* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download No Slide Title
Heart failure wikipedia , lookup
Electrocardiography wikipedia , lookup
Coronary artery disease wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Myocardial infarction wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
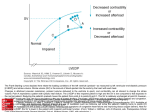
Functional Hemodynamic Indicators Arterial Pressure Waveform Technology Donna Adkisson, RN, MSN Anatomy & Physiology Review Blood Flow in the Heart From the body Right side of the Heart To the lungs for Oxygenation Air in via trachea Bronchus Bronchioles Alveoli Capillaries Oxygen in Carbon Dioxide out Left side of the Heart Out the aorta www.lidco.com Anatomy & Physiology Review Anatomy & Physiology Review Cardiac Cycle Diastole – relaxation or filling Preload coming into right side of the heart 70% of blood flows into the ventricles passively Other 30% from atrial kick Systole – contraction or pumping Atrial Systole = Ventricular Diastole 30% of blood flows into the ventricles from the atrial contraction Ventricular Systole www.lidco.com How well can the heart pump – Ejection or Stroke Volume What is the heart pumping against - SVR Cardiac Output CO = SV x HR Cardiac output is the volume of blood pumped by the heart per minute. For an average size of adult (70 kg) at rest this would be about 5 liters/min. During severe exercise it can increase to over 30 liters/min. Cardiac output is frequently necessary to assess the state of a patient's circulation. The simplest measurements, such as heart rate and blood pressure, may be adequate for many patients, but if there is a cardiovascular abnormality then more detailed measurements are needed. www.lidco.com Hemodynamic Monitoring Hemodynamic Monitoring is an important aspect of patient care in: Operating Rooms Critical Care Units Hemodynamic Monitoring ranges from: Non-Invasive EKG www.lidco.com NIBP Invasive Arterial Line LiDCO CVP PA catheter Functional Hemodynamic Monitoring Transpulmonary Thermodilution (TPTD) – Based on the Stewart-Hamilton equation LiDCOplus Pulse Power analysis to derive Stroke Volume Calibrated with Bolus dilution of lithium PiCCO Pulse contour analysis Temperature change sensed by thermistor-tipped arterial catheter www.lidco.com Functional Hemodynamic Monitoring Non-Calibrated LiDCOrapid Pulse Power analysis to derive Stroke Volume Same algorithm as the LiDCOplus FloTrac Proprietary sensor attached to arterial line Algorithm applied to analysis has been changed www.lidco.com Hemodynamic Monitoring including: Cardiac Output Cardiac Index SVR Stroke Volume Blood Pressure DO2 Oxygen Consumption Preload Indicators www.lidco.com Cardiac Output Ways to clinically determine Cardiac Output: Dilution method Thermodilution Green Dye Lithium Dilution Arterial Wave Form Analysis Blood sample to calculate the Fick equation Continuous Cardiac Output TEE/EsopheagealDoppler www.lidco.com Continuous Cardiac Output? Sampling to get a 3 to 5 minute average PA catheter Beat to Beat Continuous Arterial wave form analysis www.lidco.com Beat-to-Beat Continuous Cardiac Output Pulse Power waveform analysis continuously assesses the patient's hemodynamic status by analyzing and processing the arterial pressure signal obtained from the primary blood pressure monitor. • 0 www.lidco.com CO = SV x HR Stroke Volume The volume of blood per stroke of the heart Effected by: Amount of Blood coming into the heart – Preload How well the heart works – Contractility How much pressure or resistance the heart has to work against – Afterload www.lidco.com CO = SV x HR Stroke Volume SV = Preload + Afterload + Contractility Preload – volume Afterload – resistance (SVR) Contractility – Muscle compliance (EF) www.lidco.com Ventricular Preload and Fluid Responsiveness Fluid Resuscitation primary treatment of many shock states Fluid Resuscitation is not without risk Less than 50% of patients respond to a fluid bolus. The heart performs more efficiently when appropriately filled. The term preload refers to maximum stretch on the heart's muscle fibers at the end of diastolic filling. The degree of stretch is determined by the volume of blood contained in the ventricle at that time. www.lidco.com Ventricular Preload and Fluid Responsiveness Commonly used static preload measurement are not sensitive or specific predictors of a patient's ability to respond to fluid bolus CVP PAOP Functional Hemodynamic Indices are more sensitive and specific predictors of fluid responsiveness Reflect the effect of positive pressure ventilation on preload and SV Pulse Pressure Variation Stroke Volume Variation Systolic Pressure Variation www.lidco.com Functional Hemodynamics Bridges, Elizabeth J. Arterial Pressure – Based Stroke Volume and Functional Hemodynamic