* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Creatinine Clearance When Does It Matter?
Compounding wikipedia , lookup
Psychopharmacology wikipedia , lookup
Plateau principle wikipedia , lookup
Discovery and development of direct thrombin inhibitors wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Pharmacognosy wikipedia , lookup
Drug discovery wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Prescription costs wikipedia , lookup
Drug design wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
Neuropharmacology wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Drug interaction wikipedia , lookup
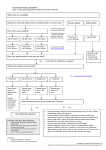
Bruce Lang, BSP PAS Conference April 25, 2015 Objectives Describe the difference between creatinine clearance (CrCl ) and estimated glomerular filtration rate (eGFR) Explain when and how to use which formula Identify when to recommend a change in dose or medication Case CG is a 75yr old male Caucasian with T2DM and stable CKD. He is 175cm and 85kg. His serum creatinine = 198umol/L, eGFR (MDRD) on the lab is 31.2ml/min/1.732 and CrCl (CG)is 29.5ml/min. His BP is 135/86 and ACR=60mg/mmol. He has some pitting edema and has a history of A. Fib. He is also complaining of some muscle soreness in his legs. He is taking the following: Metformin 1g AM and 500mg PM Rosuvastatin 20mg AM Coversyl Plus HD 8/2.5mg daily Warfarin to INR 2-3 Have has had trouble stabilizing on warfarin and the Dr. would like to switch to rivaroxiban and would like your help to dose. Anything else? Endogenous Filtration Markers Creatinine & Cystatin C6,7 Creatinine Cystatin C Small Amino Acid derived from muscle mass Relatively small molecule derived from all nucleated cells Both filtered by the glomerulus and secreted (1015%) by the proximal tubule Filtered but not secreted by the kidney Dependant on age, sex, race and muscle mass Only determinants are age and sex, therefore more uniform across populations Can be affected by alterations in muscle mass and drugs that inhibit tubular secretion (cimetidine, trimethoprim) Not affected by muscle mass. May be influenced by thyroid function and corticosteroid use Inexpensive and easy to use Expensive, therefore will be reserved for confirmatory testing of renal function Used in estimation of CrCl and eGFR Incorporated into equations (CKD-EPI) estimating eGFR Am J Kidney Dis. 2014; 63(5): 820-834 Curr Opin Nephol Hypertens 2014; 23: 258-266 Creatinine Clearance - 1976 Is a measure of how much creatinine is filtered and secreted by the kidney over time expressed as ml/min Surrogate used to estimated GFR, but tends to overestimate true GFR Traditionally used for decades in conjunction with the Cockcroft-Gault (CG) equation to estimate kidney function for drug dosing purposes Uses serum creatinine in the calculation Pharmacotherapy 2011; 31(11): 1130-1144 Nephron 1976; 16: 31-41 eGFR -1999 Glomerular filtration rate is a measure of the ultrafiltrate of blood as it passes through the glomerulus. Used to stage and monitor those with chronic kidney disease (CKD) – and has been utilized for drug dosing??? Uses the Modification of Diet in Renal Disease (MDRD) and Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equations to provide a more accurate assessment of GFR compared to CG. Expressed as ml/min/1.73m2. Also uses serum creatinine in the calculation eGFR results reported by the laboratory are derived by MDRD MDRD is less accurate at levels above 60 ml/min/1.73m2 , therefore will eventually be replaced with the CKD-EPI KDIGO classification of CKD eGFR less the 60 ml/min/1.73m2 for 3 months or more is diagnostic for CKD Albuminuria is an independent risk factor for the progression of CKD Green: low risk (if no other markers of kidney disease, no CKD); Yellow: moderately increased risk; Orange: high risk; Red, very high risk. Kidney International 2013; suppl 3(1) Cockroft-Gault equation -1976 [((140-age)x weight*) x 1.23] ÷ Scr(umol/L) x 0.85 if female reported in ml/min. Reflective of actual renal function Modified CG equation normalized to 70kg10 (used by RQHR and found in eCPS) does not use weight in its formula and correlates well with weight based versions of CG11 . Reflects relative renal function. ((140-age) x 90) ÷ Scr (umol/L) x 0.85 if female reported in ml/min/70kg eCPS reports as ml/second – multiply by 60 to get ml/min Because CG is creatinine based, adjustments may be required for obese patients (BMI greater than 30 or 30% above