* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Epilepsy - Back to Medical School
Drug discovery wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Adherence (medicine) wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Pharmacognosy wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Electronic prescribing wikipedia , lookup
Psychopharmacology wikipedia , lookup
Prescription costs wikipedia , lookup
Drug interaction wikipedia , lookup
Neuropharmacology wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
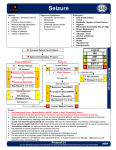
Epilepsy Morgan Feely Consultant Physician Target Meeting Tong, November 2006 Epilepsy A person is said to have ‘epilepsy’ when they have exhibited a tendency to have recurring seizures It is not a single disease Manifest by underlying brain dysfunction from many known or unknown causes Single seizures should not be diagnosed as epilepsy A patient could be said to have ‘one of the epilepsies’ as there are a number of seizure types and causes. Epidemiology Bimodal incidence 440,000 active cases in UK Typical practice: 15 patients per 2000 Age-specific prevalence of treated epilepsy per 1000 persons Source: Wallace, Shorvon, Tallis, Lancet 9.5 9 8.5 8 7.5 7 Prevalence/100 0 6.5 6 5.5 5 4.5 4 3.5 3 2.5 2 1.5 1 0.5 0 5-9 10-14 15-19 20-24 25-29 30-34 35-39 40-44 45-49 50-54 55-59 60-64 65-69 70-74 75-79 80-84 Age 85+ Incidence/100,000 Age-specific incidence of treated epilepsy per 100,000 persons (Source: Wallace, Shorvon, Tallis: The Lancet, 1998 Dec 19–26;352 (9145):1952-3) 210 200 190 180 170 160 150 140 130 120 110 100 90 80 70 60 50 40 30 20 10 0 5-9 10-14 15-19 20-24 25-29 30-34 35-39 40-44 45-49 50-54 Age 55-59 60-64 65-69 70-74 75-79 80-84 85+ The epilepsies Generalised epilepsies (mostly idiopathic) tonic-clonic (T-C) and/or absences and/or myoclonic seizures Location related epilepsies (mostly symptomatic) partial seizures partial +/- secondary (T-C) generalisation Over 200 epilepsy syndromes described - mostly of relevance to young people Seizures across the ages Teens/early 20’s Late 20’s – 50’s Late 50’s – 80+ JME Alcohol / drugs Primary generalised (T-C) Brain tumours Cerebrovascular disease Dementias SAH Brain tumours Partial +/secondary T-C Head injury Metabolic disorders eg low Na Late presentation of earlier types Continuation of childhood/earlier epilepsy Making the diagnosis 1 History History and / or Eye witness or… First tonic-clonic seizure in an adult Clinical scenario You are asked to see a patient who collapsed and appeared to have a ‘fit’ within the last few days and is now back to normal What are the key issues? Seizure versus (convulsive) syncope Provocation (late nights and alcohol, drugs) ? Is there any evidence of previous unrecognised seizures What is the patient’s occupation / driving status? Differences between seizures and syncope Seizures Syncope Any posture (e.g. in bed at night) Blue lips during attack Stiffness and tonic-clonic movements coincide with loss of consciousness and often last for several minutes Patient is rigid as falls to ground Urinary incontinence common Disorientated or headache afterwards Tongue biting and serious injuries are common Seizures arising from secondary generalisation may be preceded by an aura or recognisable partial seizure Occurs standing (or sitting if elderly) Pale and clammy Brief jerking movements may occur after loss of consciousness Patient loses tone then falls to ground Urinary incontinence can occur Quick recovery Tongue biting rarely; serious injuries occur in 5% of cases Often preceded by feeling warm and light headed Case 1 18 year old female law student attends your surgery after suffering a ‘blackout’ following breakfast. Her housemate had said to her she had a ‘grand mal convulsion’. Seizure versus syncope features to support syncope or convulsive syncope…WITNESS / TELEPHONE Provocation Studying for exams, started drinking at university, no illicit drugs Is there any evidence of previous unrecognised seizures Since the age of 16 occasionally ‘daydreams’, jerks in the morning, cup of tea What is the patient’s occupation / driving status Student, drives a car, NB. OCP Diagnosis: JME Case 2 42 year old businessman attends surgery following a generalised seizure. On record he has a heavy alcohol consumption (>50 units per week), but has recently cut down. Seizure versus syncope No clear witness account, any eye witnesses? Provocation Alcohol (ab)use and cut down Is there any evidence of previous unrecognised seizures ‘Has had a fit before’ after binge drinking What is the patient’s occupation / driving status Driver. DVLA issues. Provoked seizure? Case 3 42 year old businessman attends surgery with his wife who is concerned he is behaving oddly at times, repeatedly saying things over and over. On record he has a heavy alcohol consumption (>50 units per week) Seizure versus syncope History from wife ‘Golf-traps! Golf-traps!’ , detached : complex partial seizure(s) Provocation Alcohol use, but not in keeping with focal seizure Is there any evidence of previous unrecognised seizures No What is the patient’s occupation / driving status Driver. Urgent investigations Diagnosis: Glioblastoma Case 4 A 69 year old male attends with seven attacks of speech disturbance lasting 3 minutes over the last 4 months. He has been investigated previously for TIA / stroke. Seizure versus syncope No evidence of syncope. Recurrent stereotypical focal neurology. Clean stroke tests. Provocation No evidence. Not situational. Without warning. Is there evidence of unrecognised seizures? No What is the patient’s occupation / driving status? Driver. DVLA issues Case 5 You are asked to see a 73 year old lady in her RH. She had a previous Left hemi-paresis. The staff think that she has ‘had another stroke.’ Seizure versus syncope? Speak to RH witness. ‘Vacant’ at onset with ‘jerking movements’ of left upper limb. Provocation Recently started antidepressant for low mood, recent UTI and ‘antibiotics’ Is their evidence of unrecognised seizures? RH staff say she occasionally ‘switches off’ and ‘stares into space’. Recurrent ‘strokes’ Occupation / driving status Less relevant, ‘lifestyle issues’. Avoid unnecessary tests? Making the diagnosis 2 Making the diagnosis 3 Management Management Starting AED treatment in newly diagnosed epilepsy AIMS PRINCIPALS Prevention of seizures Appropriate drug for patient’s seizure(s) Minimal side effects Optimise QOL Appropriate drug for individual patient Through trial and error Antiepileptic drug development More AEDS 20 Levetiracetam Tiagabine 15 Topiramate Felbamate Zonisamide 10 Ethosuximide Gabapentin Lamotrigine Carbamazepine Benzodiazepines Primidone Phenobarbital Bromide Fosphenytoin Vigabatrin Sodium valproate 5 Oxcarbazepine Phenytoin 0 1840 1860 1880 1900 1920 Year 1940 1960 1980 2000 Choice of drug Seizure type Women of childbearing age Pregnancy Breastfeeding Children Elderly Learning disability Treatment options by seizure type GENERALISED-ONSET SEIZURES PARTIAL-ONSET SEIZURES Absence myoclonic tonic / atonic primary T-C simple complex-partial secondary generalisation Ethosuxamide CARBAMAZEPINE Phenytoin Vigabatrin Gabapentin Oxcarbazepine VALPROATE LAMOTRIGINE Levetiracetam Topiramate Phenobarbital Benzodiazepines Initial (first line) treatment Drugs for generalised seizures Drugs for partial seizures (+/secondary generalisation) Valproate (Epilim Chrono) Carbemazepine (Tegretol Retard) Lamotrigine Lamotrigine [Topiramate] Valproate (Epilim Chrono) Levetiracetam [Topiramate ] Sodium valproate (Epilim Chrono) Useful for location related and generalised epilepsy Can be brought up to therapeutic dose quickly Low(er) doses tolerated and possibly drug of choice for elderly patients Can cause tiredness, tremor, weight gain, alopecia Teratogenic (spina bifida) Carbamazepine (Tegratol) Good drug for partial seizures in young(er) adults Needs gradual build up to a therapeutic dose Enzyme-inducer, therefore interactions/oestoporisis Most specialists use MR (Tegretol Retard) Lamotrigine (Lamictal) Broad spectrum Good tolerability as monotherapy Well tolerated by the elderly Synergistic effect with sodium valproate Least teratogenic Needs to build up slowly (months) to reduce AEs Rash common, sometimes severe and associated with StevenJohnson’s syndrome Blood dyscrasias Newer second line agents - Levetiracetam (Keppra) Relatively new but appears well tolerated and efficacious Sedation common, though tends to resolve Monotherapy licence Long-term experience still lacking Licensed for partial seizures +/- secondary generalisation (may be effective in other seizure types) Can be started at close to therapeutic range Newer second line agents - Topiramate Potent anticonvulsant activity Useful for most forms of epilepsy Often not tolerated due to side effects: confusion, word-finding difficulties, weight loss Needs slow induction When to start treatment What is the cause? What is the risk of recurrence? First Vs second seizure? What does the patient / carer think? Poor control • Concurrent pro-convulsant drugs Alcohol prescription • Lifestyle Sleep Stress • Concordance / compliance Why? ADR other drugs Social aspects Treatment errors • Incorrect / incomplete detection of seizure(s) resulting in inappropriate drug choice. • Appropriate drug for the seizure(s), but not the patient. • Wrong dose (high or low) • Seizures are controlled, but intolerance / SE are a problem. • The occurrence of a progressive neurological condition Prognosis • 70 – 80% prolonged remission • Poor control Structural lesion EEG abnormality Associated neuropsychiatric disorder More than one drug ? • SUDEP AED withdrawal • Seizure free (remission) > 3 (2?) years • Overall risk of recurrence is 40% • Most relapses occur within the first year off treatment • Factors increasing relapse; syndrome, structural abnormality, severe epilepsy before remission, age. • Discussion risk versus continued therapy DVLA – 6 month suspension Leisure pursuits Contraception / pregnancy etc Service Level Primary Care GMS Referral First seizure Poor control Special cases AED withdrawal Follow-up if stable Re-refer Secondary care Establish diagnosis initiate treatment Follow up Difficult control Tertiary referral Neuro-oncology Obstetrics Elderly Epilepsy Nurse specialists