* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Analgesia and Asthma
Discovery and development of direct thrombin inhibitors wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Pharmacognosy wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Prescription costs wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Drug interaction wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Neuropharmacology wikipedia , lookup
Psychopharmacology wikipedia , lookup
Theralizumab wikipedia , lookup
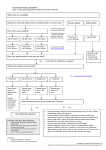
NAPLEX Analgesics PG 132 Treatment Algorithm for Pain Patient in pain Rating Scale 0-10 Mild Pain (0-3) NSAID, aspirin, APAP Moderate Pain (4-6) Weak opioid: codeine, hydrocodone Severe Pain (7-10) Strong opioid: morphine, oxycodone, hydromorphone Treating Specific Types of Cancer Pain Bone pain NSAIDs, bisphosphonates, corticosteroids, opiates Visceral pain NSAIDs, opiates Neuropathic pain TCAs, gabapentin, carbamazepine, corticosteroids Muscle spasms Benzodiazepines, baclofen Non Opioid Analgesics Drug Dose Interval Renal Adjustment Hepatic Adjustment Acetaminophen 500-1000 mg 4-6 hours GFR: >50 ml/min q4h, 10-50 ml/min q6h, <10 ml/min q8h 1/2 life is increased, Can be given safely Max: 4 g Aspirin 500- 1000 mg Max: 4 g 4-6 hours Avoid Avoid Celecoxib 100-200 mg Max: 800 mg 12 hours Avoid Decrease dose by 50 % Rofecoxib (off market) 12.5 mg-25 mg Max: 50 mg Daily Avoid Avoid Valdecoxib (off market) 10-20 mg Max: 40 mg Daily Avoid Avoid PG 134 Non Opioid Analgesics con’t Drug Dose Interval Renal Adjustment Hepatic Adjustment Ibuprofen 200-800 mg 4-6 hours Use with caution Contraindicated in renal failure No dose alterations, Kinetics minimally effected Max: 3.2 g/day Naproxen 550 mg initial, 250 subsequent Max: 1.5g/day 6-8 hours Use with caution Reduce dose 50% Indomethacin 25 mg Max: 200mg/day 8-12 hours Use with caution Avoid Ketoralac 30 mg or 60 mg IM Max: 5 days of combine treatment (IM & PO) 6 hours Avoid Avoid Propionic Acids oxaprozin naproxen ibuprofen ketoprofen fenoprofen flurbiprofen Naphthylalkanone Carboxylic Acids Nonacetylated Salicylates Oxicams salsalate diflunisal choline piroxicam meloxicam nabumetone Fenamates meclofenamate mefenamic acid GI Sparing Agents diclofenac/misoprostol Salicylates ASA Acetic Acids sulindac etodolac indomethacin tolmetin diclofenac ketorolac Weak Opioid Analgesics Drug Dose Interval Codeine 15-60 mg Max: 120 mg 4-6 hours Oxycodone w/ -acetaminophen -aspirin 5 mg Max: 4 g* Hydrocodone w/ -ibuprofen (7.5/200) -acetaminophen (5/500) -aspirin (5/500) 1-2 tabs Max: 5 tabs 4-6 hours 1-2 tabs Max: 4 g* 1-2 tabs Max: 4 g* 4-6 hours Tramadol 50-100 mg Max: 400mg 2 tabs Max: 8 tabs 4-6 hours -acetaminophen (37.5/325) 4-6 hours Renal Adjustment Hepatic Adjustment CrCl: 10-50 ml/min=75% of dose, <10 ml/min=50% of dose A dosage adjustment decrease Be conservative, drug levels increase by 50% 1/3 to 1/2 of usual dose, Elimination 1/2 life increase by 2.3 hours Use cautiously in mild to moderate renal failure, avoid in severe renal failure Avoid CrCl < 30 ml/min increase dosing interval to q12h with a max of 200 mg per day Cirrhosis 50 mg q12h 4-6 hours 4-6 hours Avoid Weak Opioid Analgesics con’t Drug Propoxyphene -acetaminophen -aspirin Dose 1-2 tabs Max: 4 g* 1-2 tabs Interval Renal Adjustment Hepatic Adjustment Avoid 4 hours Don’t give in severe renal failure, use cautiously in mild and moderate renal failure 4 hours Strong Opioid Analgesics Drug Dose Interval Renal Adjustment Hepatic Adjustment Meperidine - Binds opiate receptors 50 - 150 mg 3-4 hours GFR >50 ml/min No adjustment 10-50 ml/min 75% of dose <10 ml/min 50% of dose Decrease dose, 1/2 life is increased Titrate to response 2-6 hours GFR >50 ml/min No adjustment 10-50 ml/min 75% of dose <10 ml/min 50% of dose 1/2 life prolonged increase interval by 1.5 to 2 times Morphine (gold standard) -immediate release -IV, IM, SQ, continuous infusion -epidural -intrathecal Metabolite accumulation (normeperidine) Anxiety, agitation, tremor &/or seizures 10-30 mg 2.5-20 mg 0.8 to 10 mg/hr Max: 80 mg/hr 5mg bolus, redose 1 hr 1 to 2 mg Max: 10 mg/24 hr 0.2 to 1 mg -rectal 10-20 mg No repeat dose 4 hours (morphine-6-glucuronide) accumulates in renal failure Strong Opioid Analgesics con’t Drug Hydromorphone -PO, IM, IV, SQ -rectal Oxycodone - percocet (APAP) - percodan (ASA) Methadone -PO, IM, SQ -IV Dose Interval Renal Adjustment Hepatic Adjustment Decrease dose 1-4 mg 3 mg 4-6 hours 6-8 hours 5 mg May titrate to response – no maximum dose 6 hours – 2.5-10 mg Max:1000 mg 0.1mg/kg 3-8 hours 4 hrs x 3 doses then 6-12 hours Be conservative, drug levels increase by 50% 1/3 to 1/2 of usual dose, Elimination 1/2 life increase by 2.3 hours GFR >50ml/min q6h 10-50 ml/min q8h <10 ml/min q12h No Change in dose mild to moderate disease, Avoid in severe liver disease CrCl <10 ml/min 50-75% dose Strong Opioid Analgesics con’t Drug Fentanyl -transdermal -transmucosal -Parenteral Dose Initial 25 mcg/hr Initial 200 mcg Interval Renal Adjustment Hepatic Adjustment 72 hours 30 min CrCl 10-50 ml/min 75% of dose <10 ml/min 50% of dose Unaffected by cirrhosis, effected by hepatic blood flow Remind patients that heat can increase fentanyl absorption. Warn against extended exposure of the patch to heating pads, hot tubs, sunbathing, high fever, etc. Opioid Equianalgesic Dosing Drug Oral (mg) Parenteral (mg) Morphine 30 10 Hydromorphone 7.5 1.5 Oxycodone 20-30 10-15 Methadone 10-20 acute? 2-4 chronic 4 acute 1 chronic x 10 acute? 2-4 chronic 2 acute 1 chronic 0.1-0.2 x 1 300 75 Levorphanol Fentanyl Oxymorphone Meperidine Morphine Analogs---table 2-28, pg.132 General properties CNS depression Respiratory depression Reduce propulsive activity of the gut Urinary retention Toxicity causes pinpoint pupils No maximum dose Meperidine Analogs---See Table 2-28, pg.132 General properties Good analgesic (parenteral) Less CNS depression or constipation than opiates Spasmolytic action - may be useful for pain related to uterus, GI, bronchi, etc. Combination with hydroxyzine or promethazine permits 25–50% dosage reduction Principal drugs Meperidine (Demerol)---accumulates in renal disease, metabolite can cause siezures Diphenoxylate + atropine (Lomotil) – C-V - antidiarrhea - subtherapeutic dose of atropine to prevent abuse Drugs for Migraine Headache Types - Tension, Cluster, Migraine - Migraine is unilateral, pulsating, throbbing, with or w/o aura, nausea, photophobia, sonophobia Treatments – Prophylactic and Abortive Abortive Aspirin - analgesic, antipyretic, anti-inflammatory, anti-platelet Acetaminophen—analgesic, antipyretic NSAIDs - analgesic, antipyretic, anti-inflammatory (See Table pg. 133) • Mechanism of action • Common adverse effects: GI toxicity, hypersensitivity, renal effects PG 133 Contraindications to the use of Imitrex include which of the following: I. uncontrolled HTN II. use of and MAOI within the past 2 weeks III. ischemic heart disease a. I only b. III only c. I and II only d. II and III only e. I, II, and III Contraindications to the use of Imitrex include which of the following: I. uncontrolled HTN II. use of and MAOI within the past 2 weeks III. ischemic heart disease a. I only b. III only c. I and II only d. II and III only e. I, II, and III Drugs for Migraine Abortive - (cont.) Dihydroergotamine (Migranal) - nasal spray; dose may be repeated after 15 min – MOA – blocks alpha adrenergic causing vasoconstrition 5-HT1D Receptor Agonists - avoid in patients with cardiovascular disease • Almotriptan (Axert) • Eletriptan (Relpax) – tablets; newest agent on the market – another “me-too” • Frovatriptan (Frova) – tablets; longest half life among agents • Naratriptan (Amerge) - tablets • Rizatriptan (Maxalt) - tablets; also Maxalt MLT (oral disintegrating tab) • Sumatriptan (Imitrex) - injection, tablet, nasal spray • Zolmitriptan (Zomig) - tablets; also Zomig