* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Inner-City Asthma Intervention
Survey
Document related concepts
Transcript
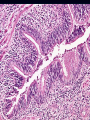
CHRONIC OBSTRUCTIVE PULMONARY DISEASE Chronic Obstructive Pulmonary Disease (COPD) Chronic Obstructive Airway disease (COAD) DEFINITION COPD is a disease state characterized by increase in resistance to airflow due to partial or complete obstruction of airway at any level from the trachea to respiratory bronchiole. Changes are usually irreversible esp. in chronic bronchitis and emphysema. - Predominant symptom; Dyspnoea - Predominant cause; Smoking Pulmonary function tests show : 1-Increased pulmonary resistance 2- Limitation of maximal expiratory flow rates (reduced FEV1). 1. EMPHYSEMA 2. CHRONIC BRONCHITIS 3. ASTHMA 4. BRONCHIECTASIS Emphysema. -Abnormal permanent enlargement of the distal air spaces due to destruction of the alveolar walls and loss of respiratory tissue. -“Obstruction” is caused by lack of elastic Etiology: 1- Most common cause is smoking: produces combination of emphysema and chronic inflammation 2- Genetic deficiency of alpha1 antitrypsin (Pi locus on chromosome 14) ; alpha-1-antitrypsin produces almost pure emphysema deficiency Pathogenesis: 1- Protease-antiprotease imbalance: . Alpha1 antitrypsin present in serum, tissue fluids, macrophages . Inhibitor of proteases (esp. elastase secreted by neutrophils during inflammation) .Stimulus--TNF,IL8--Increased neutrophils-- Pathogenesis 2- Oxidant-antioxidant imbalance: Smoking--Free O2 radicals--Deplete Antioxidant in lung (superoxide dismutase, glutathione)—Damage of lung tissue Types of Emphysema 1-Centroacinar (Centrilobar) Emphysema -- Affects central (proximal) parts of the acini (respiratory bronchioles) but spares the distal alveoli. - More severe in upper lobes, especially apical segments . Causes: -Smoking -Coal dust 2-Panacinar (Panlobar) Emphysema -- Uniform enlargement of the acini in a lobule. - May not necessarily involve entire lung - Predominantly lower lobes. - Alpha -1- antitrypsin deficiency is prototype. 3-Paraseptal (Distal Acinar) Emphysema -- Proximal acinus normal, distal part involved - Most prominent adjacent to pleura and along the lobular connective tissue septa. - Probably underlies spontaneous pneumothorax in young adults. 4-Bullous Emphysema -- Any form of emphysema which produces large subpleural blebs or bullae (> 1cm). - Localized accentuation of any one of the type. 5-Interstitial Emphysema Air penetration into the connective tissue stroma of the : - lung - mediastinum or - subcutaneous tissue. 6-Compensatory “Emphysema” - Dilatation of alveoli in response to loss of lung substance elsewhere. - Actually hyperinflation destruction of septal walls. since no 7-Senile “Emphysema” - Change in geometry of lung with larger alveolar ducts and smaller alveoli. - No loss of lung tissue; hence not really an emphysema. Chronic Bronchitis - Clinical definition: persistent cough with sputum production for at least three months in at least two consecutive years. - Can occur with or without evidence of airway obstruction - Smoking is the most important cause. Basic Mechanism: : Hypersecretion of mucus Histology -Increased numbers of goblet cells in small airways as well as large airways. -Increased size of submucosal glands in large airways (Reid index: ratio of thickness of mucosal glands to thickness of wall between epithelium and cartilage) -Peribronchiolar chronic inflammation. Bronchiectasis - Permanent abnormal dilation of bronchi and bronchioles, - Usually associated with chronic necrotizing inflammation - Patients have fever, cough, foul–smelling sputum. - More common in left lung, lower lobes. Causes: Obstruction (tumor, mucus) Congenital Intralobar sequestration Cystic fibrosis Immotile cilia syndrome Necrotizing pneumonia Kartaganer’s Syndrome Asthma - Increased responsiveness of tracheobronchial tree to various stimuli, leading to paroxysmal airway constriction - Unremitting attacks (status asthmaticus) can be fatal. Etiology : 1- Extrinsic Factors (atopic, allergic); most common 2- Intrinsic Factors recognize mixed. (idiosyncratic); now Basic Mechanism - Bronchial plugging by thick mucous plugs containing eosinophils, whorls of shed epithelium (Curschmann’s spirals), and Charcot – Leyden crystals (Eosinophil membrane protein); - Distal air- spaces become over distended. Histology: -Thick basement membrane -Edema and infiltration of the bronchial walls by inflammatory cells with prominence eosinophils, - Hypertrophy of bronchial wall muscle. of Therapeutic agents are aimed at increasing cAMP levels either by : - increasing epinephrine) production (ß-agonists, e.g or - decreasing degradation (Methyl xanthines, e.g theophylline). - Cromolyn degranulation. sodium prevents mast cell Allergic Bronchopulmonary Aspergillosis Occur in chronic asthmatics; hypersensitivity to non – invasive Aspergillus. Bronchocentric mucus granulomatous impaction of bronchi, inflammation, eosinophilic pneumonia. Distinctive (?Pathgnomonic) promixal bronchiectasis Burden of Asthma Prevalence increasing in developed countries more than developing or underdeveloped countries affecting 10 15% of population. The number of children with asthma has increased sixfold in the last 25 years Between 100 and 150 million people around the globe 5.1 million people in the UK have asthma In South Asia (including Pakistan) rough estimates indicate a prevalence of between 10% and 15% Burden of Asthma World-wide, the economic costs associated with asthma are estimated to exceed those of TB and HIV/AIDS combined. In the United States, for example, annual asthma care costs (direct and indirect) exceed US$6 billion. At present Britain spends about US$1.8 billion on health care for asthma and because of days lost through illness Burden of Asthma Age-adjusted death rate per million 25 Under 5 years 20 15 10 5-14 years 5 0 1980 15-34 years 1985 1990 1995 19992000 2011 2010 Target 35-64 years 65 years and over 0 80 20 40 60 Deaths per Million CLASSIFICATION OF ASTHMA EXTRINSIC Implying a definite external cause Atopic individuals Positive skin prick test More common Early onset in childhood INTRINSIC OR CRYPTOGENIC Late onset (middle age) Etiology and Pathogenesis Allergy Airway hyperresponsiveness Genetic factors Asthma triggers The Underlying Mechanism Risk Factors (for development of asthma) INFLAMMATION Airway Hyperresponsiveness Airflow Limitation SymptomsRisk Factors (shortness of breath, (for exacerbations) cough, wheeze) Pathological changes Genetic Factors Candidate genes on chromosome 5q31-33 (IL4 GENE CLUSTER) Responsible for production of cytokines ,IL3,IL4 ,IL9 ,IL13, GM-CSF Gene A Gene D Atopy susceptible Gene B Gene C Asthma susceptible Gene E Asthma triggers Indoor allergens Outdoor allergens Occupational sensitizers Tobacco smoke Air Pollution Respiratory Infections Parasitic infections Socioeconomic factors Family size Diet and drugs Obesity Exercise Acid reflux Burden of COPD The global burden of COPD will increase enormously over the foreseeable future as the toll from tobacco use in developing countries becomes apparent. In UK and USA COPD occurs in 18% male smokers 14% female smokers 6-7% those who have never smoked Direct and Indirect Costs of COPD, (US $ Billions) Direct Medical Cost: $18.0 Total Indirect Cost: $ 14.1 Mortality related IDC 7.3 Morbidity related IDC 6.8 Total Cost $32.1 Risk Factors for COPD Host Factors Genes (e.g. alpha1-antitrypsin deficiency) Hyperresponsiveness Lung growth Exposure Tobacco smoke Occupational dusts and chemicals Infections Socioeconomic status Pathogenesis of COPD NOXIOUS AGENT (tobacco smoke, pollutants, occupational agent) Genetic factors Respiratory infection Other COPD Noxious particles and gases Host factors Lung inflammation Anti-oxidants Oxidative stress Anti-proteinases Proteinases Repair mechanisms COPD pathology ASTHMA COPD Sensitizing agent Noxious agent Asthmatic airway inflammation CD4+ T-lymphocytes Eosinophils Completely reversible COPD airway inflammation CD8+ T-lymphocytes Macrophages Neutrophils Airflow limitation Completely irreversible Symptoms and Signs Acute attack of asthma Intermittent dyspnoea Cough, sputum ,wheeze Tachypnoea Hyperinflated chest Hyperresonant percussion note Diminished air entry Widespread polyphonic wheeze Acute exacerbation of COPD Dyspnoea , cough ,sputum, wheeze Tachyponea Use of accessory muscles reduced cricosternal distance <3cm Reduced expansion Hyperinflation Hyperresonant percussion note Quiet breath sounds Wheeze , cyanosis Cor pulmonale Signs of severe attack of asthma Inability to complete sentence Pulse>110 Respiratory rate >25 PEFR <50%of predicted Signs of Life threatening attack Silent chest Cyanosis Bradycardia Exhaustion Confusion Feeble respiratory effort PEFR <33% of predicted Low pH <7.35, PaO2< 8KPa , PaCO2>5KPa Investigations for acute attack of asthma Full Blood Count Urine Complete and Electrolytes PEFR (pt may be too ill to perform it well) Arterial Blood Gases Pulse oximetry ECG CXR Investigations for Acute Exacerbation of COPD Full Blood Count Urine Complete and Electrolytes PEFR (pt may be too ill to perform it well) Arterial Blood Gases Pulse oximetry ECG CXR Blood cultures (if Pyrexial) Sputum for culture Differential Diagnosis Asthma COPD Pneumothorax Pulmonary edema Upper respiratory tract obstruction Pulmonary embolus Anaphylaxis Management Plan Immediate management to stabilize the patient Long term management of disease Prevention of further attacks Immediate management of acute asthmatic attack B2 Agonists Salbutamol 5mg or Terbutaline 10mg nebulized with O2 (se;tacchycardia,tremor,hypokalemia,arrythmia) Corticosteroids Hydrocortisone 200 mg iv or Prednisolone 30 mg oral (both if very ill) Immediate management of acute asthmatic attack Additional management in Life threatening attack Nebulize with Anti cholinergics (Ipratropium 0.5 mg add to B2agonist) Aminophylline 250 mg (5mg/kg) I/V over 20 mins I/V B2 agonists Salbutamol or Terbutaline 0.25mg over 10 mins Effects of Corticosteroids in Acute Asthma Systemic Corticosteroids Anti-inflammatory Late improvement in outcomes (> 6 hrs) Corticosteroids induce transcriptional effects synthesis of new proteins Inhaled Corticosteroids Topical Early improvement in outcomes (< 3 h) Corticosteroids upregulating postsynaptic adrenergic receptors airway mucosa, vasoconstriction decrease airway mucosal blood flow, mucosal decongestion Complications Respiratory failure Type I continuous O2 Type II controlled O2 Intubation and ventilation Cor pulmonale Pneumothorax (ruptured bulla …bullous lung disease, Indication of surgery) Chest infection (pneumonia) Polycythemia Complications Respiratory failure Treatment options; Noninvasive Positive Pressure Ventilation Intubation Sedatives and Neuromuscular Blockers PREVENTION Elimination of risk factors Patient education and information Advice on not missing the dose Proper management plan Addition of mast cell stabilizers like sodium cromoglycate and nedocromil and leukotriene antagonists e.g; montelukast and zafirlukast to traditional therapy