* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download NSAIDs not 4 322
Pharmacogenomics wikipedia , lookup
Pharmacognosy wikipedia , lookup
Discovery and development of direct Xa inhibitors wikipedia , lookup
Neuropharmacology wikipedia , lookup
Drug interaction wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Metalloprotease inhibitor wikipedia , lookup
Hyaluronic acid wikipedia , lookup
Discovery and development of integrase inhibitors wikipedia , lookup
Discovery and development of neuraminidase inhibitors wikipedia , lookup
Psychopharmacology wikipedia , lookup
Discovery and development of ACE inhibitors wikipedia , lookup
Discovery and development of proton pump inhibitors wikipedia , lookup
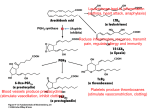
Discovery and development of cyclooxygenase 2 inhibitors wikipedia , lookup
Dr. Yieldez Bassiouni Inflammation The inflammatory process is a normal response to injury. Inflammation is considered the first step in the process of healing. Inflammation can become exaggerated, which leads to further tissue damage. Inflammation When tissues are damaged, substances like histamine, bradykinin, PGs, 5HT are released that produce vasodilation and increased permeability of the capillary walls Leukocytes migrate to the area to destroy harmful substances introduced by the injury. Redness, swelling (edema), warmth, pain, and loss of function. 1-3 Mediators of inflammation Prostaglandins Mediate pain, fever and headache Produced via cyclooxygenase pathway Cyclooxygenase pathway produce prostaglandins, prostacyclines and thromboxanes Thromboxanes causes vasodilation which lead to headache. Cyclooxygenase enzymes make prostaglandins from acracadonic acid in the cell membrane Leukotriens produced via lipooxygenase pathway components of the lipid-signalling pathway have potential role in the inflammatory cascade as contributors to pain. Antiinflammatory Drug Action Steroidal antiinflammatory drugs decrease inflammation by inhibiting arachidonic acid formation. Nonsteroidal antiinflammatory drugs decrease inflammation by inhibiting cyclooxygenase enzymes. 20-8 NSAIDs NSAIDs are group of drugs that share in common the capacity to induce: Analgesic effect. Antipyretic effect. Anti-inflammatory effect. Paracetamol is an analgesic and antipyretic drug with no antiinflammatory activity. It is not included in NSAIDs. ANALGESIC Drug that relieve pain. ANTIPYRETIC Drug that lower the elevated body temperature to normal. MOA OF NSAIDS PGs have protective effect on GIT PGs (generated via COX-1) 1) inhibit stomach acid secretion, 2) stimulate mucus and HCO3- secretion, vasodilation and therefore, 3) are cytoprotective for the gastric mucosa. Therefore, NSAIDs with COX-1 inhibitory activity will produce gastric irritation Cyclo-oxygenase (COX) Exists in the tissue as constitutive isoform (COX-1). At site of inflammation, cytokines stim the induction of the 2nd isoform (COX-2). Inhibition of COX-1 is responsible for their GIT toxicity. Inhibition of COX-1 exerted antiplatelet activity Inhibition of COX-2 is responsible for the antiinflammatory effect of NSAIDs. COX (cont’d) Selective COX-2 inhibitors. Have similar efficacies to that of the non- selective inhibitors, but the GIT side effects are decr by ~50%. But, no cardioprotection and there is actually increased MI. THERAPEUTIC USES Fever (non-specific). Analgesic (headache, toothache, myalgia and arthralgia). Common cold (lowers fever and relieves headache and muscle aches). Rheumatoid arthritis . Acute rheumatic fever Reducing the risk of myocardial infarction. Aspirin in low dose (75- 150 mg/ day or lower) inhibits platelet aggregation i.e. antithrombotic. CLASSIFICATION OF NSAIDS Non-selective COX inhibitors Selective COX-2 inhibitors Classification of NSAIDs: Non-selective COX inhibitors: These NSAIDs inhibit the constitutive COX- 1 and the inducible COX-2 so are liable to be associated with GIT upset and renal impairment on long term use. This group is further classified according to chemical structure into: Salicylates e.g. acetyl salicylic acid, sodium salicylate Other NSAIDs: Propionic acid derivatives e.g. Ibuprofen and naproxen. Oxicams Aryl acetic acid derivatives e.g. Diclofenac. Indole derivatives e.g. Indomethacin and sulindac. Selective COX-2 inhibitors: Celecoxib, etoricoxib, valdecoxib – selective COX-2 inhibitors. Have similar efficacies to that of the non-selective inhibitors, but the GIT side effects are decr by ~50%. But, no cardioprotection and there is actually