* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Artery Vein - Stephen Tavoni
Survey
Document related concepts
Transcript
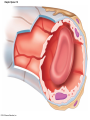
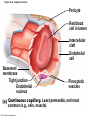
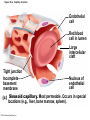
Chapter Opener 18 © 2014 Pearson Education, Inc. Figure 18.1 Generalized structure of arteries, veins, and capillaries. Artery Vein Tunica intima • Endothelium • Subendothelial layer • Internal elastic membrane Tunica media (smooth muscle and elastic fibers) • External elastic membrane Tunica externa (collagen fibers) • Vasa vasorum Artery Vein Valve Capillary network Lumen Capillary © 2014 Pearson Education, Inc. Lumen Basement membrane Endothelial cells Figure 18.1a Generalized structure of arteries, veins, and capillaries. Artery Vein © 2014 Pearson Education, Inc. Figure 18.1b Generalized structure of arteries, veins, and capillaries. Tunica intima • Endothelium • Subendothelial layer • Internal elastic membrane Tunica media (smooth muscle and elastic fibers) • External elastic membrane Tunica externa (collagen fibers) • Vasa vasorum Artery Vein Valve Capillary network Lumen Capillary © 2014 Pearson Education, Inc. Lumen Basement membrane Endothelial cells Figure 18.2 The relationship of blood vessels to each other and to lymphatic vessels. Venous system Large veins (capacitance vessels) Arterial system Heart Elastic arteries (conducting arteries) Large lymphatic vessels Lymph node Lymphatic system Small veins (capacitance vessels) Muscular arteries (distributing arteries) Arteriovenous anastomosis Lymphatic capillaries Sinusoid Arterioles (resistance vessels) Terminal arteriole Postcapillary venule © 2014 Pearson Education, Inc. Thoroughfare channel Capillaries (exchange vessels) Precapillary sphincter Metarteriole Table 18.1 Summary of Blood Vessel Anatomy (1 of 2) © 2014 Pearson Education, Inc. Table 18.1 Summary of Blood Vessel Anatomy (2 of 2) © 2014 Pearson Education, Inc. Figure 18.3 Capillary structure. Pericyte Red blood cell in lumen Intercellular cleft Endothelial cell Basement membrane Tight junction Pinocytotic Endothelial vesicles nucleus Continuous capillary. Least permeable, and most common (e.g., skin, muscle). Pinocytotic vesicles Red blood cell in lumen Fenestrations (pores) Endothelial nucleus Basement membrane Tight junction Intercellular cleft Endothelial cell Fenestrated capillary. Large fenestrations (pores) increase permeability. Occurs in areas of active absorption or filtration (e.g., kidney, small intestine). Endothelial cell Red blood cell in lumen Large intercellular cleft Tight junction Nucleus of Incomplete endothelial basement cell membrane Sinusoid capillary. Most permeable. Occurs in special locations (e.g., liver, bone marrow, spleen). © 2014 Pearson Education, Inc. Figure 18.3a Capillary structure. Pericyte Red blood cell in lumen Intercellular cleft Endothelial cell Basement membrane Tight junction Endothelial nucleus Pinocytotic vesicles Continuous capillary. Least permeable, and most common (e.g., skin, muscle). © 2014 Pearson Education, Inc. Figure 18.3b Capillary structure. Pinocytotic vesicles Red blood cell in lumen Fenestrations (pores) Endothelial nucleus Basement membrane Tight junction Intercellular cleft Endothelial cell Fenestrated capillary. Large fenestrations (pores) increase permeability. Occurs in areas of active absorption or filtration (e.g., kidney, small intestine). © 2014 Pearson Education, Inc. Figure 18.3c Capillary structure. Endothelial cell Red blood cell in lumen Large intercellular cleft Tight junction Incomplete basement membrane Nucleus of endothelial cell Sinusoid capillary. Most permeable. Occurs in special locations (e.g., liver, bone marrow, spleen). © 2014 Pearson Education, Inc. Figure 18.4 Anatomy of a capillary bed. Precapillary sphincters Vascular shunt Metarteriole Thoroughfare channel True capillaries Terminal arteriole Postcapillary venule Sphincters open—blood flows through true capillaries. Terminal arteriole Postcapillary venule Sphincters closed—blood flows through metarteriole – thoroughfare channel and bypasses true capillaries. © 2014 Pearson Education, Inc. Figure 18.4a Anatomy of a capillary bed. Vascular shunt Precapillary sphincters Metarteriole Thoroughfare channel True capillaries Terminal arteriole Postcapillary venule Sphincters open—blood flows through true capillaries. © 2014 Pearson Education, Inc. Figure 18.4b Anatomy of a capillary bed. Terminal arteriole Postcapillary venule Sphincters closed—blood flows through metarteriole – thoroughfare channel and bypasses true capillaries. © 2014 Pearson Education, Inc. Figure 18.5 Relative proportion of blood volume throughout the cardiovascular system. Pulmonary blood vessels 12% Systemic arteries and arterioles 15% Heart 8% Capillaries 5% Systemic veins and venules 60% © 2014 Pearson Education, Inc. Figure 18.6 Blood pressure in various blood vessels of the systemic circulation. 