* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Slide 1
Survey
Document related concepts
Transcript
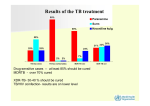
North American Region, IUATLD, San Antonio, 2012 Impact of effective treatment on MDRTB transmission Preliminary Results from the Airborne Infections Research (AIR) Facility Edward A. Nardell, MD Brigham & Women’s Hospital Harvard Medical School Harvard School of Public Health Partners In Health 53 XDR Patients in Kwazulu Natal, South Africa Gandhi, Lancet, 2006: 55% had no previous TB treatment – i.e., transmitted - most had the same “KZN” strain 67% had been hospitalized 100% had HIV co-infection 100% mortality – avg 16 days from TB diagnosis Reinfection Drug Resistant TB in a Boston Homeless Shelter Nardell, et al. NEJM 1986; 315:1570-5 • Proved that transmission (reinfection) was common in a 1983 outbreak of drug resistant TB in a large, crowded homeless shelter in Boston • Conditions not dissimilar to hospital conditions in earlier times in Europe and the US, and in many poor countries today. Don Smith Alterative Pathway to Cavitary TB Smith DW, et al. Rev Infect Dis 11: S385-S393 (1989) NEJM 365;1:79-81, 2011 Force of Transmission Implications Global MDR-TB Treatment Scale Up • Estimated 500,000 new MDR-TB cases per year – More than half result from transmission – 2008 - 29,423 cases reported • 7% of estimated cases • 1% treated with quality assured drugs • Most are treated in hospitals for first 6 months – until sputum smear or culture conversion Source: Multidrug and extensively drugresistant TB (M/XDR-TB) 2010 GLOBAL REPORT ON SURVEILLANCE AND RESPONSE Importance of Transmission in Tomsk Glemanova, et al., Bull WHO, 2007; 85:703-711. • Retrospective study • Substance abuse • MDR-TB occurred – role of non-adherence and default and the acquisition of multidrug resistance – strong predictor of non-adherence (OR 7.3 (2.89-18.46) – but non-adherence NOT associated with MDR-TB – among adherent patients who had been hospitalized in the course of therapy compared to those treated as out- patients • OR 6.34 (1.34 – 29.72) – began treatment in hospital • OR 6.26 (1.02 – 38.35) – hospitalized later during treatment Anton Chekhov, MD Community Based Treatment • Highly effective • e.g., Peru, Lesotho, Cambodia, KZN, and others • Less opportunity for institutional transmission But, what about community transmission? Developing Guidelines for Discontinuation of Isolation for Patients with MultidrugResistant Tuberculosis Sundari Mase MD, MPH Barbara Seaworth MD Edward Nardell MD Jennifer Flood MD, MPH Julian Thomas Discontinuation of Airborne Infection Isolation: Drug-Susceptible TB Organization CDC CDC Title Prevention and Control of Tuberculosis in Correctional and Detention Facilities: Recommendations from CDC Guidelines for preventing the transmission of Mycobacterium tuberculosis in health-care facilities, 2005 Min Days Tx Lab Results Not mentioned 14 Not mentioned Not mentioned Not mentioned 14 3 neg smears Tuberculosis (TB): Clinical Policies and Protocols Not mentioned 14 3 neg smears Canadian Tuberculosis Standards 6th Ed. neg /pos 14 pos/pos 14 The Interdepartmental Working Group on Tuberculosis: The UK Department prevention and control of of Health tuberculosis in the United Kingdom: Department of Health – Publications NYC Bureau of Tuberculosis Control Public Health Agency Canada Smear /Culture pos /neg Not mentioned 3 neg smears 3 neg smears none needed 3 neg cultures Discontinuation of Airborne Infection Isolation: MDR-TB Organization Department of Health Title Prevention and Control of Tuberculosis in Correctional and Detention Facilities: Recommendations from CDC Guidelines for preventing the transmission of Mycobacterium tuberculosis in health-care facilities, 2005 The Interdepartmental Working Group on Tuberculosis: The prevention and control of tuberculosis in the United Kingdom: Department of Health – Publications Bureau of Tuberculosis Control Public Health Agency Canada Tuberculosis (TB): Clinical Policies and Protocols Canadian Tuberculosis Standards 6th Ed. CDC CDC Smear /Culture Min days Tx Lab results Type Suggestion all Not mentioned neg culture comment all Not mentioned neg culture comment all Not mentioned neg culture case by case Not mentioned Not mentioned neg smear + neg culture if possible 3 neg cultures guideline all all Effects of Chemotherapy on Transmission – Early Papers • • • • • • Andrews RH. Bull WHO. 1960 (Madras, India) Crofton J. Bull IUAT. 1962 (Edinburg, Scotland) Brooks S. Am Rev Resp Dis. 1973 (Ohio) Riley R. Am Rev Resp Dis. 1974 (Baltimore) Gunnels J. Am Rev Resp Dis. 1974 (Arkansas) Rouillon A. Tubercle. 