increased MI. Mechanism of action of NSAIDs: Acetyl salicylic acid, the prototype of NSAIDs induces irreversible inhibition of both COX-1 and COX-2 enzymes. This inhibit conversion of arachidonic acid to PG and TXA2. Other NSAIDs cause competitive reversible inhibition of COX enzymes. Celecoxib is a selective COX-2 inhibitor. The Salicylates - Aspirin Duration of action ~ 4 hr. Orally Weak acid so, non-ionized in stomach easily absorbed. Pharmacological Actions of Salicylates Analgesic action Salicylates act on subcortical level to produce their analgesic action: By raising the threshold to painful stimuli. Through its anti-inflammatory action because inflamed tissue will stimulate the pain receptors. Antipyretic action Salicylates lower the elevated body temperature to normal by: Inhibiting prostaglandin synthesis (centrally). Acting on heat regulating center in the hypothalamus promoting loss of heat by: Vasodilatation of cutaneous blood vessels stimulating radiation. Increasing sweating and evaporation. Anti-inflammatory and anti-rheumatic action Relieves muscular pain. Relieves joint pain and swelling. through decreasing the synthesis of prostaglandins. On the G.I.T. Salicylates irritate gastric mucosa leading to nausea and vomiting. Central due to stimulation of CTZ. Peripheral due to irritation of gastric mucosa by the released salicylic acid. Higher doses may cause: Gastric ulceration, and bleeding. Effect on the blood Inhibits platelet aggregation secondary to inhibition of platelet COX and reduces production of TXA2 (a platelet aggregating factor) with prolongation of bleeding time. Large doses lead to hypoprothrombinaemia and prolongation of coagulation time. This effect is reversed by vitamin K. Uricosuric action Small doses: (less than 5 g /day) depress uric acid secretion by proximal tubules causing uric acid retention. Large doses: (greater than 5 g/day) inhibit the renal reabsorption by proximal tubules, increasing uric acid excretion, decreasing its plasma level thus producing uricosuric action. This effect is enhanced if the urine is made alkaline. Side effects Gastric irritation, N&V , gastric ulceration, bleeding Hypersensitivity; Bronchoconstriction, Urticaria. Mechanism: by inhibiting COX enzyme, therefore arachidonic acid will be acted upon by lipo-oxygenase enzyme increasing leukotrienes (powerful bronchoconstrictor). Salicylism Salicylism: (occurs after repeated administration of large doses of salicylates as in rheumatic fever and gout). Its symptoms are: Headache Mental confusion, Ringing in the ears Visual disturbances Sweating Nausea, vomiting and diarrhea Disappear after stoppage of the drug Contraindications of Salicylates: Patients with peptic ulcer. Patients having hypersensitivity reactions to salicylates. Bleeding tendency. Patients taking anti-coagulants. Gout: in small dose. Viral infections in children Other NSAIDs Ibuprofen: Effective and better tolerated (less side effects). First choice in inflammatory joint diseases. Naproxen: Related to ibuprofen. More potent. Moderate risk of side effects, longer acting Diclofenac: (Voltaren) It is very potent used in: Rheumatoid arthritis and osteoarthritis Renal colic and postoperative pain Indomethacin (Indocid) Potent, but due to its serious side effects, its use is limited Selective COX-2 Inhibitors Celecoxib: It is a selective COX-2 inhibitor that spares COX-1, thus it does not inhibit synthesis of protective PGs in the gut. Hence, its anti-inflammatory effect is associated with less GI adverse effects. Paracetamol It is an analgesic-antipyretic with no anti- inflammatory action. It effectively inhibits PG synthesis in the CNS resulting in analgesic and antipyretic effects but it is a weak PG inhibitor in peripheral tissue. It has no anti-inflammatory effect. A commonly used analgesic antipyretic instead of aspirin in cases of: Peptic or gastric ulcers. Bleeding tendency. Allergy to salicylates. Viral infections in children (to avoid Reye syndrome). Pregnancy. Reye syndrome is sudden (acute) brain damage and liver function problems of unknown cause. The syndrome has occurred in children who have been given aspirin when they have chicken pox or the flu. Reye syndrome has become very uncommon since aspirin is no longer recommended for routine use in children. Toxicity Skin rash. Liver damage (with over dosage). NB. In case of acute paracetamol poisoning, N-acetyl cysteine is a specific antidote and should be given as early as possible (it contains -SH group) Thank you