* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Tachyarrhythmias, Diagnosis and Management
Survey
Document related concepts
Coronary artery disease wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Electrocardiography wikipedia , lookup
Ventricular fibrillation wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Transcript
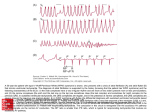
Tachyarrhythmias, Diagnosis and Management Laurent Lewkowiez, MD Assistant Professor Denver Health and Hospitals University of Colorado Health Sciences Mechanisms of Arrhythmia • Abnormal automaticity – automatic impulse generation from unusual site or overtakes sinus node • Triggered activity – secondary depolarization during or after repolarization – Dig toxicity, Torsades de Pointes • Reentry – 90 % of arrhythmias Reentry • Most common mechanism • Requires two separate paths of conduction • Requires an area of slow conduction • Requires unidirectional block Supraventricular Tachycardias Diagnosis • ECG is cornerstone • Observe zones of transition for clues as to mechanism: – – – – onset termination slowing, AV nodal block bundle branch block Regular SVT in adults • 90% reentrant 10 % not reentrant • 60% AV nodal reentrant tachycardia (AVNRT) • 30% orthodromic reciprocating tachycardia (ORT) • 10% Atrial tachycardia • 2 to 5% involve WPW syndrome Differential Dx of Regular SVT • Short RP tachycardia – AV nodal reentrant tachycardia – ORT( Orthodromic reciprocating tachycardia) – atrial tachycardia when associated with slow AV nodal conduction Short RP interval AV Nodal Reentrant Tachycardia Slow pathway • 2 pathways within or limited to perinodal tissue – anterograde conduction down fast pathway blocks with conduction down slow pathway, with retrograde conduction up fast pathway. • May have very short RP interval with retrograde P wave visible as an R’ in lead V1 or psuedo-S wave in inferior leads in 1/3 of cases . No p wave seen in 2/3 Fast pathway AV Nodal Reentrant Tachycardia • Responds to vagal maneuvers in 1/3 cases • Very responsive to AV nodal blocking agents such as beta blockers, CA channel blockers, adenosine. • Recurrences are the norm on medical therapy • Catheter ablation 95% successful with 1% major complication rate Ablation AVNRT His bundle Ablation area Orthodromic Reciprocating Tachycardia • Anterograde over AV node and retrograde conduction of an accessory pathway. • RP interval short but longer than AVNRT due to required conduction through ventricle prior to conduction up accessory pathway • Frequently presents in patients with WPW patients as narrow complex tachycardia Conduction down AVnode Up accessory pathway ORT • Amenable to AV nodal blocking agents in absence of WPW syndrome (anterograde conduction of pathway) • Amenable to catheter ablation with 95% success and 1% rate major complication Conduction down AVnode Up accessory pathway Differential Dx of Regular SVT • Long RP tachycardia – – – – Atrial tachycardia Sinus node reentry Sinus tachycardia Atypical AV nodal reentrant tachycardia – Permanent form of junctional reciprocating tachycardia Long RP interval Atrial Tachycardia • Atrial rate between 150 and 250 bpm • Does not require AV nodal or infranodal conduction • P wave morphology different than sinus • P-R interval > 120 msec differentiating from junctional tachycardia • Origin inferred from P wave morphology. Atrial tachycardia • P wave upright lead V1 and negative in aVL consistent with left atrial focus. • P wave negative in V1 and upright in aVL consistent with right atrial focus. • Adenosine may help with diagnosis if AV block occurs and continued arrhythmia likely atrial tachycardia • 70-80% will also terminate with adenosine. Atrial Tachycardia • Most are due to abnormal automaticity and have right atrial focus • May be reentry particularly in patients with previous atriotomy scar, such as CABG or congenital repair patients Atrial Tachycardia Therapy • Frequently treated with antiarrhythmics – Class 1 agents procainamide, quinidine, flecainide may be used in patients without structural heart disease. – Class III agents sotalol, amiodarone, dofetilide may be used with caution according to specific side effects • AV Nodal blocking agents for rate control. • Catheter ablation effective in 70-80% Other Long RP tachycardias • Sinus node reentrant – abrupt onset and offset – P wave complex same as sinus – Amenable to calcium channel blockers, much less responsive to beta blockers – Amenable to catheter ablation • Syndrome of inappropriate sinus tachycardia – typical sinus