120 Systolic pressure 100 Mean pressure 80 60 40 Diastolic pressure 20 0 © 2014 Pearson Education, Inc. Figure 18.7 The muscular pump. Venous valve (open) Contracted skeletal muscle Venous valve (closed) Vein Direction of blood flow © 2014 Pearson Education, Inc. Figure 18.8 Major factors enhancing cardiac output. Exercise BP activates cardiac centers in medulla Activity of respiratory pump (ventral body cavity pressure) Sympathetic activity Parasympathetic activity Activity of muscular pump (skeletal muscles) Epinephrine in blood Sympathetic venoconstriction Venous return Contractility of cardiac muscle ESV EDV Stroke volume (SV) Heart rate (HR) Initial stimulus Physiological response Result © 2014 Pearson Education, Inc. Cardiac output (CO = SV HR) Figure 18.9 Baroreceptor reflexes that help maintain blood pressure homeostasis. 3 Impulses from baroreceptors stimulate cardioinhibitory center (and inhibit cardioacceleratory center) and inhibit vasomotor center. 4a Sympathetic impulses to heart cause HR, contractility, and CO. 2 Baroreceptors in carotid sinuses and aortic arch are stimulated. 4b Rate of vasomotor impulses allows vasodilation, causing R. 1 Stimulus: Blood pressure (arterial blood pressure rises above normal range). 5 CO and R return blood pressure to homeostatic range. 1 Stimulus: 5 CO and R return blood pressure to homeostatic range. Blood pressure (arterial blood pressure falls below normal range). 4b Vasomotor fibers stimulate vasoconstriction, causing R. 2 Baroreceptors in carotid sinuses and aortic arch are inhibited. 4a Sympathetic impulses to heart cause HR, contractility, and CO. © 2014 Pearson Education, Inc. 3 Impulses from baroreceptors activate cardioacceleratory center (and inhibit cardioinhibitory center) and stimulate vasomotor center. Figure 18.9 Baroreceptor reflexes that help maintain blood pressure homeostasis. (1 of 2) 3 Impulses from baroreceptors stimulate cardioinhibitory center (and inhibit cardioacceleratory center) and inhibit vasomotor center. 4a Sympathetic impulses to heart cause HR, contractility, and CO. 2 Baroreceptors in carotid sinuses and aortic arch are stimulated. 4b Rate of vasomotor impulses allows vasodilation, causing R. 1 Stimulus: Blood pressure (arterial blood pressure rises above normal range). © 2014 Pearson Education, Inc. 5 CO and R return blood pressure to homeostatic range. Figure 18.9 Baroreceptor reflexes that help maintain blood pressure homeostasis. (2 of 2) 1 Stimulus: Blood pressure (arterial blood pressure falls below normal range). 5 CO and R return blood pressure to homeostatic range. 4b Vasomotor fibers stimulate vasoconstriction, causing R. 2 Baroreceptors in carotid sinuses and aortic arch are inhibited. 4a Sympathetic impulses to heart cause HR, contractility, and CO. © 2014 Pearson Education, Inc. 3 Impulses from baroreceptors activate cardioacceleratory center (and inhibit cardioinhibitory center) and stimulate vasomotor center. Table 18.2 Effects of Selected Hormones on Blood Pressure © 2014 Pearson Education, Inc. Figure 18.10 Direct and indirect (hormonal) mechanisms for renal control of blood pressure. Direct renal mechanism Arterial pressure Indirect renal mechanism (renin-angiotensin-aldosterone) Initial stimulus Arterial pressure Physiological response Result Inhibits baroreceptors Sympathetic nervous system activity Filtration by kidneys Angiotensinogen Renin release from kidneys Angiotensin I Angiotensin converting enzyme (ACE) Angiotensin II Urine formation Adrenal cortex ADH release by posterior pituitary Thirst via hypothalamus Secretes Aldosterone Blood volume Sodium reabsorption by kidneys Water reabsorption by kidneys Water intake Blood volume Mean arterial pressure © 2014 Pearson Education, Inc. Mean arterial pressure Vasoconstriction; peripheral resistance Figure 18.11 Factors that increase MAP. Activity of muscular pump and respiratory pump Release of ANP Fluid loss from hemorrhage, excessive sweating Crisis stressors: exercise, trauma, body temperature Conservation of Na+ and water by kidneys Blood volume Blood pressure Blood pH O2 CO2 Blood volume Baroreceptors Chemoreceptors Venous return Activation of vasomotor and cardioacceleratory centers in brain stem Stroke volume Heart rate Vasomotor tone; bloodborne chemicals (epinephrine, NE, ADH, angiotensin II) Diameter of blood vessels Cardiac output Physiological response © 2014 Pearson Education, Inc. Blood viscosity Body size Blood vessel length Peripheral resistance Initial stimulus Result Dehydration, high hematocrit Mean arterial pressure (MAP) Figure 18.12 Body sites where the pulse is most easily palpated. Superficial temporal artery Facial artery Common carotid artery Brachial artery Radial artery Femoral artery Popliteal artery Posterior tibial artery © 2014 Pearson Education, Inc. Dorsalis pedis artery Figure 18.13 Distribution of blood flow at rest and during strenuous exercise. 