* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Pneumonia Decisions
Leptospirosis wikipedia , lookup
Anaerobic infection wikipedia , lookup
Oesophagostomum wikipedia , lookup
Schistosomiasis wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Marburg virus disease wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Neisseria meningitidis wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
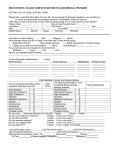
PNEUMONIA Dr.M.Shahparianpour Mr. P • 92 yo male w/ h/o fall 3 days prior to admission, came to ER with c/o mental status changes (per NH staff), and 1 day h/o vomiting and dyspnea. • Pmhx of alzheimers, emphysema, glaucoma. • Meds included 5 different eye drops and donepezil. No drug allergies. • Shx: nursing home resident, no recent etoh or tobacco. Daughter involved. • Pneumovax 2001, flu vaccine 2002. • PE: T 97.9, rr 22, bp 109/65, p 77, 70% RA oxygen saturation. • Confused, non-rebreather in place. Heent wnl. Lungs: coarse crackles bilaterally. CV: reg, s1s2, no mrg. Abd: wnl. Ext: +2 ankle edema. Neuro: nonfocal, not oriented, following some commands. • Labs remarkable for wbc 12.6 w/ 90% n, chem 7 wnl, po2 on ABG of 38 mm Hg (ph 7.44) • CXR w/ ? small RLL infiltrate, but portable film, final read by radiology negative. Does this patient have pneumonia? In other words, how do you define pneumonia? Why is diagnosing pneumonia important? And if he has pneumonia, what kind, and how do you investigate possible causes further? How do you triage the patient? How do you treat him? When do you send him home? Could it have been prevented? • Pneumonia is defined as inflammation and consolidation of the lung tissue due to an infectious agent. • • Pneumonia that develops outside the hospital setting is considered community-acquired pneumonia Pneumonia developing48 hours or more after admission to the hospital is termed nosocomial or hospital-acquired pneumonia. • Community-acquired pneumonia is caused most commonly by bacteria that traditionally have been divided into 2 groups, typical and atypical. • Typical organisms include S pneumoniae (pneumococcus) and Haemophilus and Staphylococcus species. • Atypical refers to pneumonia caused by Legionella, Mycoplasma, and Chlamydia species. Definition (perof IDSA) Acute infection the pulmonary parenchyma accompanied by: • Acute infiltrate on CXR or auscultatory findings consistent with pneumonia • And usually two of the following: fever or hypothermia, rigors, sweats, new cough with or without sputum (or change in color), chest discomfort, dyspnea. • In the elderly, more common to be afebrile/hypothermic, and altered mental status sometimes is the ONLY complaint. Pneumonia • Community • Nosocomial • Eldery house • Immunocompromised host • Community-acquired pneumonia remains a common illness. • pneumonia is reported to be 170 cases per 100,000 persons. • Estimates of incidence of nosocomial pneumonia range from 4-7 episodes per 1000 hospitalizations. • Approximately 25% of patients in intensive care units (ICUs) develop pneumonia. • 20% result in hospitalization • With advancing age, the incidence increases 3 folds in patients( aged 44 years to 65 years) • Pneumonia as a cause of hospitalization increased from 36 to 48 cases per 100,000 persons between 1984 and 1995. • Pneumonia is the sixth leading cause of death • the most common infectious causes of death. • The mortality rate is reported to be 1% in the outpatient setting but may increase to up to 25% in those requiring hospital admission. • In a patient with preexisting respiratory disease, onset of bacterial pneumonia may result in deterioration of respiratory status, leading to respiratory failure and death. • Nosocomial pneumonia is the leading cause of death among hospital-acquired infections. • Recent studies have shown that nosocomial pneumonia causes excessive risk of death, and the mortality rates range from 20-50%. • Although less common in the antibiotic era, bacterial pneumonia may lead to bronchiectasis. • However, lower respiratory infection with pneumococci, staphylococci, and Klebsiella species may result in bronchiectasis, especially if treatment is delayed. • Incidence is greater in males than in females. • Advanced age increases the incidence of pneumonia and