* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download CardioVascular Assessment Lab
Management of acute coronary syndrome wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Heart failure wikipedia , lookup
Electrocardiography wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Aortic stenosis wikipedia , lookup
Artificial heart valve wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Coronary artery disease wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Cardiac surgery wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
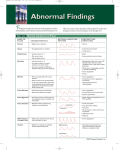
CardioVascular Assessment Lab C Ruckdeschel RN, BSN Objectives Review Anatomy of Heart Review Vascular System Review Physiologic basics for Cardiovascular System Objectives: Identify Skills to assess cardiovascular System: Pulse Peripheral vascular assessment Heart Sounds Blood Pressure Anatomy of Heart Right side of heart - receives deoxygenated blood from systemic circulation - LOW PRESSURE Left Side of the heart - receives oxygenated blood from pulmonary circulation and pumps it into systemic circulation - HIGH PRESSURE Chambers and Valves Rt Atrium RT AV Valve (Tricuspid) Rt Ventricle Rt semilunar (Pulmonic) Left Atrium Lft AV Valve (bicuspid, Mitral) Left Ventricle Left semilunar (Aortic) Great Vessels of the Heart Vena Cava - deoxygenated blood brought to heart IVC (inferior vena Cava) SVC (superior Vena Cava) Pulmonary Artery - deoxygenated blood from rt ventricle to pulmonary capillaries Pulmonary Veins - oxygenated blood from pulmonary capillaries to lft atrium Aorta Ascending Arch Descending Thoracic Abdominal http://www.youtube.com/wat ch?v=PgI80Ue-AMo Coronary Arteries Arteries that arise from base of aorta and supply myocardium with richly oxygenated blood LCA LAD Circumflex RCA Cardiac Conduction System • Heart is innervated by Autonomic nervous system Sympathetic : stimulates Parasympathetic: slows SA Node (Sinoatrial node): located in right atria, generates impulses that travel through the conduction system & produce cardiac muscle contraction. AV Node (atrioventricular node): located in the atrial septum Bundle of His: right and left bundle branches Purkinjie fibers: located in ventricular myocardium, where ventricular contraction takes place 12 Lead EKG • Chest X-ray Common Cardiovascular Problems CAD (Coronary Artery Disease) HTN (Hyypertension) > 80% of US population RHD (Rheumatic Heart Disease) - Sequelae of beta hemolytic strep infections resulting in valvular damage, more likely seen In older adults BE (Bacterial Endocarditis) - bacteremia causes valvular damage CHD (Congenital Heart Disease) – greatest portion diagnosed early in life Peripheral Vascular Anatomy Aorta Arteries Arterioles Capillaries Venules Veins Vena Cava Important Vessels Accessible arteries: Temporal, Carotid, Aorta, Brachial, Ulnar, Radial, Femoral, Popliteal, Doraslis pedis, Posterior Tibial Accessible veins: Jugular, Superficial & deep arm veins, Femoral vein (deep), Popliteal vein (deep), saphenous (superficial) Physiologic Basics Myocardium - muscle layer of the heart that allows it to act as pump Cardiac Output = HR x SV Heart Rate (pulse) = beats per minute Blood Pressure = SVR x CO Electrical conduction of the heart Assessing: Heart Sounds Heart Sound Review Location Aortic: 2nd ICS, RSB (s2 is loudest) Pulmonic: 2nd ICS, LSB (s2 is loudest) Erbs Point: 3rd ICS, LSB Tricuspid: 4th ICS, LSB (s1 is loudest) Mitral (Apex): 5th ICS, MCL (s1 is loudest) S1: represents ventricular contraction & ejection: S1 sound is produced by closing of AV valves (tricuspid and Mitral valves) S2: represents ventricular relaxation & filling: S2 sound is produced by closing of semilunar valves: Aortic and Pulmonic valves http://www.youtube.com/ watch?v=Ge12P7u0aQo Assessing: Heart Sounds Assessing: Heart Sounds