750 750 Brain 750 Heart 250 12,500 1200 Skeletal muscles 500 Skin Kidneys 1100 Abdomen 1400 1900 Other 600 Total blood flow at rest 5800 ml/min 600 600 400 © 2014 Pearson Education, Inc. Total blood flow during strenuous exercise 17,500 ml/min Figure 18.14 Blood flow velocity and total cross-sectional area of vessels. Relative crosssectional area of different vessels of the vascular bed 5000 4000 Total area (cm2) of the 3000 vascular 2000 bed 1000 0 Velocity of blood flow (cm/s) © 2014 Pearson Education, Inc. 50 40 30 20 10 0 Figure 18.15 Intrinsic and extrinsic control of arteriolar smooth muscle in the systemic circulation. Vasodilators Metabolic O2 CO2 H+ K+ • Prostaglandins • Adenosine • Nitric oxide Neuronal Sympathetic tone Hormonal • Atrial natriuretic peptide Extrinsic mechanisms Intrinsic mechanisms (autoregulation) Vasoconstrictors • Metabolic or myogenic controls • Distribute blood flow to individual organs and tissues as needed Myogenic • Stretch © 2014 Pearson Education, Inc. Neuronal Sympathetic tone Metabolic Hormonal • Endothelins • Angiotensin II • Antidiuretic hormone • Epinephrine • Norepinephrine • Neuronal or hormonal controls • Maintain mean arterial pressure (MAP) • Redistribute blood during exercise and thermoregulation Figure 18.16 Capillary transport mechanisms. Pinocytotic vesicles Red blood cell in lumen Endothelial cell Fenestration (pore) Endothelial cell nucleus Basement membrane Tight junction Lumen Intercellular cleft Caveolae Pinocytotic vesicles Intercellular cleft Endothelial fenestration (pore) Basement membrane 1 Diffusion through membrane (lipid-soluble substances) © 2014 Pearson Education, Inc. 2 Movement through intercellular clefts (watersoluble substances) 4 Transport via vesicles or caveolae (large substances) 3 Movement through fenestrations (water-soluble substances) Figure 18.16 Capillary transport mechanisms. (1 of 2) Pinocytotic vesicles Red blood cell in lumen Endothelial cell Fenestration (pore) Endothelial cell nucleus Basement membrane © 2014 Pearson Education, Inc. Tight junction Intercellular cleft Figure 18.16 Capillary transport mechanisms. (2 of 2) Lumen Caveolae Pinocytotic vesicles Intercellular cleft Endothelial fenestration (pore) Basement membrane 1 Diffusion through membrane (lipid-soluble substances) © 2014 Pearson Education, Inc. 2 Movement through intercellular clefts (watersoluble substances) 4 Transport via vesicles or caveolae (large substances) 3 Movement through fenestrations (water-soluble substances) Figure 18.17 Bulk fluid flow across capillary walls causes continuous mixing of fluid between the plasma and the interstitial fluid compartments, and maintains the interstitial environment. How do the pressures drive fluid flow across a capillary? Net filtration occurs at the arteriolar end of a capillary. The big picture Fluid filters from capillaries at their arteriolar end and flows through the interstitial space. Most is reabsorbed at the venous end. Boundary (capillary wall) Capillary Hydrostatic pressure in capillary “pushes” fluid out of capillary. HPc= 35 mm Hg Osmotic pressure in capillary “pulls” fluid into capillary. OPc= 26 mm Hg Interstitial fluid Arteriole Fluid moves through the interstitial space. For all capillary beds, 20 L of fluid is filtered out per day—almost 7 times the total plasma volume! To determine the pressure driving the fluid out of the capillary at any given point, we calculate the net Hydrostatic pressure filtration pressure (NFP)––the HPif = 0 mm Hg in interstitial fluid outward pressures (HPc and OPif) “pushes” fluid into minus the inward pressures capillary. (Hpif and OPc). So, OPif = 1 mm Hg Osmotic pressure in NFP = (HP + OP ) – (HP + OP ) interstitial fluid “pulls” fluid out of capillary. Net filtration pressure (NFP) determines the direction of fluid movement. Two kinds of pressure drive fluid flow: Hydrostatic pressure (HP) Osmotic pressure (OP) • Due to fluid pressing against • Due to nondiffusible solutes that cannot cross the a boundary • HP “pushes” fluid across the boundary • OP “pulls” fluid across the boundary boundary • In blood vessels, is due to • In blood vessels, is due to blood pressure plasma proteins Piston Boundary Solute molecules (proteins) “Pushes” NFP= 10 mm Hg if if c Net reabsorption occurs at the venous end of a capillary. 