ideal body weight) [((140-age) x ABW*) x1.23 ] ÷ Scr (umol/L) x 0.85 if female ABW = adjusted body weight Calculators: http://www.globalrph.com/multiple_crcl.htm * weight in kg Am J Health-Syst Pharm 1996: 53: 1028-32 Pharmacotherapy 2011; 31(7): 658-664 Obes Surg 2013; 23: 1427-1430 Am J Health-Syst Pharmacy 2009; 66: 642-648 MDRD GFR = 186.3 x (SCR)-1.154 x (age in years)-0.203 x 1.212 (if patient is African American) x 0.742 (if female) Normalized to ml/min/1.732 Calculator: many: http://www.globalrph.com/multiple_crcl.htm Does not require weight in calculation Provides a more accurate estimate of eGFR, but MDRD underestimates eGFR at levels > 60 ml/min/1.732 Pharmacotherapy 2011; 31(11): 1130-1144 CKD-EPI Chronic Kidney Disease Epidemiology Collaboration Provides a more accurate estimate of eGFR at levels greater than 60 ml/min/1.732 compared to MDRD Can be used with Cystatin C to estimated eGFR Likely to replace MDRD on laboratory reports JAMA 2012; 307(18): 1941-51 Am J Kidney Dis. 2013; 62(3)” 595-603 Which equation for drug dosing? CrCl (CG) or eGFR (MDRD/CKD-EPI) CrCl Considerable experience with CG (50 years) Pharmacokinetic studies (the relationship between CrCl and total drug clearance) and recommendations for dose adjustment in renal impairment based on CG equation Reported in units (ml/min) not adjusted for body surface area which is appropriate for drug dosage adjustment May underestimate GFR in elderly as kidney function does not decrease linearly with age as described in the CG equation19 Current Opinion in Hephrology and Hypertension 2011; 20: 482-91 Am J Health-Syst Pharm 1996; 53: 1028-32 Clin Pharm Therapeutics 2009; 86(5):468-470 Which equation for drug dosing? CrCl (CG) or eGFR (MDRD/CKD-EPI) eGFR Easy availability as reported on all or most lab reports Stevens et al15 studied 5504 participants comparing MDRD and CG Their conclusion was MDRD had greater concordance with measured GFR for drug dosage recommendations relative to the CG equation Stevens et al6 in a recent review found a 78% vs 73% concordance of drug dosing recommendations with MDRD and CG respectively. Am J Kidney Dis 2009; 54(1): 33-42 Am J Kidney Dis 2014; 63(5) 820-834 Clin Pharm Therapeutics 2009; 86(5): 465-467 The Answer Both can be used to recommend drug dosing National Kidney Disease Education Program (2010)16 U. S. FDA – Guidance for Industry (2010)4 Kidney Disease: Improving Global Outcomes (KDIGO) (2011)17 Canadian Society of Nephrology (2015)8 Remember, no equation can accurately estimate kidney function for all patients. Therefore estimates MUST be made in conjunction with the patients clinical status (ie: creatinine must be at steady state, etc.) U.S. FDA. Center for Drug Evaluation and Research. Guidance for Industry: March 2010 Am J Kidney Dis. 2015; 65(2): 177-205 NKDEP. Chronic Kidney Disease nd Drug Dosing: Information for Providers. Jan. 2010 Kidney International 2011; 80: 1122-1137 Concerns with MDRD Tends to overestimate dosing compared to CG particularly in the elderly greater than 75 years of age19,5. This may have implications when making recommendations for drugs: with a narrow therapeutic window With significant adverse event profile Substitution with an alternate agent Direct toxic effects on the kidney MDRD has not been validated for drug dosing in a number of circumstances including the elderly and obesity18 May require recalculation from ml/min/1.732 to ml/min (MDRDIND) for drug dosing recommendations in those who are below ideal body weight or above by >30% or BSA >304,8,16,17 http://mdrd.com/ Pharmacotherapy 2013; 33(9): 912-921 PLOS ONE 2015; March: 1-31 Int J Clin Pract 2015; 69(3): 313-320 Pharmacotherpay 2011; 31(11): 1130-1144 J Am Pharmacists Association 2013; 53(1): 54-57 Estimates of Kidney function by age group The magnitude of difference between CrCl and eGFR as calculated by MDRD and CKD-EPI increases with each decade of life. In the elderly the MDRD overestimates renal function which could lead to higher doses of drugs compared to CG.5, 19,20 Hudson, JQ et al. Int J Clin Pract(2015): 69(3) 313-320 Pharmacotherapy 2013; 33(9): 912-921 Ann Pharmacotherapy 2012; 46: 1174-87 Bottom Line CG vs MDRD/CKD-EPI Both equations can be used to estimate renal function for drug dosing in particular for drugs with broad therapeutic range where a 2-3 fold increase in drug exposure will not have significant impact on safety and efficacy. At this time, it MAY be best to use CG in the elderly (>70 years) and with drugs with narrow therapeutic index such as new oral anticoagulants MDRD should be “normalized” at extremes of body mass. Not for everyone: Amputees, low muscle mass (paraplegic), AKI, malnourished, vegetarian diet. Must be combined with sound clinical judgment in drug dose decision making Pharmacotherapy 2011; 31(11): 1130-1144 Pharmacotherapy 2013; 33(9): 912-921 Curr Opin Nephrol Hypertens 2011; 20: 482-491 J Am Pharmacists Association 2013; 53: 54-57 Drug therapy in CKD General Goals of Therapy 20,21 Most renally excreted drugs (>30% renally excreted) will require some dosage adjustment at <60ml/min / ml/min/1.732 Loading doses may be required for drugs with long half life and the need for rapid achievement of steady state (AMG, levofloxacin, digoxin) Maintenance dose: Maintain usual peak/trough level same dose with longer interval (certain antibiotics : AMG; quinolones) Maintain average steady state lower dose with same dosing interval (antihypertensives, penicillins) Many references : “Drug Prescribing in Renal Failure: Dosing Guidelines for Adults” (Bennett's), eCPS/e-Therapeutics, Lexi-Comp, Micromedex, calculators : http://www.globalrph.com/renaldosing2.htm Ann Pharmacotherapy 2012; 46: 1174-87 Ann Acad Med Singapore 2009; 38: 1095-1103 When should a change in drug or dosing recommendation be made in CKD? With a narrow therapeutic window New oral anticoagulants, digoxin With significant or increased adverse event profile Diabetic medications, statins Substitution with an alternate agent Certain antibiotics, thiazide diuretics Direct toxic effects on the kidney ACE inhibitors Toxic or active metabolites Meperidine, morphine Drug Classes Requiring Dosage Adjustment in CKD Drug Class B Beta Blockers A ACE inhibitors/ARBs N NSAIDS, Opioids D Diuretics D Diabetic medications C Cholesterol medications A M Antimicrobials (Dose reductions are often delayed for 24-48 hours to allow for aggressive dosing/drug to reach steady state) Miscellaneous P Psychotropics Adjust Dose Avoid in Stages 4 and 5 CKD Acebutolol, atenolol, bisoprolol, nadolol, sotalol Sotalol Most ACE inhibitors (adjust according to response) Codeine, Morphine, oxycodone, tramadol, long term NSAIDS Potassium sparing diuretics, loop diuretics Watch for hyperkalmia and possible decrease in renal function All NSAIDS, meperidine Thiazide diuretics, caution with potassium sparing diuretics-monitor closely for hyperkalemia Gliclazide, acarbose, insulin, gliptins Glyburide exanitide Metformin: 50% of present or max dose at Metformin: may be used with caution in select eGFR 30-60ml/min/1.732 individuals Statins. Avoid fibrate/statin combinations due to risk Fibrates –may increase serum creatinine of muscle side effects Antibiotics: Most antibiotics EXCEPT Nitrofurantoin Cloxacillin, clindamycin, metronidazole, Watch for hyperkalemia and increase in serum erythromycin, azithromycin creatinine with trimethoprim Antifungals: fluconazole, itraconazole Antivirals, acyclovir, famciclovir, valacyclovir, valgancyclovir Allopurinol, colchicines, digoxin, H2RAs, New anticoagulants: rivaroxiban, dabigatran Apixaban: decrease dose; avoid <15ml/min) Magnesium/Phosphate containing bowel preps or laxatives Lithium; gabapentin, pregabalin, topiramate, vigabatrin, bupropion, fluoxetine, paroxetine, venlafaxine Adapted from: Saskatchewan Drug Information Services, College of Pharmacy and Nutrition, U of S. www.druginfo.usask.ca New Oral Anticoagulants Apixiban: Usual dose: 5mg bid 2.5mg bid if ≥2 of: age ≥ 80, wt ≤60kg, CrCl <25ml/min Avoid: CrCl<15mL/min Rivaroxiban: Usual dose: 20mg daily with food CrCl 30‐50mL/min: 15mg daily with food CrCl <30mL/min: not recommended Dabigatran: usual dose: 150mg bid 110mg if >75yr & CrCl 30‐50mL/min Avoid if CrCl <30ml/min Diabetic Medications Requiring dose adjustment: – monitor for signs of hypoglycemia22 Sufonylureas Avoid glyburide <60ml/min Gliclazide: consider lower dose <30ml/min. Switch to alternative <15ml/min such as meglitinide. Insulin 30-50% renal elimination. Dose adjustments usually required as renal function declines DPP-4 inhibitors (gliptins) Linagliptin only agent that does not require dose adjustment in renal dysfunction. Can J Diabetes 2014; 38: 334-343 Metformin KDIGO and CSN Renally cleared and clearance decreases by ~75% with CrCl <60ml/min Concern of lactic acidosis (LA) Limited evidence for increased incidence of LA in those with renal function 30-60ml/min (3-10 per 100,000 