recurrent external blood loss ( peptic ulcer or
menstrual bleeding) may result in iron deficiency anemia.
HEMOSTASIS AND THROMBOSIS
Hemostasis : tightly regulated processes that maintain
blood in a fluid, clot-free state in normal vessels while
inducing the rapid formation of a localized hemostatic
plug at the site of vascular injury.
The pathologic form of hemostasis is thrombosis.
Thrombosis: blood clot (thrombus) formation in
uninjured vessels or thrombotic occlusion of a vessel
after relatively minor injury.
Both hemostasis and thrombosis involve three
components: the vascular wall, platelets, and the
coagulation cascade.
CAUSES OF THROMBOSIS
Virchow's triad:
(1) endothelial injury,
(2) stasis or turbulence of blood flow,
(3) blood hypercoagulability.
1- ENDOTHELIAL INJURY
exposes highly thrombogenic subendothelial
extracellular matrix, allowing platelets to adhere
and be activated (aggregation)
Intact endothelial cells maintain liquid blood
flow by actively inhibiting platelet adherence,
preventing coagulation factor activation, and
lysing blood clots that may form.
Endothelial cells can be stimulated by direct
injury. Such stimulation results in local
thrombus formation.
Examples of endothelial injury:
1. Endocardial injury in myocardial infarction (thrombus
formation within the cardiac chambers)
2.Ulcerated plaques in atherosclerotic arteries.
3.At sites of traumatic or inflammatory vascular injury
(vasculitis)
2- ALTERATIONS IN NORMAL BLOOD FLOW
Turbulence contributes to arterial and cardiac
thrombosis by causing endothelial injury or dysfunction.
Stasis is a major contributor to the development of
venous thrombi.
CAN BE SEEN IN SEVERAL CLINICAL
SETTINGS:
1- Ulcerated atherosclerotic plaques (turbulent) .
2- Abnormal aortic and arterial dilations, called aneurysms
(stasis).
3- Acute myocardial infarction results in focally
noncontractile myocardium; can lead to aneurysm
formation.
4- Hyperviscosity syndromes (such as polycythemia;)
increase resistance to flow and cause small vessel stasis.
5- Deformed red cells in sickle cell anemia cause vascular
occlusions, with the resultant stasis also predisposing to
thrombosis.
3- HYPERCOAGULABILITY
Primary (genetic) and secondary (acquired) disorders .
A- Inherited causes of hypercoagulability:
Mutations in the factor V gene and the prothrombin
gene are the most common.
Deficiencies of anticoagulants such as protein C or
protein S (rare)
B. Acquired hypercoagulability
1.Oral contraceptive use and hyperestrogenic state of
pregnancy .
2.Prolonged bed rest or immobilization .
3.Myocardial infarction.
4. Disseminated cancers, release of mucin in
adenocarcinoma predisposes to thrombus formation (migratory
thrombophlebitis, or Trousseau's syndrome).
FATE OF THE THROMBUS
1. Propagation: Thrombus enlargement by
accumulation of additional platelets and fibrin.
2. Embolization: Fragment of thrombus is transported
elsewhere in the vasculature.
3. Dissolution: In newly formed thrombus,, activation of
fibrinolysis may lead to its rapid shrinkage and complete
dissolution.
Note: older thrombi, are more resistant to plasmin-induced
lysis .
4. Organisation and recanalization: Older thrombi
become fibrosed and capillary channels may form and
establish the continuity of the original lumen.
5. Bacterial seeding of thrombus serve as a culture
medium, and the resulting infection may weaken the
vessel wall, leading to formation of a mycotic aneurysm.
CLINICAL CORRELATIONS: VENOUS
VERSUS ARTERIAL THROMBOSIS
1- Venous thrombi by obstructing the venus drainage can
cause swelling and edema, but are most worrisome
because they can embolize to the lungs and cause death.
2- Arterial thrombi can embolize. However, they mainly
obstruct vessels (in coronary and cerebral arteries ) to
cause myocardial and cerebral infarction.
Also cardiac thrombi in the setting of myocardial
infarction can give systemic embolization (brain,
kidneys, and spleen).