Obtain History Risk factors/lifestyle diet, exercise smoking cholesterol stress, palpitations dyspnea/orthopnea edema fatigue - relationship to exercise chest pain Location substernal? Radiate precordial? Quality crushing? Associated N/V Related to activity? Obtain History Any medications?ty pe doseside effectsexpected effectstake as prescribed? Pacemaker Typebattery checkPresence of AICDautomated internal defibrillator Assessing: Heart Sounds Obtain History Past Health History Diabetes Dependent edema congenital heart defect CAD Rheumatic fever Most recent EKG, stress EKG Other diagnostics Obtain History Past Family History Angina Heartdisease MI,StrokeDM, Hyperlipidemia Sudden death age? Assessing: Heart Sounds Inspection Bare chest Quiet room, Privacy Note: symmetry of chest, any pulsatile areas, discolorations Palpate Precordium palpate 5 sites for: Heave (with palmer surface), thrust Thrill (with base of finger of heel of hand (bony part)) palpable murmur » cat purring Thrills - indicative of obstructed flow fine palpable rushing sensation R or L 2nd ICS - Aortic or pulmonic stenosis When palpate precordium use other hand to palpate carotid artery S1 should coincide with carotid impulse Assessing: Heart Sounds Auscultate Use diaphragm and bell of stethoscope start with diaphragm, (S1 and S2 relatively high pitched) use bell to listen for S3 and S4 heart sounds - S1 and S2 rate rhythm - regular (NSR), irregular (warrants investigation) extra sounds? Murmurs? Auscultation: want to hear crisp, distinct S1 and S2 S1 > at apex S2 > at base Assessing: Heart Sounds BE Systematic!! APE TO MAN Listening for S1 and S2 interval between S1 and S2 should be silent heart sounds not heard best directly over valve which produces it, but in direction of blood flow there are specific sites where each valve sound is best heard http://www.youtube. com/watch?v=2aO0 HKIP3vI After Auscultating Heart Sounds..... Perfect time to auscultate Apical Pulse. Count for one full minute, each cardiac cycle. Note rate & rhythm What is a Pulse? • The ventricles pump blood into the arteries at about 72 bpm. The blood causes an alternating expansion and recoil creates a pressure wave which travels through all of the arteries. Pulse Adult (60-100) bpm Child (80-120) bpm Infant ( 140 bpm) Palpated on superficial arteries (pulse points) Auscultated on Apex of the heart Pulse Variations: Tachycardia - >100 bpm Bradycardia - < 60 bpm Palpitations - Unpleasant sensations of awareness of the heartbeat: described as skipped beats, racing, fluttering, pounding or irregularity: may result from rapid acceleration or slowing of heart, increased forcefulness of cardiac contraction: not necessarily associated with heart disease. Factors Assessing Pulse • • • • • • • Cardiac output Age Gender Exercise Fever Stress Position Factors Assessing Pulse Cardiac Output Amount of blood ejected from the heart in one minute Measured by SV x HR Normal HR = 60 - 100 beats per minute Factors Assessing Pulse Age Adult (60-100) bpm Child (80-120) bpm Infant ( 140 bpm) Gender - after puberty female > male Exercise increased HR with activity increased metabolism causes vasodilatation causes O2 demand Factors Assessing Pulse Fever body compensates for increased temp by vasodilatation, decreased BP causes body to compensate by > HR increased 10-20 beats/min/ degree above norm especially in children Factors Assessing Pulse Stress sympathetic response, increases HR & BP Position sitting, standing causes pooling results in transient - BP rate compensates by increasing Assessing : Pulse • • • Please note: Assessing a heart rate is determining beats per minute, noting rate, rhythm and strength. Assessing peripheral pulses is to assess arterial blood flow to peripheral arteries. Assessment: Pulse Auscultating at Apex Using the diaphragm of your