Monitoring. Journal of Cardiovascular Nursing, March/April 2008;23(2): pp 105-112 www.lidco.com Preload Systolic and Pulse pressure variation can be measured intermittently from the arterial line via the beside monitor continuously using PPV, SVV or SPV LiDCO system – plus or rapid FloTrac SVV www.lidco.com Preload Indicators Systolic pressure variation (SPV) may reflect variations in pleural pressure and changing LVSV. PPV reflects only changes in transmural aortic pressure and therefore changes in LVSV on a beat-to-beat basis. Michard et al (1999) found PPV gave a more accurate measure of cardiac index when compared to SPV, which it turn was a better measure than CVP and PAW. PPV was superior to SPV in predicting preload responsiveness proving to have better precision with less variance. Note: SPV and PPV do not require the patient to be in apnoea. In fact they depend on positive pressure breathing. www.lidco.com Best Preload Responsiveness - PPV Michard F., Boussat S, Chemla D, et al. Relation between respiratory changes in arterial pulse pressure and fluid responsiveness in septic patients with acute circulatory failure. American Journal of Respiratory and Critical Care Medicine. Jul 2000;162(1):134-138 www.lidco.com Hemodynamic Monitoring Arterial Waveform Analysis Preload indicator - looks at the variation from inspiration to expiration of the patient PPV - Pulse Pressure Variation » Greater than 10 to 13% patient preload responsive SVV - Stroke Volume Variation » Greater than 10 to 13% patient preload responsive SPV - Systolic Pressure Variation » Greater than 5mmHg patient preload responsive www.lidco.com Frank Starling’s Law The greater the ventricle is filled during diastole, the more the muscle fibres are stretched, the greater is the force of contraction. This is true to a defined point of stretch above which point contraction force will not increase further. www.lidco.com Frank Starling Curve Frank-Sartling's Curve 90 Patient A is preload responsive Patient B 80 SV SV Stroke Volume 70 On steep part of curve Set preload results in Significant increase in SV Preload 60 50 Patient B is not preload responsive 40 Patient A 30 SV An equal preloading does not result in a great increase in SV This patient does not require fluid resuscitation 20 10 Preload 0 1 3 5 7 9 11 Preload www.lidco.com 13 15 17 19 Case Studies Pulse Pressure Variation of 65% After ½ liter of volume down to 24% After another ½ liter of volume down to 10% Pulse Pressure Variation of 124% Patient on Epinephrine & Levophed drips 2 units of Albumin given Within 24 hours, patient off all drips Extubated Pulse Pressure Variation of 38%, CO 2.8, EF 15% Pulmonary Edema & Peripheral Edema 500cc IV fluid, Lasix (times 4) 8 hours later: PPV 16%, CO 3.9 no increase in Pulmonary or Peripheral Edema www.lidco.com Afterload Systemic Vascular Resistance The amount of pressure the heart must work against Decreases as CO & CI increases Can be controlled with medications Vasoconstrictor – Increases SVR & BP Vasodialators – Decreases SVR & BP www.lidco.com Drugs used to Effect SVR Vasoactive Drugs – can be a vasoconstrictor or vasodialators Vasoconstrictors – increase SVR (afterload) and blood pressure, but vary in their effect on cardiac output. The pure a agonists leave the output of the normal heart unchanged, but may significantly reduce it in the failing heart. As the beta activity of the vasoconstrictor is increased, so cardiac output also tends to increase Vasodilators – Used to dilate arteries, Decrease SVR, Decrease BP www.lidco.com Vasoactive Drugs Vasoactive Drugs: vasoconstructors Isoproteranol – most widely used to ease breathing problems in asthma and COPD and to control irregular heartbeat until a pacemaker can be implanted. Phenylephrine – Neo-Synephrine: used to treat shock and low blood pressure. Ephedrine – used to counteract the hypotensive effects of anesthesia. Also useful as a pressor agent in hypotensive states following sympathectomy, or following overdosage drugs used for lowering blood pressure in the treatment of arterial hypertension. Metaraminol – Aramine: used to raise the blood pressure and stimulate the heart in treating patients with shock. Milrinone – Primacor : short-term treatment of patients with acute decompensated heart failure. Vasopressin – an alternative to noradrenaline in the treatment of hypotension effective in combating milrinone-induced hypotension. www.lidco.com Drugs used to Effect SVR Vasodilators - Used to dilate arteries, Decrease SVR, Decrease BP Sodium Nitroprusside is the most potent of the 'mixed' vasodilators. Reliably reduces both afterload and preload. Nitroglycerine acts predominantly on the venous side of the circulation to reduce preload. The reduction in preload is accompanied by