1976 (Review): – Smear and culture correlate with infectivity only in untreated cases – Evidence that smear and culture positive TB patients on therapy do not infect skin test negative close contacts. • Menzies R. Effect of treatment on contagiousness of patients with active pulmonary tuberculosis. Infect Control Hops Epidemiol 1997; 18:582-586 The Madras Experience (Bull WHO 1966; 34:517-32) • The first clinical trials of ambulatory TB treatment demonstrated no more household conversions after the start of treatment – Most household contacts had been exposed for months before diagnosis and treatment – Susceptible contacts already infected – Patients no longer infectious Effects of Chemotherapy on Transmission • Brooks et al (ARRD 1973): – 107 TST-negative subjects living with 21 patients with positive sputum. – After up to 23 days hospitalization, 19 smear positive patients were sent home (they did not all become negative on culture until after 5 mos) – No TST negative subjects in contact after the beginning of treatment converted their skin test. Effects of Chemotherapy on Transmission • Riley and Moodie (ARRD, 1974): – studied 70 household contacts of 65 new TB cases on domiciliary treatment (non-RIF regimen) – never hospitalized. – A series of 6 TST results showed no transmission among 25 TST negative contacts after the start of treatment. – Most household contacts were infected in the month or two before diagnosis and treatment . Effects of Chemotherapy on Transmission • Gunnels et al (ARRD 1974): – studied contacts of 155 patients sent home after 1 month of treatment in hospital – 69 Culture neg. – 86 Culture pos • 52 Smear and culture positive. • No difference in infection rate among 284 contacts of culture pos cases versus 216 contacts of culture negative contacts Effects of Chemotherapy on Transmission • Rouillon A, Perdrizet S, Parrot R. Transmission of tubercle bacilli: The effects of chemotherapy. Tubercle 1976; 57:279-299. – Sputum smear and culture positivity correlate with transmission before but not on therapy • Discordance between effect of treatment on culture and smear – Evidence that smear and culture positive TB patients on therapy do not infect close contacts. Effects of Chemotherapy on Transmission (Rouillon) • “There is an ever-increasing amount of evidence in support of the idea that abolition of the patient’s infectiousness – a different matter from ‘cure,’ which takes months, and from negative results of bacteriological examinations, direct and culture, which may take weeks – is very probably obtained after less than 2 weeks of treatment”. • “These facts seem to indicate very rapid and powerful action by the drugs on infectivity…” CDC/ATS Policy on Treatment in general hospitals, communities, and discharge • 1969 ATS – Guidelines for the general hospital for the admission and care of tuberculosis patients. • 1970 ATS – Bacteriologic standards for discharge of patients • 1973 ATS – Guidelines for work for patients with tuberculosis • 1974 CDC – Recommendation for health department supervision of tuberculosis patients Another point of view • Menzies R. Effect of treatment on contagiousness of patients with active pulmonary tuberculosis. Infect Control Hops Epidemiol 1997; 18:582-586. – – – – – – – – • Assumes smear/culture pos. = infectious But, no reported outbreaks from source case on therapy Dismisses Madras due to high rates from the community US studies were not randomized – Riley may have selected less infectious patients for home treatment. Found faults with all epi studies - uninfected household contacts less vulnerable Compared to early studies, most household contacts (in N. America) are uninfected and more vulnerable. Concluded that smear + treated