the mortality from pneumonia. • Elderly persons have • weaker immune responses, • higher risk of aspiration, • comorbidities. • Resistant bacteria are becoming an increasing problem, which affects treatment. • We have an increasing population with immunosuppression or chronic diseases (which impacts cause and mortality) Pathogenesis of typical pneumonia • S pneumoniae generally resides in the nasopharynx and is carried asymptomatically in approximately 50% of healthy individuals. • Invasive disease may occur upon acquisition of a new epithelium serotype. • A strong association exists with viral illnesses, such as influenza. • Viral infections increase pneumococcal attachment to the receptors on activated respiratory epithelium. • Once aspirated from the nasopharynx to the alveolus, pneumococci infect type II alveolar cells. • The pneumonic lesion progresses as pneumococci multiply in the alveolus and invade alveolar epithelium. • Pneumococci spread from alveolus to alveolus through the pores of Kohn, thereby producing inflammation and consolidation along lobar compartments. Pathogenesis of atypical infection • After inhalation, the atypical organisms attach to the respiratory epithelial cells by a variety of mechanisms. • The presence of pili on the surface of Legionella species facilitates attachment. • Once adhered, the organisms cause injury to the epithelial cells and their associated cilia. • Many of the pathogenetic mechanisms may be immune-mediated rather than due to direct injury by the bacteria. • A host defense is mounted via cellmediated and humoral immunity. • Infection caused by atypical organisms often spreads beyond the lobar boundaries and frequently is bilateral. Pathogenesis of nosocomial pneumonia • Aspiration plays a central role in the pathogenesis of nosocomial pneumonia . • Approximately 45% of healthy subjects aspirate during sleep, and an even higher proportion of severely ill patients aspirate routinely. • Depending on the number and virulence of the pathogenic organisms reaching the lower respiratory tract and on the host defense factors, pneumonia may develop. • The oropharynx of hospitalized patients may become colonized with aerobic gramnegative bacteria within a few days of admission. • Therefore, nosocomial pneumonia is caused predominantly by the gram-negative bacilli. • However, the incidence of Staphylococcus aureus lower respiratory tract infection is increasingly common in the hospitalized and institutionalized patient and must now be considered a possible pathogen for nosocomial pneumonia. Pneumonia Decisions • PORT • Microbiology • Empiric Therapy Pneumonia Routes of Transmission • Inhalation • Aspiration • Blood-borne Community Acquired Pneumonia etiology S.pneumoniae H.influenzae Other Anaerobes L.pneumophilia M.pneumoniae C.pneumoniae Community - Acquired • • • • • • • • • • Bacteria Streptococcus pneumoniae Hemophilus influenzae Staphylococcus aureus “Atypical” Mycoplasma pneumoniae Chlamydia pneumoniae Virus Influenzae Adenovirus % Cases 50-70 10-15 5 10-30 10-20 Epidemic Community Pneumonia Microbiology • • • • • Unusual / Don’Miss • Very Unusual • • • PCP Tb Moraxella Legionella Hantavirus Fungi (cocchisto) Anthrax, SARS Different categories of pneumonia and common pathogens • Patients w/ minimal co-morbidities (cause identified only 50% of the time): • S. pneumoniae (most common overall) • M. pneumoniae/C. pneumoniae • Viruses • Chronic pulmonary/cardiovascular disease: • • • • Drug resistant S. pneumoniae H. influenza M. catarrhalis Legionella • Nosocomial (hospitalized or nursing home patients): • • • • • Resistant GNR’s Pseudomonas aeruginosa S. aureus (MRSA) Aspergillosis Anaerobes (aspiration) • In alcoholics: • Klebsiella pneumoniae, anaerobes, TB • IVDU: • S. aureus, PCP, anaerobes • Post-splenectomy: • S. pneumoniae, H. influenza • HIV/AIDs: • PCP, S. pneumonia, TB, fungal • Leukemic patients/bone marrow transplant: • Aspergillosis, legionella, CMV, other fungal. • Post influenza: • S. pneumoniae, S. aureus • Cystic fibrosis: • Pseudomonas aeruginosa, S. aureus • In patients who have received solid organ transplants, pneumonia from S pneumoniae may occur more than 3 months after the transplant. • Other organisms include Legionella species, Pneumocystis