* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download anemia: symptoms - Oregon Health & Science University
Coronary artery disease wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Discovery and development of direct Xa inhibitors wikipedia , lookup
Atrial fibrillation wikipedia , lookup
History of invasive and interventional cardiology wikipedia , lookup
Discovery and development of direct thrombin inhibitors wikipedia , lookup
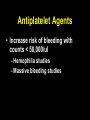
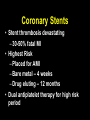
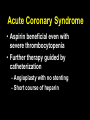
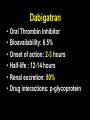
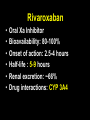
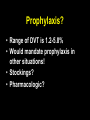
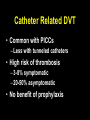
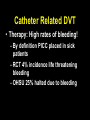
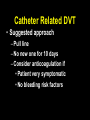
Thrombosis Update Tom DeLoughery MD FACP FAWM Oregon Health and Sciences University DISCLOSURE Current Relevant Financial Relationship(s) Speaker Bureau – None What I am Talking About • • • • Antiplatelet agents Antithrombotics Atrial fibrillation Venous thrombosis Anticoagulation • Patients with hematological malignancies not immune to thrombosis • DVT 3-5% – Line – 3-15% • PICC > Central • Coronary artery disease: – 45-64: 5% – > 65: > 15% Issues • Antiplatelet agents • Antithrombotic – Atrial fibrillation – Valves – Venous thrombosis Antiplatelet Agents • Increase risk of bleeding with counts < 50,000/ul – Hemophilia studies – Massive bleeding studies MI: Primary and Secondary Prevention • Primary prevention – Minimal short term effect – Halt aspirin for duration • Secondary prevention – 22% reduction in new events – Stop and restart at 50,000/ul Coronary Stents • Stent thrombosis devastating – 30-50% fatal MI • Highest Risk – Placed for AMI – Bare metal – 4 weeks – Drug eluting – 12 months • Dual antiplatelet therapy for high risk period Drug Eluting Stents • Drugs inhibits restenosis by inhibiting cell proliferation • Inhibits endothelialization of stent • Increasing reports of late thrombosis even 18 months Stent Management • Outside “risk period” – Bare Metal > 4 weeks – Drug eluting > 12 months • Aspirin until platelets < 20,000/uL Stent Management • Risk Period – Bare metal < 4 weeks – Drug eluting < 12 months • Cardiology input • Continue dual antiplatelet therapy unless severe bleeding Acute Coronary Syndrome • Aspirin beneficial even with severe thrombocytopenia • Further therapy guided by catheterization – Angioplasty with no stenting – Short course of heparin Antithrombotic Therapy • UF Heparin – Short T1/2 0.5-1 hours • LMWH – Longer T1/2 4 hours – Reversible by protamine – Need to adjust for renal disease • Fondaparinux – Longest T1/2 17-19 hours – Not reversible by protamine – Contraindicated in renal failure General LMWH Plan • Change warfarin patients to LMWH • Continue full dose until platelets <50,000/uL • “Prophylactic” dose until platelet <20,000/uL – Enoxaparin 40mg/day – Several studies have shown this dose effective for treatment Dabigatran • • • • • • Oral Thrombin Inhibitor Bioavailability: 6.5% Onset of action: 2-3 hours Half-life : 12-14 hours Renal excretion: 80% Drug interactions: p-glycoprotein Dabigatran: Bottom Line • Superior to warfarin in stroke prevention • GI side effects 15% • 1.3x increase risk of MI – outweighed by benefit • CrCl > 50 • Effects aPTT Drug Interactions • Contraindicated – Dronedarone, azoles, rifampin, St John’s wort, carbamazepine • Caution with renal disease or use of multiple of these drugs – Verapamil, amiodarone, quinidine, clarithromycin Rivaroxaban • • • • • • Oral Xa Inhibitor Bioavailability: 80-100% Onset of action: 2.5-4 hours Half-life : 5-9 hours Renal excretion: ~66% Drug interactions: CYP 3A4 Rivaroxaban • Approved 10mg daily for DVT prophylaxis in TKR and THR • Approved 20mg daily for afib – 15mg if CrCl 15-50mL/m – Contraindicated < 15mL/m • Approved for DVT – 15mg BID x 3 weeks – 20mg daily Drug interactions • Ketoconazole, itraconazole, lopinavir/ritonavir, ritonavir, indinavir/ritonavir, and conivaptan • Potential with renal insufficiency – CSA, Erythromycin, azithromycin, diltiazem, verapamil, quinidine, ranolazine, dronedarone, amiodarone, and felodipine Rivaroxaban: Bottom Line • • • • • Effective in stroke prevention Superior in prevention of VTE Safer in treatment of VTE CrCl > 15 (15mg < 50) Once a day drug – BID x 3 weeks in acute VTE • INR to