ZMT (oral disintegrating tab) PG 132 Drugs for Migraine Prophylactic Therapy - Given to patients with >2-3 HA/month, severe HA, ineffective treatment Drugs of Choice: - propranolol (Inderal) – use if patient also has HTN - amitriptyline (Elavil) – concomitant depression - valproate (Depakote) - concomitant seizures Other agents: - verapamil, topiramate PG 133 Pathophysiology Complications Source: www.arava.com Rheumatoid Arthritis Corticosteroids – early, acute, not long-term - also NSAIDs / COX-2 Inhibitors Disease Modifying Antirheumatic Drugs (DMARDs) – liver, heme Auranofin (Ridaura) Gold Aurothioglucose (Solganol) Azathioprine (Imuran) Cyclophosphamide (Cytoxan) Cyclosporine (Neoral, Sandimmune) Gold sodium thiomalate (Myochrysine) Hydroxychloroquine (Plaquenil) – retinal toxicity – Q 6 months Methotrexate (Rheumatrex) Leflunomide (Arava)---Preg Cat X, long half-life, hepatotoxic Penicillamine (Cuprimine, Depen) Sulfasalazine (Azulfindine) – orange-yellow urine PG 134 Biologic Response Modifiers Etanercept (Enbrel) – avoid with live vaccine (soluble receptor TNF inhibitor) Anakinra (Kineret) – monitor for pulmonary problems (IL-1 receptor antagonist) Infliximab (Remicade) – monitor for infection (monoclonal antibody for TNF) Adalimumab (Humira) – monitor for infection (monoclonal antibody for TNF receptor) Abatacept (Orencia®) – monitor for infection (Inhibits T-Cell (Tlymphocytes activation by binding to CD80 and CD86 on antigen presenting cells) Osteoarthritis (OA) - acetaminophen & NSAIDs - surgery – knee/hip replacement - glucosamine/chondrotin – NIH study (GAIT) PG 134 Joint Distribution: RA Compared to OA Rheumatoid Arthritis Osteoarthritis SLE (systemic lupus erythematosus) occurs more frequently in: a. male African Americans b. Asians c. post-menopausal women d. people of Mediterranean origin e. young women SLE (systemic lupus erythematosus) occurs more frequently in: a. male African Americans b. Asians c. post-menopausal women d. people of Mediterranean origin e. young women Patients who are life time smokers have the greatest risk of leg pain associated with? a. hypokalemia b. rhabdomylosis c. intermittent claudication d. dopamine deficiency e. myocardial infarction Patients who are life time smokers have the greatest risk of leg pain associated with? a. hypokalemia (cramps) b. rhabdomylosis (statins) c. intermittent claudication (PVD) d. dopamine deficiency (RLS) e. myocardial infarction Trigeminal neuralgia is treated by the use of: a. aspirin b. carbamazepine c. dipyridamole d. methylprednisolone e. thiamine Trigeminal neuralgia is treated by the use of: a. aspirin b. carbamazepine c. dipyridamole d. methylprednisolone e. thiamine When dispensing a prescription for Robitussin AC, the pharmacist should attach label(s) indicating: I. May cause drowsiness II. Shake well before using III. Finish all of this medication a. I only b. III only c. I and II only d. II and III only e. I, II, and III When dispensing a prescription for Robitussin AC, the pharmacist should attach label(s) indicating: I. May cause drowsiness II. Shake well before using III. Finish all of this medication a. I only b. III only c. I and II only d. II and III only e. I, II, and III Which of the following is/are appropriate warning(s) for the use of Duragesic transdermal system patches? I. Do not cut patches before applying II. Not intended for use in children under the age of 12 III. Replace patch every day unless pain is under control a. I only b. III only c. I and II only d. II and III only e. I, II, and III Which of the following is/are appropriate warning(s) for the use of Duragesic transdermal system patches? I. Do not cut patches before applying II. Not intended for use in children under the age of 12 III. Replace patch every day unless pain is under control a. I only b. III only c. I and II only d. II and III only e. I, II, and III The upper daily dosing regimen for naproxen is NOT more than: a. 0.5 g b. 1 g c. 1.5 g d. 2.5 g e. 4 g The upper daily dosing regimen for naproxen is NOT more than: a. 0.5 g b. 1 g (mefenamic) c. 1.5 g (naproxen) d. 2.5 g e. 4 g (acetaminophen) Ibuprofen (3.2g) Indomethacin (200mg) Which of the following ingredients is are present in Percodan but not in Percocet: I. Aspirin II. Acetaminophen III. Oxycodone a. I only b. III only c. I and II only d. II and III only e. I, II, and III Which of the following ingredients is are present in Percodan but not in Percocet: I. Aspirin II. Acetaminophen III. Oxycodone a. I only b. III only c. I and II only d. II and III only e. I, II, and III NAPLEX Drugs for the Treatment of Asthma PG 142 Classification Symptoms Step 1 Mild Intermittent ¨ Symptoms ≤ 2 times a week ¨ Asymptomatic and normal PEF between exacerbations ¨ Exacerbations brief (from a few hours to a few days); intensity may vary Step 2 Mild Persistent ¨ Symptoms > 2 times a week but < 1 time a day ¨ Exacerbations may affect activity Step 3 Moderate Persistent ¨ Daily symptoms ¨ Daily use of inhaled shortacting beta-2 agonist ¨ Exacerbations affect activity ¨ Exacerbations ≥ 2 times a week; may last day Step 4 Severe Persistent ¨ Continual Symptoms ¨ Limited Physical Activity ¨ Frequent Exacerbations Nighttime Symptoms ≤ 2 times a month > 2 times a month Lung Function ¨ FEV1/PEF ≥ 80% predicated ¨ PEF variability < 20% ¨ FEV1/PEF ≥ 80% predicated ¨ PEF variability < 2030% > 1 time a week ¨ FEV1/PEF > 60 - < 80% predicated ¨ PEF variability > 30% Frequent ¨ FEV1/PEF ≤ 60% predicated ¨ PEF variability > 30% Drugs for the Treatment of Asthma phosphodiesterase Adenyl cyclase cyclic AMP (bronchodilation) elimination Sympathomimetics Increase formation of cyclic AMP Nonselective • Ephedrine • Epinephrine (Adrenalin, Medihaler-Epi, Bronkaid, Primatene, etc.) • Ethylnorepinephrine (Bronkephrine) PG 142 Drugs for the Treatment of Asthma Selective Short-Acting Beta-2 Agonists. Provide quick relief; may cause tachycardia, tremor, etc. • Albuterol (Proventil, Ventolin, Airet, Volmax) 0.5hr peak, 4 hours duration • Albuterol - oral sustained-release product • Pirbuterol (Maxair) – Autoinhaler – longer duration 6 hrs (tertiary butyl group) • Levalbuterol (Xopenex) – active isomer of albuterol, neb., less cardiac side effects • Metaproterenol (Alupent, Metaprel) – delayed onset (1 hour) & prolonged effect (4 hour) • Terbutaline (Brethine, Bricanyl) – delayed onset 1 hour & prolonged duration (6hr) – no-inhalation in U.S. & (management of pretermed labor) • isoproterenol (Isuprel, Medihaler-Iso) – beta-1 & beta-2 activity PG 143 Drugs for the Treatment of Asthma (cont.) Long-Acting Beta-2 Agonists. For long-term symptom control; frequently used with inhalational corticosteroids; may cause tachycardia, tremor, etc.; for prophylaxis only. • Formoterol (Foradil) – DPI - capsule • Salmeterol (Serevent) – DPI – Diskus NOT SUITABLE AS A RESCUE INHALER!!!!!!!!!!!!!! PG 142 Drugs for the Treatment of Asthma Xanthines Phosphodiesterase inhibitors; generally for prophylaxis; adverse effects similar to caffeine • Theophylline (Slo-Phyllin, Theolair, Theo-Dur)----Think drug interactions, serum levels 10-20, arryhthimogenic at high levels • Dyphylline (Lufyllin).theophylline derivative • Aminophylline (Somophyllin-CRT).anhydrous contains 86% - 300mg theo (PO) = 380mg Amino (IV) theophylline, dihydrate 79% • Oxtriphylline (Choledyl).contains 64% theophylline Leukotriene receptor drugs For prophylaxis; may reduce need for beta-2 agonist • Zafirlukast (Accolate).leukotriene receptor antagonist • Montelukast Sodium (Singulair).leukotriene receptor antagonist • Zileuton (Zyflo).inhibits leukotriene formation (5-lipoxygenase inhibitor); PG 142 monitor hepatic function, think DIs---potent inhibitor Zyflo CR will be given BID instead of QID. But patients will still need liver function tests every month for the first 3 months...then every 2 to 3 months for the rest of the first