VENOUS THROMBOSIS
1. Superficial venous thrombi:
- Arise in the saphenous vein particularly in varicose
veins; these rarely embolize but can cause edema from
impaired venous outflow, leading to varicose ulcers.
II. Deep venous thromboses ("DVTs") : Occur in the
larger leg veins at or above the knee ( popliteal, femoral,
veins). May be asymptomatic. Serious because they can
embolize.
EMBOLISM
An embolus is a detached intravascular solid, liquid, or
gaseous mass that is carried by the blood to a site distant
from its point of origin.
Virtually 99% of all emboli represent some part of a
dislodged thrombus, hence the term thromboembolism.
Rare forms:
Air embolism, fat embolism, amniotic fluid embolism.
The consequences of thromboembolism include ischemic
necrosis (infarction) of downstream tissue.
Two forms:
1.Pulmonary thromboembolism.
2.Systemic thromboembolism.
PULMONARY THROMBOEMBOLISM
In 95% of cases, venous emboli originate from thrombi
within deep leg veins, above the knee.
They are carried through progressively larger channels
and pass through the right side of the heart before
entering the pulmonary vasculature.
CLINICAL FEATURES OF PULMONARY
THROMBOEMBOLISM:
a. Clinically silent: 60% to 80% of emboli esp. small ones.
b. Sudden death or right sided heart failure (acute cor
pulmonale):A large embolus that blocks a major pulmonary
artery or pulmonary trunk (saddle embolus)
c. Pulmonary hemorrhage: embolic obstruction of medium-sized
arteries and subsequent rupture of capillaries, with no
infarction since the area also receives blood through bronchial
arteries.
d- Pulmonary hypertension and chronic right ventricular
failure (chronic cor pulmonale): Multiple emboli occurring
over time.
SYSTEMIC THROMBOEMBOLISM
80% arise from intra cardiac thrombi.
The remainder originate from aortic aneurysms and
thrombi overlying ulcerated atherosclerotic plaques.
Common arteriolar embolization sites :
a. The lower extremities (75%).
b. Central nervous system (10%).
c. Intestines, kidneys, are less common.
Note: Arterial emboli often cause infarction
FAT EMBOLISM
Caused by:
- Soft tissue crush injury or long bone fractures, with
release of microscopic fat globules into the circulation.
Note: Fat embolism occurs in some 90% of individuals
with severe skeletal injuries, but less than 10% show
fat embolism syndrome.
FAT EMBOLISM SYNDROME
a. Pulmonary insufficiency (tachypnea, dyspnea,)
b. Neurologic symptoms (irritability and restlessness to
coma)
c. Anemia, thrombocytopenia.
AIR EMBOLISM
Gas bubbles within circulation can coalesce and obstruct
vascular flow.
a. Small venous gas emboli have no deleterious effects,
but sufficient air that enter the pulmonary circulation
during obstetric procedures or due to a chest wall
injury can cause hypoxia.
b. Large venous gas emboli may arrest the heart .
INFARCTION
An infarct is an area of ischemic necrosis caused by
occlusion of either the arterial supply or the venous
drainage in a particular tissue.
Nearly 99% of all infarcts result from thrombotic or
embolic events, and almost all result from arterial
occlusion.
Although venous thrombosis can cause infarction, it
more often merely induces venous obstruction and
congestion.
Infarcts are classified on the basis of their color
(reflecting the amount of hemorrhage) and the presence
or absence of microbial infection. Therefore, infarcts
may be either:
Red (hemorrhagic)
White (anemic)
Either septic or bland.
RED INFARCTS
(1) With venous occlusions (such as in ovarian torsion).
(2) In loose tissues (such as lung).
(3) In tissues with dual circulations such as lung and small
intestine.
(4) In tissues that were previously congested because of
sluggish venous outflow.
(5) When flow is re-established to a site of previous arterial
occlusion.
WHITE INFARCTS
Arterial occlusions or in solid organs (such as heart,
spleen, and kidney), where the solidity of the tissue
limits the amount of hemorrhage.