tachycardia with lowest rate on Holter of 130 bpm – Treated with high dose beta blockers – Poor results with catheter ablation Atrial Flutter • Rate 250 to 350 bpm • Rotates counter-clockwise around right atrium using a protected isthmus • Negative saw-tooth pattern leads II , III, AVF and positive in lead V1 • Treatment similar to atrial tachycardia but rate control more difficult Atrial Flutter Atrial Flutter and Risk of Stroke • Although risk of stroke historically has been thought to be low, multiple instances of stroke with cardioversion lead to similar indication for anticoagulation as atrial fibrillation. A 32 year old female is treated in the emergency room for palpitations. The first ECG is tachycardia and the second is after adensosine.What is the arrhythmia? • • • • A. B. C. D. AVNRT ORT Atrial tachycardia Atrial fibrillation Answer: AVNRT (A) • A small R’ is seen is lead V1 with pseudo-S waves in the inferior leads that are absent after termination of the arrhythmia. These represent retrograde atrial activation with a very short RP interval. WPW syndrome • Accelerated AV conduction PR <120 msec • Prolonged QRS > 120 msec • Abnormal slurred upstroke of QRS ( delta wave) • Abnormal depolarization and repolarization may lead to pseudoinfarction pattern WPW pathophysiology • Short AV conduction – early excitation of ventricle at site of accessory pathway The result is fusion of both normal and accessory conduction No conduction • Bizarre upstroke of QRS delay – abnormal initial site of depolarization • Wide QRS – early initiation of ventricular depolarization AV node Accessory pathway WPW epidemiology • Present in 0.3% of the population • Risk of sudden death 1 per 1000 patient-years • Sudden death due to atrial fibrillation with rapid ventricular conduction • Atrial fibrillation often induced from rapid ORT ORT(orthodromic reciprocating tachycardia Atrial Fibrillation and WPW • AV nodal blocking agents may paradoxically increase conduction over accessory pathway by removing concealed retrograde penetration into accessory pathway. Concealed penetration into the pathway causes intermittent block of pathway conduction Management of Atrial Fibrillation with WPW • Avoid AV nodal blockers • IV procainamide to slow accessory pathway conduction • Amiodarone if decreased LVEF • DC cardioversion if symptomatic with hypotension Management of Patients with WPW • All patients with symptomatic AF & WPW should be evaluated with EPS • Accessory pathways capable of conducting faster than 240 BPM should be ablated • Patients with inducible arrhythmias involving pathway should be ablated • WPW patients in high risk professions should be ablated. A 42 year old smoker presents to the ED with palpitations. His blood pressure is 100/60. The following rhythm strip is obtained . What is the next appropriate step? • A. Emergent cardioversion for polymorphic VT. • B. I.V. procainamide • C. I.V. lidocaine • D. diltiazem drip to obtain rate control. Answer B • This patient has WPW with atrial fibrillation and a rapid ventricular response. He is stable, thus I.V. procainamide is indicated to slow conduction down the accessory pathway. Diltiazem is contraindicated. Lidocaine will have no effect, as this is not VT . Atrial Fibrillation Epidemiology • Affects 2 to 4% of population • Increases to 5 to 10 % of patients over 80 • Associated with 2-fold increased risk of death • Risk of thromboembolism is approximately 5% per year but may be as high as 20% in high risk groups not anticoagulated Mechanism of Atrial Fibrillation • Multiple reentrant wavelets moving between right and left atrium • May be initiated by rapidly firing automatic foci found commonly in pulmonary veins, SVC, and coronary sinus. • Factors that shorten atrial refractoriness and slow conduction velocity perpetuate atrial fibrillation • Factors that lengthen atrial refractoriness (antiarrhythmic drugs ) aid in termination Management of Atrial Fibrillation • Aimed at symptom relief by rate and rhythm control • Aimed at reducing risk of thromboembolism by anticoagulation • Preventing tachycardia mediated cardiomyopathy (a progressive, reversible rate-induced form of LV dysfunction) Acute Management of Atrial Fibrillation • Focuses on Rate control • Patient with atrial fibrillation may undergo DC cardioversion or pharmacologic conversion if less than 48 hours duration or following TEE on Heparin without evidence of left atrial thrombus. Stroke rate .8% • Following cardioversion the patient should be kept anticoagulated for 4 weeks with goal