* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Chest Pain
Electrocardiography wikipedia , lookup
Saturated fat and cardiovascular disease wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Aortic stenosis wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
History of invasive and interventional cardiology wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
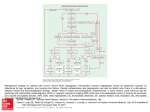
Chest Pain Dr. Mohannad F Allehyani Emergency Medicine Demonstrator KAUH – Faculty of Medicine Goals Review the pathophysiology, diagnosis and treatment of life threatening causes of chest pain. Epidemiology 5% of all ED visits Approximately 5 million visits per year Visceral Pain Visceral fibers enter the spinal cord at several levels leading to poorly localized, poorly characterized pain. (discomfort, heaviness, dull, aching) Heart, blood vessels, esophagus and visceral pleura are innervated by visceral fibers Parietal Pain Parietal pain, in contrast to visceral pain, is described as sharp and can be localized to the dermatome superficial to the site of the painful stimulus. Initial Approach ABC’s first, always (look for conditions requiring immediate intervention) Aspirin for potential ACS EKG Cardiac and vital sign monitoring History O- onset P-provocation /palliation Q- quality/quantity R- region/radiation S- severity/scale History Change in pain pattern Associated symptoms: DOE, SOB, diaphoresis, vomiting, heart burn, food intolerance PHx Social history FHx Physical Exam General Appearance and Vitals (sick vs not sick) Chest exam -Inspection (scars, heaves, tachypnea, work of breathing) -Auscultation (murmurs, rubs, gallops, breath sounds) -Percussion (dullness) Physical Exam Neck: JVD, crepitence, bruits Abdomen Extremities: swelling, pulses, tenderness, Homan’s Differential Diagnoses Cardiovascular Acute myocardial infarction, Acute coronary ischemia, Aortic dissection, Cardiac tamponade, Unstable angina, Coronary spasm, Prinzmetal's angina, Cocaine induced, Pericarditis, Myocarditis, Valvular heart disease, Aortic stenosis, Mitral valve prolapse, Hypertrophic cardiomyopathy Pulmonary Pulmonary embolus, Tension pneumothorax, Pneumothorax, Mediastinitis, Pneumonia, Pleuritis, Tumor, Pneumomediastinum Gastrointestinal Esophageal rupture (Boerhaave), Esophageal tear (MalloryWeiss), Cholecystitis, Pancreatitis, Esophageal spasm, Esophageal reflux, Peptic ulcer, Biliary colic Musculoskeletal Muscle strain, Rib fracture, Arthritis, Tumor, Costochondritis, Nonspecific chest wall pain Neurologic Spinal root compression, Thoracic outlet, Herpes zoster, Postherpetic neuralgia Other Psychologic, Hyperventilation Life Threatening Causes of Chest Pain Acute Coronary Syndromes Pulmonary Embolus Tension Pneumothorax Aortic Dissection Acute Coronary Syndromes Epidemiology In a typical ED population of adults over the age of 30 presenting with visceral-type chest pain, about 15 percent will have AMI and 25 to 30 percent will have UA Acute Coronary Syndromes - History “Typical” Chest Pain Story (Pressure-like, squeezing, crushing pain, worse with exertion, SOB, diaphoresis, radiates to arm or jaw) The majority of patients with ACS DO Acute Coronary Syndromes – EKG Findings STEMI - ST segment elevation (>1 mm) in contiguous leads; new LBBB T wave inversion or ST segment depression in contiguous leads suggests subendocardial Acute Coronary Syndromes – Cardiac Markers Marker Initial Rise Peak Return to normal Troponin 2-4 hr 10 -24 hr 5 -10 days CK-MB 3-4 hr 10-24 hr LDH 10 hr 24 -72 hr 14 days Myoglobin 1-2 hr 4 -8 hr 2 – 4 days 24 hours Benefits Sensitive and specific Unaffected by renal failure Very sensitive, powerful negative predictive value Acute Coronary Syndromes – Cardiac Markers Echocardiogram Wall abnormalities occur within minutes Will detect abnormalities in 80% of AMI Normal resting echo in setting of chest pain gives low probability Early screen for AMI Echo Acute Coronary Syndromes Treatment Aspirin