a decrease in LV wall tension with a secondary reduction in myocardial oxygen, also a specific coronary arterial vasodilator and spasmolytic. Adenosine can be used for its vasodilatory effects. Because of its short plasma half life (< 5 seconds), the drug has a particular role as a relatively specific pulmonary vasodilator. Hydralazine acts exclusively on the arterial side of the circulation to reduce afterload. www.lidco.com Contractility Muscle Compliance (EF) The ability of the muscle fiber to stretch and contract Medications that can assist with contractility Epinephrine Dobutamine www.lidco.com Contractility Contractility Myocardial Contractility Is the power of contraction Is independent of preload or afterload At a constant preload positive inotropic agents > contractility > SV www.lidco.com Drugs used to Effect Cardiac Output Vasoactive Drugs – can be a vasoconstrictor or iontrope Vasoconstrictors: increase SVR (afterload) and blood pressure, but vary in their effect on cardiac output. The pure a agonists leave the output of the normal heart unchanged, but may significantly reduce it in the failing heart. As the beta activity of the vasoconstrictor is increased, so cardiac output also tends to increase Inotrope: is an agent that alters the force or energy of muscular contractions www.lidco.com Positive Inotropic Agents Inotrope: is an agent that alters the force or energy of muscular contractions Adrenaline – Epinephrine (Epi or Adrenalin): used to treat shock, as a heart stimulant. Noradrenaline – Norepinephrine (Levophed): used to increase the output of the heart and raise blood pressure as part of the treatment of shock. Dopamine – used for the correction of hemodynamic imbalances present in the shock syndrome due to myocardial infarctions, trauma, endotoxic septicemia, open heart surgery, renal failure, and chronic cardiac decompensation as in congestive failure. Dobutamine – Dobutrex and generic forms: used to stimulate the heart during surgery or after a heart attack or cardiac arrest. www.lidco.com CO = SV x HR Heart Rate HR < 60 beats per minute HR > 100 beats per minute Bradycardia – pacemaker, Atropine, Epinephrine Tachycardia – Cardioversion, Digoxin, Treat fever or shock causing ↑ HR www.lidco.com Cardiac Output Changes Cardiac Output Decreases Decrease in blood volume Increase in PPV or SVV Decrease in ejection fraction Decrease in SV Decrease in Heart Rate Bradycardia www.lidco.com Cardiac Output Increases Vasodilation Decrease in SVR Increase in Contractility Increase SV Increase in Heart Rate Tachycardiac Decision Table Does my patient need an increase in SV or CO? ↓Yes Is the arterial trace accurate? ↓Yes Is the patient fully ventilated? ↓Yes Is the tidal volume > 8ml/kg ↓Yes Is the cardiac rhythm regular ↓Yes What is the PPV or SVV < 10% → No fluid www.lidco.com > 10 to 13% → Give fluid Fluid replacement therapy Non responder Responder Stroke volume increases < 10% Stroke volume increases > 10% 100 - 200 ml fluid challenge www.lidco.com The Old Way is Not Good Enough Hemodynamic monitoring has traditionally involved the placement of a pulmonary artery catheter Minimally invasive Cardiac Output Monitoring eliminates the complications of the pulmonary artery catheter Which includes: Complications Related to Catheter Vascular Complications www.lidco.com Complications Related to Pulmonary Artery Catheters Tachyarrhytmias Right bundle branch block ( 0.05-5% ) Complete heart block ( with preexisting left bundle branch block ) Cardiac perfuration Thrombosis and embolism Pulmonary infarction due to persistent wedging ( 0-1.4% ) Catheter-related sepsis PA rupture ( 0.2% chance ) Knotting of the catheter Endocarditis, bland and infective Pulmonic valve insufficiency Balloon fragmentation and embolization www.lidco.com Vascular Complications Related to Pulmonary Artery Catheters Accidental arterial puncture Pneumothorax Braquial plexus lesion Horner syndrome Phrenic nerve lesion Gaseous embolism Hemorrhage Infections www.lidco.com Cost Related to Line Infections Cost for Prolonged Bloodstream Infections can top $50,000 7 to 21 extra hospital days for Bloodstream Infections New Medicare Regulations Hospitals will no longer receive higher payments for the additional costs associated with treating patients for hospital-acquired infections Payments will be withheld from hospitals for care associated with treating vascular catheterassociated infections. www.lidco.com New rules go into effect October 2008 Cost Related to Line Infections CDC reports that there are 248,678 cases of central line associated bloodstream infections every year. Institute for Healthcare Improvement estimates that approximately 14,000 people die every year from central line-related bloodstream infections. www.lidco.com