carinii, and cytomegalovirus. • Sickle cell disease may indicate S pneumoniae or H influenzae infection. • Diabetic ketoacidosis may lead to S pneumoniae or S aureus infection • Animal exposure: • C. psittaci, Cryptococcus neoformans, Histoplasmosis capsulatum (birds) • Tularemia (rabbit), plague (rat), hantavirus (deer mouse), H. capsulatum (bat). • Q fever (C. burnetii) – farm animals • Travel: • SARS (Asia), coccidiomycoses, (SW USA), Legionella (endemic/epidemic areas). This sputum smear shows staphylococcus bacteria using Gram stain technique in a patient with staphylococcal pneumonia. A photomicrograph of Streptococcus spp. bacteria using Gram stain technique. Scanning electron micrograph of S. pneumoniae Photomicrograph of Streptococcus pneumoniae bacteria revealing capsular swelling using the Neufeld-Quellung test. Pneumocystis carinii, now called P. jiroveci, is present in this lung impression smear, using Giemsa stain. A photomicrograph of Pseudomonas aeruginosa bacteria. Photomicrograph of Haemophilus influenzae as seen using a Gram stain technique. MYCOPLASMA History • Clinical presentation in patients with pneumonia varies from a mildly ill ambulatory patient to a critically ill patient with respiratory failure or septic shock. • The character of sputum produced may suggest a particular pathogen. • Patients with pneumococcal pneumonia may produce bloody or rustcolored sputum. • Infections with Pseudomonas, Haemophilus, and pneumococcal species are known to expectorate green sputum. • Anaerobic infections characteristically produce foul-smelling and badtasting sputum. • Currant-jelly sputum suggests pneumonia from Klebsiella or pneumococcal species. • Patients may report rigors or shaking chills. • Patients may complain of other nonspecific symptoms, which include headaches, malaise, nausea, vomiting, and diarrhea. • These symptoms may suggest infection with Legionella, Chlamydia, or Mycoplasma species. • Malaise, myalgias, and exertional dyspnea may be observed. • Pleuritic chest pain or abdominal pain secondary to pleuritis is a common feature of pneumococcal infection, but these may occur in other bacterial pneumonias. Physical examination • Physical examination findings vary depending on the type of organisms, severity of pneumonia, coexisting host factors, and presence of complications. • The common findings of consolidation are as follows: • • • • • • • • • • • Fever or hypothermia (temperature >38.5°C or <36°C) Tachypnea (respiratory rate >18 breaths per min) Tachycardia or bradycardia Central cyanosis Dullness to percussion over pneumonic consolidation Decreased intensity of breath sounds Rales or crackles Egophony upon auscultation Whispering pectoriloquy Pleural friction rub Altered mental status • Physical examination findings that may indicate the etiology of pneumonia are as follows: • Periodontal disease with foul-smelling sputum - Anaerobes, possible mixed aerobic-anaerobic infection • Bullous myringitis - Mycoplasma pneumoniae • Absent gag reflex, altered level of consciousness, recent seizure - Polymicrobial (aerobic and anaerobic), possible macroaspiration or microaspiration • Encephalitis - M pneumoniae, C burnetii, L pneumophila • Cerebellar ataxia, erythema multiforme, erythema nodosum Chlamydia pneumoniae, M tuberculosis • Erythema gangrenosum - Pseudomonas aeruginosa, Serratia marcescens • Cutaneous nodules (abscesses and CNS findings) - Nocardia species Lab Studies • Leukocytosis with a left shift, although commonly observed in any bacterial infection, may be absent in patients who are elderly or debilitated. • Leukopenia (defined as a WBC count of <5000) is an ominous sign of impending sepsis and portends a poor outcome. • Sputum examination provides an accurate diagnosis in approximately 50% of patients. • An adequate specimen must have less than 10 squamous epithelial cells and more than 25 WBCs per low-power field. • However, the number of WBCs in the sputum of a neutropenic patient may be fewer than 25 WBCs per low-power field, despite origination from the lower respiratory tree. • A single pathogen present on the Gram stain is indicative of pneumonia; • mixed flora may indicate oral contamination or anaerobic infections. • An adequate specimen uncontaminated by oral