year. – 2007 Omalizumab. Save the monoclonal antibody, Xolair, for patients with severe asthma and allergies...who are not responding adequately to high-dose inhaled steroids and long-acting betaagonists. New NIH guidelines will improve asthma treatment. You'll see renewed emphasis on controlling symptoms...patient education...and avoiding allergens. Drugs for the Treatment of Asthma Corticosteroids Inhalational; reduce inflammation and bronchial reactivity; may cause oral candidiasis, cough, and other steroid effects (with prolonged use). Prophylaxis only. • Beclomethasone dipropionate (Beclovent, Vanceril) • Triamcinolone acetonide (Azmacort) • Flunisolide (Aerobid) • Fluticasone propionate (Flovent) • Mometasone (Asmanex Twisthaler) • Budesonide (Pulmicort) (Pulmicort Respules – only neb ICS) Anticholinergics Ipratropium bromide (Atrovent); bronchodilator. Reduces secretions; alternative to beta-2 agonists; anticholinergic adverse effects - combivent – albuterol and ipratropium PG 142 Tiotropium (Spiriva)----long acting, dry powder capsule for inhalation Drugs for the Treatment of Asthma Mast cell stabilizers Anti-inflammatory; very safe; for prophylaxis only • Cromolyn sodium (Intal, Nasalcrom) • Nedocromil sodium (Tilade) Combination products Ipratropium bromide/albuterol sulfate (Combivent) Salmeterol xinafoate/fluticasone propionate (Advair Diskus) Symbicort contains the corticosteroid budesonide (Pulmicort)...plus the long-acting beta-agonist formoterol (Foradil). - 2007 - 2 puffs BID PG 143 Side effects of oral corticosteroids include all of the following except: a. hyperglycemia b. nervousness c. fluid retention d. HPA axis suppression e. thrombocytopenia Side effects of oral corticosteroids include all of the following except: a. hyperglycemia b. nervousness c. fluid retention d. HPA axis suppression e. thrombocytopenia Patients exhibiting Cushing syndrome should avoid products containing: a. corticosteriods b. iodine c. sulfas d. penicillins e. salicylates Patients exhibiting Cushing syndrome should avoid products containing: a. corticosteriods b. iodine c. sulfas d. penicillins e. salicylates Which of the following drugs is/are administered by dry powder inhalation? I. Ipratropium (atrovent of combivent) II. Pirbuterol (MaxAir Turboinhaler) III. Salmeterol (Diskus) a. I only b. III only c. I and II only d. II and III only e. I, II, and III Which of the following drug(s) is/are administered by dry powder inhalation? I. Ipratropium (atrovent of combivent) II. Pirbuterol (MaxAir Turboinhaler) III. Salmeterol (Diskus) a. I only b. III only c. I and II only d. II and III only e. I, II, and III All of the following drugs are available as aerosol units EXCEPT: a. Spiriva b. Azmacort c. Rhinocort d. Beconase e. Combivent All of the following drugs are available as aerosol units EXCEPT: a. Spiriva b. Azmacort c. Rhinocort d. Beconase e. Combivent NAPLEX Drugs Used to Treat Glaucoma Causes of Glaucoma • Wide or open angle – most common, malfunction of trabecular meshwork • Narrow angle or closed angle – obstruction of the outflow of aqueous humor through the trabecular meshwork. PG 136 An instrument used to measure intraocular pressure is a(n): a. gonioscope b. otoscope c. ophthalmoscope d. tonometer e. barometer An instrument used to measure intraocular pressure is a(n): a. gonioscope (lens to study angle of eye) b. otoscope (instrument to examine the drum membrane of the ear) c. ophthalmoscope (device to study interior of eye) d. tonometer (device to measure intraocular pressure) e. barometer (device to measure the atmospheric pressure) Drugs for Glaucoma Treatment Goal of Therapy – reduced intraocular pressure (IOP) - measured by a tonometer (10-20mmhg) - decrease rate of aqueous humor production - increase rate of outflow (drainage) of aqueous humor Sympathomimetics— increase outflow and decrease production of aqueous humor - epinephrine (Epifrin, Glaucon) – discard if color