17 L of fluid per day is reabsorbed into the capillaries at the venous end. Boundary “Pulls” Venule Capillary Boundary (capillary wall) Hydrostatic pressure in capillary “pushes” fluid out of capillary. HPc = 17 mm Hg The pressure has dropped because of resistance encountered along the capillaries. Osmotic pressure in capillary “pulls” fluid into capillary. About 3 L per day of fluid (and any leaked proteins) are removed by the lymphatic system (see Chapter 20). Interstitial fluid OPc = 26 mm Hg Again, we calculate the NFP: Lymphatic capillary HPif = 0 mm Hg OPif = 1 mm Hg NFP= –8 mm Hg © 2014 Pearson Education, Inc. c = (35 + 1) – (0 + 26) = 10 mm Hg (net outward pressure) As a result, fluid moves from the capillary into the interstitial space. Hydrostatic pressure in NFP = (HPc + OPif) – (HPif + OPc) = (17 + 1) – (0 + 26) interstitial fluid “pushes” = –8 mm Hg (net inward fluid into capillary. pressure) Osmotic pressure in Notice that the NFP at the venous interstitial fluid “pulls” end is a negative number. This fluid out of capillary. means that reabsorption, not filtration, is occurring and so fluid moves from the interstitial space into the capillary. Figure 18.17 Bulk fluid flow across capillary walls causes continuous mixing of fluid between the plasma and the interstitial fluid compartments, and maintains the interstitial environment. (1 of 5) The big picture Fluid filters from capillaries at their arteriolar end and flows through the interstitial space. Most is reabsorbed at the venous end. Arteriole Fluid moves through the interstitial space. For all capillary beds, 20 L of fluid is filtered out per day—almost 7 times the total plasma volume! Net filtration pressure (NFP) determines the direction of fluid movement. Two kinds of pressure drive fluid flow: Hydrostatic pressure (HP) • Due to fluid pressing against a boundary • HP “pushes” fluid across the boundary • In blood vessels, is due to blood pressure Osmotic pressure (OP) • Due to nondiffusible solutes that cannot cross the boundary • OP “pulls” fluid across the boundary • In blood vessels, is due to plasma proteins Piston Boundary “Pushes” Solute molecules (proteins) 17 L of fluid per day is reabsorbed into the capillaries at the venous end. Boundary “Pulls” Venule © 2014 Pearson Education, Inc. About 3 L per day of fluid (and any leaked proteins) are removed by the lymphatic system (see Chapter 20). Lymphatic capillary Figure 18.17 Bulk fluid flow across capillary walls causes continuous mixing of fluid between the plasma and the interstitial fluid compartments, and maintains the interstitial environment. (2 of 5) The big picture Fluid filters from capillaries at their arteriolar end and flows through the interstitial space. Most is reabsorbed at the venous end. Arteriole Fluid moves through the interstitial space. For all capillary beds, 20 L of fluid is filtered out per day—almost 7times the total plasma volume! 17 L of fluid per day is reabsorbed into the capillaries at the venous end. Venule © 2014 Pearson Education, Inc. About 3 L per day of fluid (and any leaked proteins) are removed by the lymphatic system (see Chapter 20). Lymphatic capillary Figure 18.17 Bulk fluid flow across capillary walls causes continuous mixing of fluid between the plasma and the interstitial fluid compartments, and maintains the interstitial environment. (3 of 5) Net filtration pressure (NFP) determines the direction of fluid movement. Two kinds of pressure drive fluid flow: Hydrostatic pressure (HP) Osmotic pressure (OP) • Due to fluid pressing against a boundary • HP “pushes” fluid across the boundary • In blood vessels, is due to blood pressure • Due to nondiffusible solutes that cannot cross the boundary • OP “pulls” fluid across the boundary • In blood vessels, is due to plasma proteins Piston Solute molecules (proteins) Boundary “Pushes” © 2014 Pearson Education, Inc. “Pulls” Boundary Figure 18.17 Bulk fluid flow across capillary walls causes continuous mixing of fluid between the plasma and the interstitial fluid compartments, and maintains the interstitial environment. (4 of 5) How do the pressures drive fluid flow across a capillary? Net filtration occurs at the arteriolar end of a capillary. Capillary Hydrostatic pressure in capillary “pushes” fluid out of capillary. Osmotic pressure in capillary “pulls” fluid into capillary. Boundary (capillary wall) HPc = 35 mm Hg OPc = 26 mm Hg HPif = 0 mm Hg OPif = 1 mm Hg NFP = 10 mm Hg © 2014 Pearson Education, Inc. Interstitial fluid Hydrostatic pressure in interstitial fluid “pushes” fluid into capillary. Osmotic pressure in interstitial fluid “pulls” fluid out of capillary. To determine the pressure driving the fluid out of the capillary at any given point, we calculate the net filtration pressure (NFP)––the outward pressures (HPc and OPif) minus the inward pressures (HPif and OPc). So, NFP = (HPc + OPif) – (HPif + OPc) = (35 + 1) – (0 + 26) = 10 mm Hg (net outward pressure) As a result, fluid moves from