monitor Apixaban • • • • • • Oral Xa Inhibitor Bioavailability: 66% Onset of action: 1-3 hours Half-life : 8-15 hours Renal excretion: 25% Drug interactions: CYP 3A4 – Multiple other pathways Drug interactions • Ketoconazole, itraconazole, clarithromycin, lopinavir/ritonavir, ritonavir, indinavir/ritonavir, and conivaptan – Cut to 2.5 mg BID • Avoid due to decrease effect – Carbamazepine, phenytoin, rifampin, St. John’s wort Apixaban: Bottom Line • Superior in stroke prevention with less bleeding • Superior in prevention of VTE • Safer in therapy of VTE • BID drug • CrCl > 15 • Does not effect INR/PTT Comparing Trials Atrial Fibrillation Drug Stroke Bleeding Apixaban Better Safer Dabigatran Better Equal Rivaroxaban Equal Equal Warfarin: $4/month + monitoring ($20-50/visit) Apixaban: $320/month Dabigatran: $235/month Rivaroxaban: $247/month ICH – Atrial Fibrillation Stroke Intracranial Hemorrhage Events/ 100 years RR Events/ 100 years RR Dabigatran 110 1.53 0.91 (0.74-1.11)) 0.23 0.31 (0.20-0.47) Dabigatran 150 1.11 0.66 (0.53-0.82) 0.30 0.40 (0.27-0.60) Rivaroxaban 1.76 0.79 (0.66-0.96) 0.49 0.67 (0.47-0.94) Apixaban 1.19 0.79 (0.65-0.95) 0.33 0.42 (0.30-0.58) Potential for 10-12,000 less ICH in USA Atrial Fibrillation • Dabigatran – Robust trial data for all CHADS2 • Apixaban – More effective than warfarin – Better in patients at risk for bleeding – Safer – “the sweet spot” • Rivaroxaban – Effective Venous Thrombosis Drug Thrombosis Bleeding Apixaban Equal Safer Dabigatran Equal Equal Rivaroxaban Equal Safer Warfarin: $4/month + monitoring ($20-50/visit) LMWH: $100-120/day Apixaban: $320/month Rivaroxaban: $247/month Dabigatran: $235/month Venous Thrombosis • Rivaroxaban – FDA approved – Cost effective for acute DVT – Safer • Dabigatran with robust data – Two trials and extended therapy • Apixaban – Effective and safer DVT treatment Reversal • Drugs we have no antidote for: – Low molecular weight heparin, fondaparinux, aspirin, clopidogrel, ticagrelor, prasugrel, dabigatran, rivaroxaban, apixaban What We Do • Life or limb threatening bleeding • 50 units/kg of 4 factor PCC (kcentra) Atrial Fibrillation • Leading indications for warfarin anticoagulation • Warfarin reduced risk of stroke from 5%/yr to 1%/yr • Risk predicated by CHADS2 score CHADS2 CHADS2 Score 0 Stroke/yr Risk Level 1.9 Low 1 2.8 Low/moderate 2 4.0 Moderate 3 5.9 Moderate 4 8.5 High 5 12.5 High 6 18.2 High Management • CHAD2 <1: nothing • >1: LMWH protocol or new anticoagulant • Highest risk – Previous stroke – CHADS2>4 – Cardiac thrombus Cardiac Valves • Bioprosthetic – Asprin until platelets < 50,000/uL • Mechanical – New drugs absolutely contraindicated!!! – Aortic bileaflet – LMWH protocol – Higher risk • Monitored LMWH • Continue until platelets < 30,000/uL –Prophylactic throughout Venous Thrombosis • On anticoagulants • > 3 months since thrombosis – Hold anticoagulation – Prophylaxis • < 3 months since thrombosis – LMWH protocol New Thrombosis • Calf vein/Muscular vein – Thrombocytopenic • Doppler 3 days and then weekly until resolved or 4 weeks – Not thrombocytopenia • Muscular – 10 days • Calf – 6 weeks Proximal Vein/PE • New proximal thrombosis – IVC filter controversial • Yes if extensive leg DVT • Can be nidus for thrombosis • Pulmonary embolism – Filter if leg thrombosis Prophylaxis? • Range of DVT is 1.2-5.8% • Would mandate prophylaxis in other situations! • Stockings? • Pharmacologic? Upper Extremity DVT • No RCT • Lower incidence of – PE – Recurrence – Recannulization – Thrombophilia • Higher incidence of – Underlying vascular lesions Catheter Related DVT • Common with PICCs – Less with tunneled catheters • High risk of thrombosis – 3-8% symptomatic – 20-50% asymptomatic • No benefit of prophylaxis Catheter Related DVT • Therapy: High rates of bleeding! – By definition PICC placed in sick patients – RCT 4% incidence life threatening bleeding – OHSU 25% halted due to bleeding Catheter Related DVT • Increasing interest in conservative approach – NeuroICU study > 75% no anticoagulation – OHSU – anticoagulation made no difference in outcomes – NCCN • No anticoagulation if at risk for bleeding Catheter Related DVT • Suggested approach – Pull line – No new one for 10 days – Consider anticoagulation if • Patient very symptomatic • No bleeding risk factors What I Talked About • • • • Antiplatelet agents Antithrombotics Atrial fibrillation Venous thrombosis