Nitroglycerin Oxygen Analgesia Treatment Beta-Blockers Anticoagulation Anti-Platelet Agents Thrombolysis Percutaneous Coronary Interventions (PCI) Stress echocardiograms Sensitivity 60-90% Specificity 75% ? Should be employed with moderate to high risk stratification Limitations of reader, image quality, and previous functional Acute Coronary Syndromes Treatment STEMI (ASA, B-blocker, NTG, anti-platelet, anticoagulation, thrombolysis, PCI) NSTEMI (ASA, B-blocker, NTG, Acute Coronary Syndromes Disposition Mortality is twice as high for missed MI Missed MI is the most successfully litigated claim against EP's. EP’s miss 3-5% Acute Coronary Syndromes Disposition A single set of cardiac enzymes is rarely of use Risk Stratification: goal is to predict the likelihood of an adverse cardiovascular event Combination of H+P, EKG, Pulmonary Embolism Pathophysiology Thrombosis of a pulmonary artery >90% arise from DVT Clot from a DVT travels through the venous system and lodges in the pulmonary vasculature Pulmonary Embolism – History Dyspnea is the most common symptom, present in 90% of patients diagnosed with PE Sharp pleuritic chest pain, syncope, Prolonged immobilization, Pulmonary Embolism – Physical Exam Tachycardia, tachypnea, diaphoresis, hypotension, hypoxia, low grade fever, anxiety, cardiovascular collapse, right ventricular heave Pulmonary Embolism – Diagnostic Testing Sinus Tachycardia is the most frequent EKG finding Classic S1,Q3,T3 finding is seen in less than 20% ABG plays no role in ruling out Pulmonary Embolism – Wells Criteria Clinical Signs and Symptoms of DVT? Yes +3 PE is #1 Diagnosis, or Equally Likely? Yes +3 Heart Rate > 100? Yes +1.5 Immobilization at least 3 days, or Surgery in the Previous 4 weeks? Yes +1.5 Previous, objectively diagnosed PE or DVT? Yes +1.5 Hemoptysis? Yes +1 Malignancy w/ Treatment within 6 mo, or Pulmonary Embolism – Diagnostic Imaging Algorithm Pulmonary Embolism – Treatment/Disposition Unfractionated heparin vs low molecular weight heparin (some studies suggest superiority of LMWH) Thrombolysis (for cardiovascular collapse) PE CXR Aortic Dissection Pathophysiology Intimal tear of the aorta leads to dissection of the layers of the aorta creating a false lumen Aortic Dissection - Diagnosis Tearing chest pain radiating to the back Risk Factors: HTN, connective tissue disease Exam: HTN, pulse differentials, neuro deficits Aortic Dissection - Classification De Bakey system: Type I dissection involves both the ascending and descending thoracic aorta. Type II dissection is confined to the ascending aorta. Type III dissection is confined to the descending aorta. The Daily system classifies dissections Aortic Dissection - Treatment Patients with uncomplicated aortic dissections confined to the descending thoracic aorta (Daily type B or De Bakey type III) are best treated with medical therapy. Medical Therapy: Goal to decrease the blood pressure and the velocity of left ventricular contraction, both of which will decrease aortic shear stress and minimize the tendency to further dissection. Acute ascending aortic dissections (Daily type A or Tension Pneumothorax Pathophysiology Collection of air in the pleural space causes collapse of the ipsilateral lung and then cardiovascular collapse as Tension Pneumothorax Diagnosis Risk factors: COPD; connective tissue disease, trauma, recent instrumentation, positive pressure ventilation Tension Pneumothorax Treatment Needle decompression Tube thoracostomy Esophageal Rupture Pathophysiology Tear in the esophagus leads to leaking of gastrointestinal contents into the mediastinum Inflammation followed by Esophageal Rupture Diagnosis Rare but devastating Risk Factors: Iatrogenic, heavy retching, trauma, foreign bodies, toxic ingestion Not so subtle Subtle Imaging Esophageal Rupture Treatment Antibiotics Supportive Care Small tears with minimal extraesophageal involvement can Take Home Points ABC’s first History is key Have a low threshold for missed MI