the capillary into the interstitial space. Figure 18.17 Bulk fluid flow across capillary walls causes continuous mixing of fluid between the plasma and the interstitial fluid compartments, and maintains the interstitial environment. (5 of 5) Net reabsorption occurs at the venous end of a capillary. Boundary (capillary wall) Capillary Interstitial fluid Hydrostatic pressure in capillary HPc = 17 mm Hg “pushes” fluid out of capillary. The pressure has dropped because of resistance encountered along the capillaries. Osmotic pressure in capillary “pulls” fluid into capillary. OPc = 26 mm Hg HPif = 0 mm Hg Hydrostatic pressure in interstitial fluid “pushes” fluid into capillary. OPif = 1 mm Hg Osmotic pressure in interstitial fluid “pulls” fluid out of capillary. NFP= –8 mm Hg © 2014 Pearson Education, Inc. Again, we calculate the NFP: NFP = (HPc + OPif) – (HPif + OPc) = (17 + 1) – (0 + 26) = –8 mm Hg (net inward pressure) Notice that the NFP at the venous end is a negative number. This means that reabsorption, not filtration, is occurring and so fluid moves from the interstitial space into the capillary. Figure 18.18 Events and signs of hypovolemic shock. Acute bleeding (or other events that reduce blood volume) leads to: 1. Inadequate tissue perfusion resulting in O2 and nutrients to cells Initial stimulus Physiological response Signs and symptoms Result 2. Anaerobic metabolism by cells, so lactic acid accumulates 3. Movement of interstitial fluid into blood, so tissues dehydrate Chemoreceptors activated (by in blood pH) Baroreceptor firing reduced (by blood volume and pressure) Hypothalamus activated (by blood pressure) Brain Minor effect Major effect Respiratory centers activated Cardioacceleratory and vasomotor centers activated Heart rate Sympathetic nervous system activated ADH released Neurons depressed by pH Intense vasoconstriction (only heart and brain spared) Central nervous system depressed Kidneys Renal blood flow Adrenal cortex Renin released Angiotensin II produced in blood Aldosterone released Rate and depth of breathing CO2 blown off; blood pH rises © 2014 Pearson Education, Inc. Tachycardia; weak, thready pulse Kidneys retain salt and water Skin becomes cold, clammy, and cyanotic Blood pressure maintained; if fluid volume continues to decrease, BP ultimately drops. BP is a late sign. Water retention Urine output Thirst Restlessness (early sign) Coma (late sign) Figure 18.19 Pulmonary circulation. Pulmonary capillaries of the R. lung Pulmonary capillaries of the L. lung R. pulmonary L. pulmonary artery artery To systemic circulation Pulmonary trunk R. pulmonary veins From systemic circulation RA LA RV LV L. pulmonary veins Schematic flowchart. Left pulmonary artery Air-filled alveolus of lung Aortic arch Pulmonary trunk Right pulmonary artery Three lobar arteries to right lung Pulmonary capillary Gas exchange Two lobar arteries to left lung Pulmonary veins Pulmonary veins Right atrium Left atrium Right ventricle Left ventricle Illustration. The pulmonary arterial system is shown in blue to indicate that the blood it carries is oxygen-poor. The pulmonary venous drainage is shown in red to indicate that the blood it transports is oxygen-rich. © 2014 Pearson Education, Inc. Figure 18.19a Pulmonary circulation. Pulmonary capillaries of the R. lung R. pulmonary artery Pulmonary capillaries of the L. lung L. pulmonary artery To systemic circulation Pulmonary trunk R. pulmonary veins From systemic circulation LA RA L. pulmonary veins RV © 2014 Pearson Education, Inc. Schematic flowchart. LV Figure 18.19b Pulmonary circulation. Left pulmonary artery Aortic arch Air-filled alveolus of lung Pulmonary trunk Right pulmonary artery Three lobar arteries to right lung Pulmonary capillary Gas exchange Two lobar arteries to left lung Pulmonary veins Right atrium Pulmonary veins Left atrium Right ventricle Left ventricle Illustration. The pulmonary arterial system is shown in blue to indicate that the blood it carries is oxygen-poor. The pulmonary venous drainage is shown in red to indicate that the blood it transports is oxygen-rich. © 2014 Pearson Education, Inc. Figure 18.20 Schematic flowchart showing an overview of the systemic circulation. Common carotid arteries to head and subclavian arteries to upper limbs Capillary beds of head and upper limbs Superior vena cava Aortic arch Aorta RA LA RV LV Azygos system Venous drainage Inferior vena cava Thoracic aorta Arterial blood Capillary beds of mediastinal structures and thorax walls Diaphragm Abdominal aorta Inferior vena cava © 2014 Pearson Education, Inc. Capillary beds of digestive viscera, spleen, pancreas, kidneys Capillary beds of gonads, pelvis, and lower limbs Figure 18.21a Major arteries of the systemic circulation. R. internal carotid artery R. external