flora is required for a proper workup. • Sputum cultures are submitted only from specimens that are deemed satisfactory after Gram stain. • Other tests may include the following: • Urinary antigen testing for Legionella serogroup 1 has a high yield. • A urinary antigen test for pneumococcus is available and may be performed at the bedside. • A Legionella serum antibody titer rising by 1:128 confirms the diagnosis retrospectively. Mycoplasma and Chlamydia immunoglobulin M antibodies contribute to the diagnosis. • Serology is essential in the diagnosis of unusual causes of pneumonia such as Q fever and brucellosis. • Culture and Gram stain of pleural effusions or empyema fluid has a high yield. • Pleural fluid pH determination should be made to classify the effusion as simple versus complicated. • The Legionella-specific direct fluorescent antibody test is performed when indicated, even though this technique is associated with a high rate of falsenegative results • Performing blood cultures is important, but the results have a limited value. • When positive, the results confirm a causative agent. • Blood cultures are positive only in approximately 40% of cases, Imaging Studies Chest radiograph findings may indicate the following: • In a patient with a clinical picture of pneumonia, pathogenic organisms may be suggested based on the chest radiographic pattern. • The common patterns are described as follows: • Focal opacity (segment or lobar pneumonia) - S pneumoniae, M pneumoniae, L pneumophila, S aureus, C pneumoniae, M tuberculosis, B dermatitidis • Interstitial pattern (diffuse process identified as reticulonodular or reticular process) - M pneumoniae, P carinii, C psittaci • Interstitial pattern with hilar and/or mediastinal lymphadenopathy - Epstein-Barr virus, Francisella tularensis, C psittaci, M pneumoniae, fungi • Cavitation or necrotizing pneumonia - Mixed aerobicanaerobic infection (lung abscess), aerobic gram-negative bacilli, M tuberculosis, L pneumophila, C neoformans, Nocardia asteroides, Actinomyces israelii, C immitis • Bulging oblique or horizontal fissure - K pneumoniae, L pneumophila • Multifocal bilateral segment or lobar opacities - S aureus, C burnetii, L pneumophila, S pneumoniae • Miliary (diffuse micronodular) pattern - M tuberculosis, H capsulatum, C immitis, B dermatitidis, varicella zoster • Pneumatoceles (thin-walled cavities) - S aureus, Streptococcus pyogenes, P carinii • "Round" pneumonia (often presents as solitary pulmonary nodule) - C burnetii, S pneumoniae, L pneumophila, S aureus • Bronchoscopy: Bronchial washing specimens can be obtained. • Protected brush and bronchoalveolar lavage can be performed for quantitative cultures. • Transtracheal aspiration for culture: • This procedure is mentioned primarily for historical significance. This method of obtaining lower respiratory secretions has been replaced by fiberoptic bronchoscopy. • Thoracentesis: This is an essential procedure in patients with a parapneumonic pleural effusion. Triage (home, admit, step down, ICU) • Decision based on patient’s clinical condition, risk of death and complications, presence of other medical problems, social support. • Age more than 65 yo alone is not an indication for admission. • All patients with new hypoxemia (sat <90% or Po2 <60mm Hg), hemodynamic instability** should be hospitalized. Pneumonia Severity Index (PSI) • Based on data available at presentation (age, coexisting illnesses, findings on PE, lab and radiographic findings). • Stratifies patients into five risk classes. • 30 day mortality estimated for each risk class (.1%-27%). • Patients in risk class I-III at low risk of death – most can be safely treated as outpatient. Risk class IV and V should definitely be hospitalized (for both consider step-down bed, or ICU for class V). Diagnosis of CAP Can CAP be reliably differentiated from other respiratory conditions by clinical features alone? NO The diagnosis of CAP on the basis of history and physical findings is inaccurate without a chest radiograph. Nosocomial Pneumonia Major Factors: • Alteration oropharyngeal flora • Aspiration • Contaminated aerosol nebulizers • Attendant’s hands • Injudicious use antibiotics Pneumonia Microbiology • Organisms • • • • • • Acquired % Strep