INR of 2 to 3 until atrial function normalizes. Acute Management of Atrial Fibrillation • 50% of patients with paroxysmal atrial fibrillation will spontaneously convert within 24 hours • Digoxin used heavily in the past for prevention and conversion of atrial fibrillation is ineffective at either and may be profibrillatory as it decreases the atrial refractory period Acute Management of Atrial Fibrillation • Rate control may be attained with calcium channel blockers or beta blockers in patients with normal L.V. function. • Calcium channel blockers may be used cautiously in patients with depressed LV function but are associated with increased mortality in the long term. • Beta blockers should be avoided in acutely decompensated CHF patients with atrial fibrillation Atrial Fibrillation and Depressed L.V. Function • Digoxin and amiodarone may be of effective in patients with LV dysfunction and decompensated congestive heart failure to slow ventricular response. • Digoxin alone is rarely effective when the patient is sympathetically driven • Avoid high dose digoxin with amiodarone as digoxin levels increase 2-fold with amiodarone Chronic Management of Atrial Fibrillation • Patients with atrial fibrillation, paroxysmal or sustained should be anticoagulated if any of the following risk factors for stroke are present: – – – – diabetes valvular disease hyperthyroidism Prior CVA – hypertension – congestive heart failure – age greater than 65 Chronic Management of Atrial Fibrillation • Rate control with calcium channel blockers, beta blockers or combination with digoxin. • Digoxin may be used in bed bound patients but is easily overcome with sympathetic stimulation. • Maintenance of sinus is similar with class I and class III drugs approaching 50% recurrence at 1 year • Recurrence of atrial fibrillation 80% at 1 year without treatment Chronic management of Atrial Fibrillation • Class III agents may have improved efficacy – Amiodarone • pulmonary toxicity • thyroid • liver – Dofetilide • Torsades des Pointes – Safe in CHF and CAD – Limited due to side effect profile • Class IC agents safe in absence of structural heart disease. • Few side effects • Need stress testing • Can lead to 1 to 1 ventricular conduction of atrial flutter • Use with beta blocker Chronic Management of Atrial Fibrillation • Recent large trials reveal no benefit of rhythm control over rate control. • Trend of increased mortality in rhythm arm likely due to proarrhythmia from drugs. • Patients unable to tolerate atrial fibrillation due to symptoms were not enrolled in these studies and are increasingly undergoing ablation , catheter and surgical procedures. Nonpharmacologic Treatment of Atrial Fibrillation • Maze Procedure – 90% freedom from atrial fibrillation – 2% mortality required thoracotomy • Catheter ablation procedure – only moderate success – long procedures, difficult – selecting population – 60% to 80% effective – Pulmonary vein stenosis,cva,perforation, – esophageal fistula Nonpharmacologic Treatment of Atrial Fibrillation • AV node ablation with pacemaker implant – – – – recently shown to have no effect on mortality effective at reducing symptoms Does not alter need for anticoagulation Pace at 90 BPM 1 month after procedure to avoid Torsades des Pointes Wide ComplexTachycardias • Ventricular Tachycardia • SVT with aberrancy (functional bundle branch block) • SVT with underlying bundle branch block • SVT with pre-excitation Additional Mimimics of Wide Complex Tachycardias • SVT with severe hyperkalemia • SVT with use of antiarrhythmic agents particularly 1C agents • SVT with acute MI Wide-Complex Tachycardia • Majority are sinus tachycardia with bundle branch block • In higher risk population , previous MI, Decreased Left ventricular dysfunction – Predominantly Ventricular Tachycardia Differentiating Ventricular Tachycardia from SVT with Aberrancy • Leads to correct initial therapy • Avoids use of Verapamil which may precipitate hemodynamic collapse with V.T. • Cannot use rate or the presence or absence of symptoms as discriminator ! • Use ECG criteria for diagnosis • Use presence of risk factors for V.T. as discriminator The Brugada Criteria Table I. Diagnosis Of Wide QRS Complex Tachycardia With A Regular Rhythm Step 1. Is there absence of an RS complex in all precordial leads V1 – V6? If yes, then the rhythm is VT. Sens 0.21 Spec 1.0 Step 2. Is the interval from the onset of the R wave to the nadir of the S wave greater than 100 msec in any precordial leads? If yes, then the rhythm is VT. Sens 0.66 Spec 0.98 