carotid artery R. common carotid – right side of head and neck R. vertebral R. axillary R. subclavian – neck and R. upper limb Brachiocephalic – head, neck, and R. upper limb Arteries of R. upper limb L. external carotid artery L. internal carotid artery L. common carotid – left side of head and neck L. vertebral L. subclavian – neck and L. upper limb Aortic arch L. axillary Arteries of L. upper limb Ascending aorta – L. ventricle to sternal angle Thoracic aorta T5–T12 (diaphragm) L. and R. coronary arteries L. ventricle of heart Visceral branches Mediastinal – posterior mediastinum Esophageal – esophagus Bronchial – lungs and bronchi Parietal branches Pericardial – pericardium Posterior intercostals – intercostal muscles, spinal cord, vertebrae, pleurae, skin Superior phrenics – posterior and superior diaphragm Diaphragm Abdominal aorta T12 (diaphragm)–L4 Visceral branches Gonadal – testes or ovaries Suprarenal – adrenal glands and Renal – kidneys Superior and inferior mesenterics – small intestine – colon Parietal branches Celiac trunk – liver – gallbladder – spleen – stomach – esophagus – duodenum R. common iliac – pelvis and R. lower limb Arteries of R. lower limb Schematic flowchart © 2014 Pearson Education, Inc. Inferior phrenics – inferior diaphragm Lumbars – posterior abdominal wall Median sacral – sacrum – coccyx L. common iliac – pelvis and L. lower limb Arteries of L. lower limb Figure 18.21b Major arteries of the systemic circulation. Arteries of the head and trunk Internal carotid artery External carotid artery Common carotid arteries Vertebral artery Subclavian artery Brachiocephalic trunk Aortic arch Ascending aorta Coronary artery Celiac trunk Abdominal aorta Superior mesenteric artery Renal artery Gonadal artery Inferior mesenteric artery Arteries that supply the upper limb Subclavian artery Axillary artery Brachial artery Radial artery Ulnar artery Deep palmar arch Superficial palmar arch Digital arteries Arteries that supply the lower limb External iliac artery Femoral artery Common iliac artery Popliteal artery Internal iliac artery Anterior tibial artery Posterior tibial artery Illustration, anterior view © 2014 Pearson Education, Inc. Arcuate artery Figure 18.22a Arteries of the head, neck, and brain. R. Middle cerebral artery R. and L. anterior cerebral arteries Anterior communicating artery Cerebral arterial circle R. and L. Posterior communicating arteries Ophthalmic artery Superficial temporal artery R. posterior cerebral artery Basilar artery R. and L. vertebral arteries Maxillary artery Occipital artery R. and L. internal carotid arteries Facial artery Lingual artery R. and L. external carotid arteries Superior thyroid artery R. and L. common carotid arteries R. and L. subclavian arteries Brachiocephalic trunk Aortic arch Schematic flowchart © 2014 Pearson Education, Inc. Figure 18.22b–d Arteries of the head, neck, and brain. Ophthalmic artery Basilar artery Branches of the external carotid artery Vertebral artery • Superficial temporal artery Internal carotid artery External carotid artery Common carotid artery Thyrocervical trunk Costocervical trunk Subclavian artery Axillary artery • Maxillary artery • Occipital artery • Facial artery • Lingual artery • Superior thyroid artery Larynx Thyroid gland (overlying trachea) Clavicle (cut) Brachiocephalic trunk Internal thoracic artery Anterior Arteries of th e head and neck, right aspect Cerebral arterial circle (circle of Willis) Frontal lobe Optic chiasma • Anterior communicating artery Middle cerebral artery • Anterior cerebral artery Internal carotid artery • Posterior communicating artery Mammillary body • Posterior cerebral artery Basilar artery Temporal lobe Vertebral artery Pons Occipital lobe Cerebellum Posterior Colorized arteriograph of the arterial supply of the brain © 2014 Pearson Education, Inc. Major arteries serving the brain (inferior view, right side of cerebellum and part of right temporal lobe removed) Figure 18.22b Arteries of the head, neck, and brain. Ophthalmic artery Basilar artery Vertebral artery Internal carotid artery External carotid artery Common carotid artery Thyrocervical trunk Costocervical trunk Subclavian artery Axillary artery Arteries of the head and neck, right aspect © 2014 Pearson Education, Inc. Branches of the external carotid artery • Superficial temporal artery • Maxillary artery • Occipital artery • Facial artery • Lingual artery • Superior thyroid artery Larynx Thyroid gland (overlying trachea) Clavicle (cut) Brachiocephalic trunk Internal thoracic artery Figure 18.22c Arteries of the head, neck, and brain. © 2014 Pearson Education, Inc. Colorized arteriograph of the arterial supply of the brain Figure 18.22d Arteries of the head, neck, and brain. Anterior Cerebral arterial circle (circle of