patients should still be considered infectious AFTER 2wks But, no reported outbreaks from source case on therapy Fitzwater SP. Prolonged Infectiousness of tuberculosis patients in a directly observed therapy short-course program with standardized therapy. Clin Infect Dis 2010; 51:371-378. – Drug susceptible TB took median of 37 days to convert, 10% cult pos at 60 days Riley Experimental TB Ward, 1956-60 Am J Hyg 1959; 70:185-196. (reprinted as “classic” Am J Epidemiol 1995; 142:3-14) Hundreds of sentinel guinea pigs sampled the air from a 6-bed TB ward in Baltimore Richard L. Riley & William F. Wells TB transmission only from untreated patients - 1 • Patients selected: – strongly smear positive – cavitary TB • 3 of 77 patients produced 35 of 48 (73%) of GP infections that were cultured – all drug resistant M. tuberculosis on inadequate therapy – 4 month period of no infections when drug susceptible patients were admitted to the ward and started on treatment the same day 4 months Riley Ward – 2nd 2-year study - included untreated patients Relative infectivity of patients*: – Susceptible TB • 61 Untreated • 29 Treated (29 GPs) (1 GP) 100% 2% (14 GPs) (6 GPs) 28% 5% – Drug-resistant TB • 6 Untreated • 11 Treated *all smear positive patients, relative to the amount of time on the ward Riley’s conclusions ARRD 1962; 85:511-525 “The treated patients were admitted to the ward at the time treatment was initiated and were generally removed before the sputum became completely negative. Hence the decrease in infectiousness preceded the elimination of the organisms from the sputum, indicating that the effect was prompt as well as striking.” “Drug therapy appeared to be effective in reducing the infectivity of patients with drug resistant (H, SM, PAS only) organisms, but the data do not permit detailed analysis of the problem”. Dramatic Increase in antibiotic concentration as respiratory droplets evaporate into droplet nuclei Ref. Loudon, et al. Am Rev Resp Dis 1969; 100:172-176. Droplet Drug Concentration Airborne Evaporation Droplet Nucleus Sputum culture vs. GP Infection • • • Sputum sample – no evaporation – no aerosol damage No host defenses Growth support optimized Smear and culture positive • • • Droplet nucleus – evaporation with rising drug concentration – aerosol damage Host defenses Innate immunity No guinea pig infection TB transmission only from untreated patients – Peru Escombe 2008 Plos Medicine; 5:e188 – 97 HIV+ pulmonary TB patients exposed 292 guinea pigs over 505 days • 66 cult +, 35 smear + – 122/125 GP infections (98%) were due to 9 MDR patients • all inadequately or delayed treatment » 108/125 infections (86%) due to 1 MDR patient • 3 drug susceptible patients infected 1 guinea pig each » 2 had delayed treatment » 1 had treatment stopped How effective is treatment in stopping MDR-TB transmission? The AIR Facility Witbank, Mpumalanga Provence, RSA Collaborators: • MRC – – – – – – – – – – • Harvard University Brigham & Women’s Hospital – – – • Other collaborators – – – – • Paul Jensen, engineer Charles Wells Paul Arguin Mpumalanga Provence Health Dept & Specialized MDR TB Referral Center – – – – Edward Nardell, PI Melvin First Ashwin Dharmadhikari Dave McMurray – Texas A & M Ian Orme – Colorado State Randall Basaraba – Colorado State Paul Van Helden, Rob Warren, Elizabeth Streicher - Centre for Molecular and Cellular Biology, Stellenbosch U. Sidney Parsons*, engineer CDC – – – • • CSIR – • Martie van der Walt Matsie Mphahlele Kobus Venter Anton Stoltz Willem Lubbe Thabiso Masotla Karin Weyer Bernard Fourie Lourens Robberts Daan Goosen, Veterinarian Patients Nurses Administration Doctors Funding – – – – – – USAID/CDC MRC Brigham & Women’s Hospital Harvard CFAR (NIH) – two awards NIOSH (NIH) RO1 NIH K23 (A. Dharmadhikari, PI) 109 patients: smear +, cavitary, coughing, recently started on therapy Guinea Pig Transmission: South Africa 109 patients: smear +, cavitary, coughing, recently started on therapy # Patients/ Exp. Duration % guinea pigs infected (# exposed) Patients # XDR (MGIT) Pilot 26* / 4 mos 74% (360) 3/11 Exp 1 24 / 3 mos 10% (90) 5/10 Exp 2 15 / 2 mos 53% (90) 2/11 Exp 3 27 / 3 mos 1% (90) 0/21 0/27 (LPA) Exp 4 17/ 3 mos 77% (90) 