change occurs - dipiverfrin (Propine) – epinephrine prodrug – less side effects - apraclonidine (Iopidine) – alpha-2 agonist; watch for ocular allergy - brimonidine (Alphagan) - alpha-2 agonist, more selective PG 136 Drugs for Glaucoma Treatment mydriasis Miotics (direct acting)—have direct cholinergic action causing miosis; increases outflow, may cause eye pain, burning, blurred vision; less with gel and Ocusert formulations - acetylcholine (Miochol) - carbachol (Isoptocarbachol) - Pilocarpine (Isoptocarpine, Pilocar, Pilostat, Pilopine HS, Ocusert Pilo) Miotics (cholinesterase inhibitors)—increase cholinergic action by inhibiting cholinesterase; similar adverse effects as direct-acting miotics - physostigmine (Eserine) – may cause cataracts - Demecarium (Humersol) - Echothiophate (phospholine iodide) PG 136 Drugs for Glaucoma Treatment Beta-adrenergic blocking agents — reduce production of aqueous humor; watch for possible breathing difficulty, bradycardia, hypotension, and CNS depression - betaxolol (Betopic, Betoptic S) – beta 1 selective - levobetaxolol (Betaxon) – beta 1 selective - carteolol (Ocupress), levobunolol (Betagan, AKBeta) - metipranolol (Optipranolol), - timolol (Timoptic, Timoptic XE) B1 & B2 Prostaglandin analogs — increase outflow of aqueous humor; may darken iris color and cause thickened lashes - latanoprost (Xalatan) - bimatoprost (Lumigan) - travoprost (Travatan) - Unoprostone (Rescula) Not available in U.S. PG 136 Drugs for Glaucoma Treatment Carbonic anhydrase inhibitors — suppress production of aqueous humor; watch for urinary frequency and nephrolithiasis - dichlorphenarnide (Daranide) - acetazolamide (Diamox)----oral capsules, IV – Also used for mountain sickness - methazolamide (Neptazane) - dorzolamide (Trusopt) - brinzolamide (Azopt) Osmotic diuretics----given orally or IV - glycerin (Osmoglyn) , mannitol (Osmitrol) - urea (Ureaphil), isosorbide (Isomotic) PG 136 Timoptic dosage forms include: I. capsule II. tablet III. ophthlamic solution a. I only b. III only c. I and II only d. II and III only e. I, II, and III Timoptic dosage forms include: I. capsule II. tablet III. ophthlamic solution a. I only b. III only c. I and II only d. II and III only e. I, II, and III Dosage forms for timolol maleate include: I. gel II. tablet III. ophthlamic solution a. I only b. III only c. I and II only d. II and III only e. I, II, and III Dosage forms for timolol maleate include: I. gel II. tablet III. ophthlamic solution a. I only b. III only c. I and II only d. II and III only e. I, II, and III Glaucoma Case Study Page 138 Pilocarpine can be classified as a(n): a. anticholinergic agent b. carbonic anhydrase inhibitor c. beta-adrenergic blocking agent d. cholinergic agent e. sympathomimetic agent Pilocarpine can be classified as a(n): a. anticholinergic agent b. carbonic anhydrase inhibitor c. beta-adrenergic blocking agent d. cholinergic agent e. sympathomimetic agent An Ocusert Pilo-20 system: a. is administered orally once daily b. releases 20 mg of pilocarpine each day c. must be replaced each month d. releases 20 µg of pilocarpine each hour e. must be soaked in normal saline just prior to use An Ocusert Pilo-20 system: a. is administered orally once daily b. releases 20 mg of pilocarpine each day c. must be replaced each month d. releases 20 µg of pilocarpine each hour e. must be soaked in normal saline just prior to use A normal intraocular pressure reading would be: a. 10-20 mm Hg b. 20-30 mm Hg c. 30-40 mm Hg d. 40-50 mm Hg e. 50-60 mm Hg A normal intraocular pressure reading would be: a. 10-20 mm Hg b. 20-30 mm Hg c. 30-40 mm Hg d. 40-50 mm Hg e. 50-60 mm Hg Special caution must be used when timolol is used in patients with: a. sulfonamide allergy b. asthma c. cancer d. hypertension e. NSAID hypersensitivity Special caution must be used when timolol is used in patients with: a. sulfonamide allergy b. asthma c. cancer d. hypertension e. NSAID hypersensitivity