stethoscope, place it on the 5th intercostal space, MCL For one full minute, count each LUB, DUB as one!! Location of left ventricular apex & PMI (point of maximum impulse) Adult: 5th ICS, MCL Infants: 4th ICS, left of MCL Pregancy: PMI moves 1-2 cm left of MCL & up to 4th ICS Assessment:Pulses Peripheral Pulses Obtain History Intermittent claudication pain on walking disappears with rest leg cramps, leg ulcers varicose veins edema of feet or legs blood clots pallor of fingertips Assessment:Pulses Peripheral Pulses Inspection of Extremities Compare Left to Right Size Symmetry Skin/color Nail Beds Nails Hair Growth Assessment:Pulses Peripheral Pulses Palpation - Compare Right to Left Temperature Capillary refill Pulses UE:Radial,Brachial LE: Dorsalis Pedis, Posterior tibial, popliteal, Femoral Edema +1- +4 pitting Sensation Assessment: Pulses Characteristics of Pulses Rate Rhythm - regular, irregular Contour/elasticity Strength (Amplitude) +4 = bounding +3 = full, increased +2 = normal +1 = diminished, weak 0 = absent Arterial Insufficiency of Lower Extremities Pulses - Decreased/Absent Color - Pale on elevation : Dusky Rubor on dependency Temperature - Cool/Cold Edema - None Skin - Shiny, thick nails, no hair, Ulcers on Toes Sensation - Pain, more with exercise, Paresthesias Venous Insufficiency of Lower Extremities Pulses - Present Color- Pink to cyanotic, Brown pigment at ankles Temperature - Warm Edema - Present Skin - Discolored, scaly, ulcers on ankles Sensation - Pain, More with standing or sitting. Relieved with elevation/support hose Peripheral Vascular Disease Nursing interventions to promote venous return ankle circles, flex ankles, frequent ambulation, avoid dependent position for prolonged periods of time apply TED stockings or ace bandages (if no arterial problem) Nursing Diagnosis Altered cardiac output: decreased Altered tissue perfusion:peripheral Fluid volume deficit: actual Irregular Rhythm ALL irregular rhythms demand an APICAL RADIAL assessment Assessment: Blood Pressure • Obtain History: Obtain History: ** Non-modifiable Risk factors ** ** Modifiable Risk factors** Age, sex, personality type SmokingEmployment: physical vs Family History – sudden emotional demands, environmental hazard, death, HTN, stroke, MI prior stress managementNutritional Status: to 50, severe hyperlipidemis, body fat & type of dietAnaerobic DM exerciseEstrogen replacement (if postmenopausal)Drug use – alcohol,, cocaine, PMH – arrythmias, murmurs, prescription & OTCEssential CHF, Rheumatic disease HTNHypercholesterolemia, DM, DM, CAD,Congenital CAD Heart Defects Taking a Blood Pressure Blood Pressure: Key Facts • Korotkoff sounds: Turbulent sounds of partial obstruction of arterial flow Phase I: sharp tapping sound (systolic) Phase II: change to soft swishing sound Phase III: sounds more crisp & intense Phase IV: muffled tapping Phase V: cessastion of sound (diastolic) Blood Pressure: Key Facts Arm Blood Pressure: May be 5-10 mmHg higher in right arm than left arm: greater differences between right & left arm may be associated with congenital aortic stenosis or acquired conditions such as aortic dissection or obstruction of arteries to upper arm. Leg Blood Pressure: Arm & leg blood pressures are about equal during first year of life & after that time the leg blood pressure is 15-20 mmHg higher than the arm BP. Pulse Pressure: difference between systolic and diastolic blood pressures: Usual pulse pressure is between 30-40 mmHg Orhtostatic Hypotension: Decrease in SBP of 20-30 mmHg or more when changing from supine to standing position, & increase in pulse of 1020 bpm: sudden drops may result in fainting. Dizziness & faintness from orthostatic hypotension may occur when taking anti-hypertensive medications, hypovolemia, confined to bed for prolonged periods of time, or the elderly.