2/10 * 8 different spoligotypes, but only 2 transmitted to GPs – both XDR-associated Unsuspected, untreated TB TB DR General Medical Ward Orthopedic Ward Obstetrics Ward Psychiatric Ward TB DS Unsuspected, untreated MDR/XDR TB All other patients on effective treatment TB TB TB TB TB DR TB Hospital TB TB TB Potential for re-infection TB TB TB DR TB TB TB Unsuspected, untreated XDR TB All other patients on effective treatment MDR TB MDR TB MDR TB MDR TB MDR TB MDR TB XDR TB MDR TB MDR TB MDR TB Ward Potential for re-infection MDR TB XDR TB MDR TB MDR TB MDR TB TB Triage – Rapid DR Diagnosis Smear status may not be critical if on effective treatment Individual Isolation XDR by LPA Effect of treatment unknown Novel interventions Gene Xpert: TB, DS or MDR Community based – on effective treatment – responding Complications Hospitalized patients on effective treatment - responding Conclusions • Airborne transmission may be the weak link in TB propagation – Only about 1/3 of pulmonary TB patients infect close contacts • Very little effective treatment may tip the balance against transmission • Sputum smear positivity correlates with infectiousness only in inadequately treated patients. • Strong rationale for prompt diagnosis of drug resistance and prompt effective therapy – can be in the community TB CARE Transmission Control Core Package: “F-A-S-T” • Find TB cases - rapid diagnosis • Focus on rapid molecular diagnosis – Xpert TB • Sputum smear – can also be rapid, but more limited • Active case finding • Focus on cough surveillance • Separate safely and reduce exposure • Building design and engineering • Cough hygiene and triage • Treat effectively, based on rapid DST • Focus on rapid molecular DST – Xpert TB Challenges: Traditional TB IC F-A-S-T Core Strategy • • • • • • • Facility assessment Develop a TB IC plan Political will and resources TB IC committee WHO TB IC Policy – Administrative – Environmental – Respiratory protection Assessment – Process indicators – HCW cases • • • Risk of undiagnosed TB and undiagnosed DR TB Approach: F-A-S-T Political will and resources Focus on certain administrative components – – – – • Rapid diagnosis Active case finding Exposure reduction Effective treatment Assessment – Process indicators – HCW cases Differences Traditional TB IC • Assumes that TB cases on therapy are infectious until smear negative • Assumes that there will be undiagnosed cases transmitting – Focus on environmental controls – Focus on respiratory protection • Lip service to rapid dx and rapid treatment – Someone else’s job F-A-S-T • Assumes that TB cases on effective therapy are non-infectious • Assumes that all coughing patients will be screened, so no undiagnosed TB or drug resistance • Assumes real focus of campaign is on Dx and Rx How do we change an established paradigm? • Objection: Isn’t diagnosis and treatment someone else’s job? – We are expert in TB IC! • Perhaps we need a convincing demonstration (research) project to prove that HCW TB can stop through the FAST approach. • If we change our paradigm, what are the barriers to implementation. – Barriers to HCW case monitoring What does FAST really look like?: Traditional TB IC F-A-S-T Core Strategy • • • • • • • Facility assessment Develop a TB IC plan Political will and resources TB IC committee WHO TB IC Policy – – – • Admin Education HCW Education Patient Education Assessment – Process indicators – HCW cases Work through administration to: Designate cough officers at all facility entrance points – • • • • • HCW education re. cough surveillance Work with lab to assure smear and/or Xpert TB results within 1-2 days Triage and safe separation protocol to reduce exposure Rapid DST within 1-2 days in areas with drug resistance Remove barriers to rapid effective treatment - within 1-2 days Process indicators/HCW cases The New TB IC Core Competencies • Expertise in generating administrative support and funding for FAST approach • Expertise in cough surveillance • Expertise in all steps in rapid molecular diagnosis (< 2d) – Consider breath VOC analysis or CXR to reduce sputum testing • Expertise in triage and short-term exposure reduction • Expertise in rapid, DST-based treatment (2d)