Step 3. Is there AV dissociation? If yes, then the rhythm is VT. Sens 0.82 Spec 0.98 Step 4. Are morphology criteria for VT present? See Table II. If yes, then the rhythm is VT. Sens 0.99 Spec 0.97 Morphology Criteria for VT Table II. Morphology Criteria for VT Right bundle type requires waveform from both V1 and V6. V1 V6 Monophasic R wave QR or QS RS or QR R/S <1 Left bundle type requires any of the below morphologies. V1or V2 V6 R wave > 30 msec QR or QS Notched downstroke S wave. Greater than 60msec nadir S wave. Adapted from Brugada et al. A new approach to the differential diagnosis of regular tachycardia with a wide QRS complex. Circulation 1991; 83:1649-59. Therapy for Ventricular Tachycardia • Clinical condition of patient – Unstable requires DC cardioversion – Stable may be treated with Drugs or Cardioversion • Presence or absence of Left ventricular Dysfunction determines choice of pharmacologic therapy – Amiodarone 150 mg I.V. over 10 minutes may be RX of choice maximum 2.2 gm/24 hours class IIA recommendation New ACLS Algorithm VT with Depressed Left Ventricular Function • Amiodarone is Drug of choice – mortality neutral or beneficial – Initial dose 150 mg I.V. over 10 minutes – effective in Ventricular Fibrillation using 300 mg bolus with improved arrival to hospital. • DC cardioversion always acceptable option • Procainamide contraindicated Ventricular Tachycardia with Preserved Left Ventricular Function • • • • DC cardioversion Amiodarone 1st line RX according to ACLS Procainamide Lidocaine – Reduced to 3rd line therapy due to relative little effectiveness in non ischemic VT. • Avoid use of combination Antiarrhythmic agents. Polymorphic VT • Requires immediate defibrillation as does VF • Drug of choice I.V. Lidocaine , Amiodarone • Usually result of severe metabolic disturbance or Cardiac ischemia. • Rarely when associated with prolonged QT known as Torsades de Pointes Monomorphic VT in Patients with Normal Left Ventricular Function • No structural heart disease • Present as palpitations, syncope but rarely as sudden death • Right ventricular outflow tachycardia – LBB morphology inferior axis – adenosine, Calcium channel , occ beta blockers – Amenable to Ablation • Idiopathic Left ventricular tachycardia – RBB superior axis Verapamil and adenosine sensitive – Amenable to Ablation Torsades de Pointes • Polymorphic VT associated with long QT – increased risk if QTC 500 msec or greater QT > 600 msec. • Frequently initiated after pause • Usually Iatrogenic – Hypokalemia,Hypomagnesemia, Drugs, combination • May be congenital – LQT1, LQT2,LQT3 QT Prolonging or Torsadogenic Drugs The following drugs have been shown to prolong the QT interval or have documented clinical Torsades de Pointes reported in the literature Amantadine Quetiapine Aminophylline Quinidine Amiodarone Risperdone Barium Salmeterol Bepridil Thioridazine Chloralhydrate Sparfloxacin Chloroquine Sumatriptan Ciprofloxacin Tacrilimus Cisapride Tamoxifen Sertraline Chlorpromazine Disopyramide Tizanide Dofetilide Trimethorprim Sulfa Doxepine Venlafaxine Droperidol Vistaril Sotalol Flecanide Fluoxetine Foscarnet Fosphentoin Gatifloxin Halofantrine Haloperidol Ibutilide Imipramine Indipamide Isradapine Ketaconazole Levofloxacin Levomethadyl Mesoridazine Moexitine/Hctz Moxifloxicin Naratripan Nicardipine Octreotide Pentamidine Pimozide Probucol Erythromycin Zolmitriptan Felbamate Clarithromycin Terfenadine Desipramine Treatment of Torsades de Pointes • • • • Remove Offending Agent Replete Potassium Treat with Magnesium even if normal Consider increasing heart rate – isoproterenol – Pacing • Treat Congenital with Beta blockers and Pacing or ICD Sudden Death with Normal Left Ventricular Function • Brugada Syndrome – Incompete RBB ST elevation V1V2 – exacerbated by Procainamide and Flecainide – ICD implantation • Right ventricular Dysplasia – Delayed Right Ventricular activation – Epsilon wave , deep precordial Twave inversion – fatty infiltration RV, MRI, RV gram Sudden Death with Normal Left Ventricular Function • Hypertrophic Cardiomyopathy – Majority of sudden death in U.S. in young patients without coronary artery disease – Risk factors extreme hypertrophy(>3.0 cm)exertional hypotension, nonsustained VT,syncope, family history sudden death – ICD effective but appropriate selection for primary prevention problematic Sudden Death with Normal Left Ventricular Function • Brugada Syndrome – Incompete RBB ST elevation V1V2 – exacerbated by Procainamide and Flecainide – ICD implantation • Right ventricular Dysplasia – Delayed Right Ventricular activation – Epsilon wave , deep precordial Twave inversion – fatty infiltration RV, MRI, RV gram Implantable Cardiodefibrillator • Superior to Drug therapy in patients with sudden death and coronary disease • Reduced risk of death in patients with sudden death coronary disease and EF <35% over drugs • Reduces risk of death in patients with inducible VT and reduced L.V. fxn and CAD by nearly 50% Reductions in Mortality with ICDs Compared to Antiarrhythmic Drugs % Mortality Reduction 60% 54% 50% 37% 40% 31% 30% 20% 20% 10% 0% 1 AVID1 CASH2 CIDS3 MADIT4 3 years 2 years 3 years 2 years The AVID Investigators. N Engl J Med. 1997;337:1576-1583. 