pneumonia Staph aureus Pseudomonas aerug Klebsiella Enterobacter • Hemophilus • Anaerobes • Atypical hospital 5 15 31 12 15 community 50 5 2 1 1 1 2 2 10 5 30 Pneumonia Physiologic Impairment • Hypoxemia (low V/Q) • shunt • Hyperventilation (low PCO2, high pH) • Restriction Elderly Patients with CAP • Classic symptoms and signs of pneumonia less likely • Non-specific symptoms especially confusion, more likely • Comorbid illness more common • Higher mortality rate • Fever less likely • Aspiration is a risk factor Algorithm Patient with community-acquired pneumonia Is the patient > 50 years of age Yes No Does the patient have a history of any of the following comorbid conditions ? Neoplastic disease Congestive heart failure Cerebrovascualr disease Renal disease Liver disease Yes No Does the patient have a history of any of the following abnormalities on physical examination Altered mental status Pulse ≥ 125 / minute Respiratory rate ≥ 30 / minute Systolic blood pressure < 90 mmHg Temp < 35° C or ≥ 40° C No Assign patient to risk class I Yes Assign patient to risk class II-V based on prediction mosel scoring system Prediction model for C A P Patient Points characteristics assigned Demographic factors Age: males age (in yrs) females age (in yrs) -10 Nursing home resident +10 Comorbid illnesses Neoplastic disease +30 Liver disease + 20 Congestive heart failure +10 Cerebrovascular disease +10 Renal disease +10 Physical examination findings Altered mental status +20 Respiratory rate ≥ 30/mi +20 Systolic blood pressure < 90 mmHg +20 Temp. < 35° C or ≥ 40° C +15 Pulse >125 / min +10 Laboratory findings pH < 7.35 BUN > 10.7 mmol/L Sodium < 130 mEq/L Glucose > 13.9 mmol/L Hematocrit < 30% PO < 60 mmHg2 Pleural effusion +30 +20 +20 +10 +10 +10 +10 Stratification of Risk Score Risk Risk class I Low II Moderate lll IV High V Based on Algorithm < 70 total points 71-90 total points 91-130 total points > 130 total points Flow Chart Approach to Treating Outpatients and Inpatients with C.A.P. Patient with suspected pneumonia Chest radiograph Decision to hospitalize Managed as outpatient Hospitalized patient Expectorated sputum No sputum Sputum for stain (optional) Empirical antibiotic treatemnt Gram stain or other rapid test identifies likely pathogen Antibiotic treatment selected for pathogen No rapid diagnostic test positive Empirical treatment Subsequent data (blood culture, sputum culture, etc.) yields likely pathogen Empirical treatment Risk-Class Mortality Rates for Patients with Pneumonia Risk class No. of points Mortality (%) Recommendations for site of care I No predictors 0.1 Outpatient II < 70 0.6 Outpatient III (briefly) 71- 90 2.8 Inpatient IV 91 - 130 8.2 Inpatient V > 130 29.2 Inpatient CORE ADVERSE PROGNOSTIC FEATURES (CURB SCORE) Confusion : Abbreviated Mental Test score of 8 or less Urea : raised >7mmol/l (for patients being seen in hospital) Respiratory rate: raised ≥30/min Blood pressure: low (systolic <90 mmHg and/or diastolic ≤60 mmHg) These features (except Urea) should be assessed for ALL patients. The Abbreviated Mental Test Each question scores 1 mark, total 10marks • Age • Date of birth • Time (to nearest hour) • Year • Hospital name • Recognition of two persons • Recall address • Date of major event • Name of monarch (president) • Count backwards 20 →1 “Pre-existing” Adverse Prognostic Features • Age 50 years and over • Presence of coexisting disease Congestive cardiac failure Coronary artery disease Stroke Diabetes mellitus Chronic lung disease Cancer “Additional” Adverse Prognostic Feature If available to some GPs who have oximeters. • Hypoxaemia (Sao2 <92% or Pao2 <8kPa) Consider “core” adverse prognostic features None present Consider “pre-existing” adverse prognostic features NO Home management* 1 feature present YES 2 or more features present Consider “additional “ adverse prognostic feature if available Clinical judgement Refer to hospital Associated Mortality by Age and Treatment Age Mortality 18-64 yr 10% - 15% 65-74 yr 20% 75-84 yr 30% > 85 yr 40% Untreated 50% - 90% Patient Preference: Inpatient vs. Outpatient Therapy 80% 80% 74% 60% 40% 20% 0% 9% Patients Favoring Outpatient Therapy Patients willing to pay 24% of Monthly Income to Ensure Outpatient Therapy Patients Favoring Inpatient Therapy