Willis) Frontal lobe Optic chiasma • Anterior communicating artery Middle cerebral artery • Anterior cerebral artery Internal carotid artery • Posterior communicating artery Mammillary body • Posterior cerebral artery Basilar artery Temporal lobe Vertebral artery Pons Occipital lobe Cerebellum Posterior Major arteries serving the brain (inferior view, right side of cerebellum and part of right temporal lobe removed) © 2014 Pearson Education, Inc. Figure 18.23a Arteries of the right upper limb and thorax. R. vertebral artery R. common carotid artery L. common carotid artery Thyrocervical trunk L. vertebral artery L. subclavian artery Suprascapular artery R. subclavian artery. Axillary artery Thoracoacromial artery Thoracoacromial artery (pectoral branch) Aortic arch Anterior and posterior circumflex humeral arteries Brachial artery Deep artery of arm Brachiocephalic trunk Internal thoracic artery Anterior intercostal arteries Lateral thoracic artery Subscapular artery Anastomosis Common interosseus artery Radial artery Deep palmar arch Ulnar artery Metacarpal arteries Superficial palmar arch Digital arteries Schematic flowchart © 2014 Pearson Education, Inc. Costocervical trunk Thoracic aorta Posterior intercostal arteries Figure 18.23b Arteries of the right upper limb and thorax. Vertebral artery Thyrocervical trunk Costocervical trunk Suprascapular artery Thoracoacromial artery Axillary artery Subscapular artery Posterior circumflex humeral artery Anterior circumflex humeral artery Common carotid arteries Right subclavian artery Left subclavian artery Brachiocephalic trunk Posterior intercostal arteries Anterior intercostal artery Internal thoracic artery Brachial artery Deep artery of arm Lateral thoracic artery Thoracic aorta Common interosseous artery Radial artery Ulnar artery Deep palmar arch Superficial palmar arch Digital arteries Illustration, anterior view © 2014 Pearson Education, Inc. Figure 18.24a Arteries of the abdomen. Diaphragm Abdominal aorta Inferior phrenic arteries L. gastric artery R. gastric artery Common hepatic artery Hepatic artery proper L Splenic artery Gastroduodenal artery R Celiac trunk R. gastroepiploic artery Middle suprarenal arteries L. gastroepiploic artery Intestinal arteries Middle colic artery Superior mesenteric artery R. colic artery Renal arteries Gonadal arteries Ileocolic artery Sigmoidal arteries Inferior mesenteric artery Lumbar arteries L. colic artery Superior rectal artery Median sacral artery Common iliac arteries Schematic flowchart. © 2014 Pearson Education, Inc. Figure 18.24b Arteries of the abdomen. Liver (cut) Inferior vena cava Celiac trunk Common hepatic artery Hepatic artery proper Gastroduodenal artery Right gastric artery Diaphragm Esophagus Left gastric artery Stomach Splenic artery Left gastroepiploic artery Spleen Gallbladder Pancreas (major portion lies posterior to stomach) Right gastroepiploic artery Duodenum Abdominal aorta Superior mesenteric artery The celiac trunk and its major branches. The left half of the liver has been removed. © 2014 Pearson Education, Inc. Figure 18.24c Arteries of the abdomen. Hiatus (opening) for inferior vena cava Hiatus (opening) for esophagus Diaphragm Inferior phrenic artery Adrenal (suprarenal) gland Middle suprarenal artery Celiac trunk Renal artery Kidney Superior mesenteric artery Abdominal aorta Lumbar arteries Ureter Median sacral artery Major branches of the abdominal aorta. © 2014 Pearson Education, Inc. Gonadal (testicular or ovarian) artery Inferior mesenteric artery Common iliac artery Figure 18.24d Arteries of the abdomen. Celiac trunk Superior mesenteric artery Branches of the superior mesenteric artery • Middle colic artery • Intestinal arteries • Right colic artery • Ileocolic artery Ascending colon Right common iliac artery Ileum Transverse colon Aorta Inferior mesenteric artery Branches of the inferior mesenteric artery • Left colic artery • Sigmoidal arteries • Superior rectal artery Descending colon Cecum Appendix Distribution of the superior and inferior mesenteric arteries. The transverse colon has been pulled superiorly. © 2014 Pearson Education, Inc. Sigmoid colon Rectum Figure 18.25a Arteries of the right pelvis and lower limb. Abdominal aorta Superior gluteal artery Internal iliac artery Inferior gluteal artery Internal pudendal Common iliac artery Obturator artery Deep artery of thigh Medial circumflex femoral artery Lateral circumflex femoral artery External iliac artery Femoral artery Adductor hiatus Arterial anastomosis Popliteal artery Anterior tibial artery Posterior tibial artery Fibular (peroneal) artery Dorsalis pedis artery Lateral plantar artery Lateral plantar artery Medial plantar artery Arcuate artery Plantar arch Dorsal metatarsal arteries Schematic flowchart © 2014 Pearson Education, Inc. Plantar