2 Kuck K. ACC98 News Online. April, 1998. Press release. 3 Connolly S. ACC98 News Online. April, 1998. Press release. AJ. N Engl J Med. 1996;335:1933-1940. 4 Moss SCD-Heft Patients with class II,III CHF EF <35% 34.1% 40 35.8% 35 28.9% 30 25 ICD Amiodarone Placebo 20 15 10 5 0 Mortality at 5 years Conclusion • Most Arrhythmias are reentry • Unstable patient should undergo DC cardioversion, or defibrillation • Class I agents should be avoided in patients with structural heart disease • Amiodarone is drug of choice with depressed left ventricular function Conclusion • Atrial Fibrillation may be treated with rate or rhythm control • WPW patients should be screened for symptoms.If asymptomatic no further evaluation is generally needed. • WPW patients with symptoms or able to conduct faster than 240 BPM should be ablated A 67 year old male with history of previous infarct and reduced LV function presents with palpitations and dizziness. His blood pressure is 80/40. The appropriate next step is ? • A. Synchronized cardioversion for VT • B. I.V. Procainamide for Atrial Fibrillation with WPW syndrome • C. Synchronized cardioversion for unstable SVT with aberrancy. • D. I.V. Amiodarone for SVT with aberrancy in a patient with reduced LV function. Answer A. • This patient has ventricular tachycardia. An RS interval of greater than 100 msec is clearly visible. In addition, by history this patient is overwhelmingly likely to present with VT with a wide complex rhythm. Also this patient is not stable with relative hypotension requiring immediate cardioversion as opposed to pharmacologic therapy. A 24 year old male is referred to you for evaluation due to an unusual ECG. He has never had any palpitations, syncope or near-syncope. Appropriate next step would be which of the following? • A. Immediate for referral for ICD implant • B. Reassurance that no further evaluation is needed at this time • C. Referral for EPS and catheter ablation of his accessory pathway. • D. Send him to someone who knows what this is. Answer B • This patient does indeed have an accessory pathway. However he demonstrates intermittent pre-excitation at a slow rate which places him in a low risk group.Without symptoms, no further evaluation is needed. Every other beat in the ECG is pre-excited. You are called to assess a patient in the SICU for unexplained tachycardia . Which of the following is most correct? • A. The treatment depends on how long the patient has been in this rhythm • B. No treatment is needed as the patient is in sinus tachycardia. • C. Immediate cardioversion should be performed regardless of the rhythm. • D. Adenosine will likely terminate this arrhythmia. Answer A. • This patient is in atrial flutter with variable ventricular response. Flutter waves are intermittently visible on ECG tracing when higher AV block is seen. In addition, flutter waves are visible on the CVP pressure tracing also defining the rhythm. Cardioversion would be inappropriate if the patient had been in this rhythm greater than 48 hours without first performing a TEE given the risk of thromboembolism. A 46 year old female is admitted with dizziness. She is an alcoholic, on methadone, with schizophrenia. She began feeling dizzy after starting a fluoroquinalone for a UTI. Which of the following should be your next step? • A. Administer I.V . Procainamide • B. Consult E.P. for placement of a defibrillator • C. Discontinue antibiotic, treat with I.V. magnesium, discontinue antipsychotic, and consider temporary pacing • D. Administer I.V. amiodarone because it is unlikely cause Torsades de Pointes. Answer C. • This patient has Torsades de Pointes with classic polymorphic VT and prolonged QT demonstrated in the bottom strip. Antipsychotics, hypomagnesemia, quinolones all may predispose to this arrhythmia. Procainamide or amiodarone would worsen this rhythm. ICD is not indicated .