person-years)23 Greater reduction in 2-year mortality compared to other glucose lowering therapies. May be used with dose reduction in those with CrCl 30-60ml/min (50% reduction from present or max dose) Reasonable to consider in <30ml/min for those with Obesity, stable renal function, close observation and able to follow “sick day” rules Kidney International 2011; 80: 1122-37 Am J Kidney Dis 2015; 65(2): 177-205 JAMA 2014; 312(23): 2668-2675 From: Lipid Management in Chronic Kidney Disease: Synopsis of the Kidney Disease: Improving Global Outcomes 2013 Clinical Practice Guideline. Dosing is generally decreased due to decreased renal clearcence, increased ADR profile and complexity of disease. Ann Intern Med. 2014;160(3):182-189. doi:10.7326/M13-2453 Date of download: 4/2/2014 Copyright © American College of Physicians. All rights reserved. Antihypertensive agents Many require dose adjustment but do so in conjunction with pharmacodynamic effects Diuretics Thiazide ineffective as a diuretic at <30ml/min. Switch to loop diuretic K+ sparing diuretics: dose adjustment and avoidance in stage 4 & 5 CKD. β blockers Lipid soluble β-blockers such as atenolol or sotalol can accumulate in CKD stages 3-5D Bradycardia can be severe ACE inhibitors Watch for declining kidney function/hyperkalemia in those with declining function (stage 3b-5) Antimicrobials Dose reductions often delayed 24-48 hours to allow for aggressive management Maintenance doses of most penicillins, cephalosporins, antifungals and antivirals require dose reduction Nitrofurantoin Ineffective with eGFR <45ml/min Toxic metabolite can accumulate peripheral neuropathy Cotrimoxazole Decrease dose by 50% for those with CrCl 15-30ml/min. Avoid in <15ml/min trimethoprim component can worsen hyperkalemia (usually not until stage 4-5). Increase in creatinine – competition for tubular secretion Sulfa component requires adequate hydration to avoid crystaluria. “Sick Day Rules” Hold the following medications if nausea or vomiting Drug Class Mechanism of action Adverse outcome Sulfonylureas Reduced renal elimination Increased risk of hypoglycemia ACE inhibitors Interfere with kidney’s response to intravascular volume contraction. Decrease intraglomerular pressure Increased risk of decline in renal function Diuretics Exacerbate intravascular volume contraction Increased risk of decline in renal function Metformin Reduced renal elimination; dehydration Increased risk of lactic acidosis Angiotensin receptor blocker Interfere with kidney’s response to intravascular volume contraction Decrease intraglomerular pressure Increased risk of decline in renal function NSAID Afferent arteriolar constriction decreased renal blood flow (renal prostaglandins) Increased risk of decline in renal function Can J Diabetes 38(2014) 334-43 Case CG is a 75yr old male Caucasian with T2DM and stable CKD. He is 175cm and 85kg. His serum creatinine = 198umol/L, eGFR (MDRD) on the lab is 31.2ml/min/1.732 and CrCl (CG)is 29.5ml/min. His BP is 135/86 and ACR=60mg/mmol. He has some pitting edema and has a history of A. Fib. He is also complaining of some muscle soreness in his legs. He is taking the following: Metformin 1g AM and 500mg PM Rosuvastatin 20mg AM Coversyl Plus HD 8/2.5mg daily Warfarin to INR 2-3 Have had trouble stabilizing on warfarin and the Dr. would like to switch to rivaroxiban and would like your help to dose. Anything else? Case Rivaroxiban? dose? Use CG estimation of CrCl CrCl <30ml/min Consider switching to apixiban 5mg bid as CrCl <30ml/min Metformin Use CG estimation of CrCl ?decrease dose or discontinue? Consider switching to meglitinide or even insulin Could also consider continuing with metformin 500mg AM and 250mg PM if there is enough follow-up and he is able to follow sick day rules. Rosuvastatin Could use eGFR or CrCl Decrease dose to no more than 10mg daily or switch to less potent agent such as pravastatin Cosversyl Plus HD Could use eGFR or CrCl. Change to perindopril 8mg + furosemide 40mg daily (renal panel 7 days) Summary May use both CG or MDRD/CKD-EPI for estimating renal function for the purposes of drug dosing CG may be preferable in elderly particularly for drugs with narrow therapeutic window Many drugs require dose adjustment in CKD Dose adjustment, if required, must always be done in consideration of the clinical condition of the patient and the desired pharmacodynamic effects, adverse effect/toxicity profile, and desired outcome of the particular drug