Antibiotic Decision Making • Severity of disease • Microbiology environment • Patient • Host status • Individual considerations • Practice Guidelines Antibiotic Use • Empiric oral vs.. parenteral • Loading dose • Dosing • Speed of delivery • Switch to oral from IV • Duration of therapy Bacteriology of HospitalAcquired Pneumonia Early-Onset Pneumonia Late-Onset Pneumonia Other S pneumoniae P aeruginosa Anaerobic bacteria H influenzae Enterobacter sp Legionella pneumophilia Moraxella cattarrhalis Acinetobacter SP Influenza A and B S aureus K pneumoniae Aerobic gram-negative bacilli Respiratory syncitial virus S marcenscens Fungi E coli Other gram-negative bacilli S aureus PREVENTION Vaccination strategies Influenza vaccine Pneumococcal vaccine Pneumococcal vaccine • Pneumococcal vaccine: contains purified capsular polysaccharide from the 23 serotypes that cause 85-90% of the invasive pneumococcal infections in adults and children in the United States. • Cost-effective among individuals over the age of 65 for prevention of bacteremia. • Benefit has been shown in some studies for patients with diabetes, CHF, chronic pulmonary disease, asplenia. • Effectiveness has not been proven in immunosuppressed, but still recommended. • Antibody response declines over 5-10 years. • Revaccination after 5 years given to patients who received initial vaccination when less that 65 yo age, asplenic patients, and immunocompromised. Influenza vaccine • Influenza vaccine: modified annually to reflect the anticipated strains in the upcoming season. • The vaccine virus is grown in eggs, purified, and inactivated (does not contain live virus). • Efficacy can range from 70-90%. Shown to reduce all-cause mortality during influenza season by 27-54%. • Groups that benefit: age>65, residents of nursing homes, patients with chronic lung or cardiovascular disease, people frequently hospitalized, pregnant women in 2nd/3rd trimester, health care providers, HIV patients, travelers to foreign countries during influenza epidemics. • Need vaccination yearly (Sept – Feb). • New, live attenuated virus vaccine only for children and healthy adults <age 50. . The end INFLUENZA VACCINE • Primary influenza pneumonia is rare and carries a high mortality rate • Secondary bacterial pneumonia is more common notably due to S aureus • Bronchitis is also a common complication • The greatest mortality is in those patients with underlying disease INFLUENZA VACCINE Evidence on Efficacy Based on several large well designed case-control field studes from North America Other studies from UK and Netherlands INFLUENZA VACCINE Results of Studies:Reduces hospital deaths from pneumonia and influenza by about 65% and from all respiratory causes by 45% Decreases hospital admissions and outpatient visits PNEUMOCOCCAL VACCINE Recommendations in U.K. Asplenia Severe spleen dysfunction Chronic renal disease Chronic heart disease Chronic lung disease Chronic liver disease Diabetes mellitus Immunosuppression/Immunodefi ciency PNEUMOCOCCAL VACCINE EFFICACY STUDIES • Protection offered of around 66% against definitive pneumococcal pneumonia with bacteraemia for “normal” or “low risk” adults . • NO evidence that vaccine is effective in “high risk” groups and in those aged 60 to 70 years. NOSOCOMIAL PNEUMONIA Disease Definition new cough auscultatory findings new infiltrate or progressive infiltrate(s) on chest radiograph, accompanied by: fever or hypothermia, leukocytosis, sputum production Etiology: polymicrobial Disease Definition - cont’d Acquired by a patient in the following settings: in a hospital or long-term-care facility after being admitted for >48 hours or <7 days after a patient is discharged from hospital ( patient’s initial hospitalization should be 3 days duration ) Risk Factors Host factors ( e.g. extremes of age, severe underlying disease ) Colonization by gram-negative microorganisms Aspiration or reflux Prolonged mechanical ventilation Factors that impede adequate pulmonary toilet Problems in Diagnosis of NP Clinical criteria lack specificity No “gold standards” for diagnostic procedures (e.g. invasive procedures) High potential for more than one ongoing infectious process Use of antimicrobials in ICU empirically or use for infections of other sites or organs.