metatarsal arteries Figure 18.25b–c Arteries of the right pelvis and lower limb. Common iliac artery Internal iliac artery Superior gluteal artery External iliac artery Deep artery of thigh Lateral circumflex femoral artery Medial circumflex femoral artery Obturator artery Femoral artery Adductor hiatus Popliteal artery Popliteal artery Anterior tibial artery Anterior tibial artery Posterior tibial artery Fibular artery Dorsalis pedis artery Arcuate artery Dorsal metatarsal arteries Anterior view © 2014 Pearson Education, Inc. Posterior tibial artery Lateral plantar artery Medial plantar artery Posterior view Fibular artery Dorsalis pedis artery (from top of foot) Plantar arch Figure 18.25b Arteries of the right pelvis and lower limb. Common iliac artery Internal iliac artery Superior gluteal artery External iliac artery Deep artery of thigh Lateral circumflex femoral artery Medial circumflex femoral artery Obturator artery Femoral artery Adductor hiatus Popliteal artery Anterior tibial artery Posterior tibial artery Fibular artery Dorsalis pedis artery Arcuate artery Dorsal metatarsal arteries © 2014 Pearson Education, Inc. Anterior view Figure 18.25c Arteries of the right pelvis and lower limb. Popliteal artery Anterior tibial artery Posterior tibial artery Lateral plantar artery Medial plantar artery © 2014 Pearson Education, Inc. Posterior view Fibular artery Dorsalis pedis artery (from top of foot) Plantar arch Figure 18.26a Major veins of the systemic circulation. Veins of R. upper limb R. axillary R. external jugular – superficial head and neck R. vertebral – cervical spinal cord and vertebrae Intracranial dural venous sinuses R. internal jugular – dural venous sinuses of the brain R. subclavian – R. head, neck, and upper limb Same as R. brachiocephalic R. brachiocephalic – R. side of head and R. upper limb L. brachiocephalic – L. side of head and L. upper limb Superior vena cava – runs from union of brachiocephalic veins behind manubrium to R. atrium Azygos system – drains much of thorax R. atrium of heart Diaphragm Inferior vena cava – runs from junction of common iliac veins at L5 to R. atrium of heart R. suprarenal (L. suprarenal drains into L. renal vein) – adrenal glands R. gonadal (L. gonadal drains into L. renal vein) – testis or ovary R. common iliac – pelvis and R. lower limb Veins of R. lower limb © 2014 Pearson Education, Inc. Schematic flowchart. L., R., and middle hepatic veins – liver L. and R. renal veins – kidneys Lumbar veins (several pairs) – posterior abdominal wall L. common iliac – pelvis and L. lower limb Veins of L. lower limb Figure 18.26b Major veins of the systemic circulation. Veins of the head and trunk Dural venous sinuses External jugular vein Vertebral vein Internal jugular vein Right and left brachiocephalic veins Superior vena cava Great cardiac vein Hepatic veins Splenic vein Hepatic portal vein Renal vein Superior mesenteric vein Inferior mesenteric vein Inferior vena cava Common iliac vein Internal iliac vein Veins that drain the upper limb Subclavian vein Axillary vein Cephalic vein Brachial vein Basilic vein Median cubital vein Ulnar vein Radial vein Digital veins Veins that drain the lower limb External iliac vein Femoral vein Great saphenous vein Popliteal vein Posterior tibial vein Anterior tibial vein Small saphenous vein Dorsal venous arch Dorsal metatarsal veins Illustration, anterior view. The vessels of the pulmonary circulation are not shown. © 2014 Pearson Education, Inc. Figure 18.27a Venous drainage of the head, neck, and brain. Superior sagittal sinus Inferior sagittal sinus Occipital vein Superficial temporal vein Straight sinus Transverse sinus Ophthalmic vein Cavernous sinus Facial vein Posterior auricular vein Sigmoid sinus Internal jugular vein External jugular vein Superior thyroid vein Vertebral vein Middle thyroid vein Brachiocephalic veins Subclavian vein Superior vena cava Schematic flowchart © 2014 Pearson Education, Inc. Figure 18.27b–c Venous drainage of the head, neck, and brain. Ophthalmic vein Superficial temporal vein Facial vein Occipital vein Posterior auricular vein External jugular vein Vertebral vein Internal jugular vein Superior and middle thyroid veins Brachiocephalic vein Subclavian vein Superior vena cava Veins of the head and neck, right superficial aspect Superior sagittal sinus Falx cerebri Inferior sagittal sinus Straight sinus Cavernous sinus Transverse sinuses Sigmoid sinus Jugular foramen Right internal jugular vein Dural venous sinuses of the brain © 2014 Pearson Education, Inc. Figure 18.27b Venous drainage of the head, neck, and brain. Ophthalmic vein Superficial temporal vein Facial vein Occipital vein Posterior auricular vein External jugular vein Vertebral vein Internal jugular vein Superior and middle thyroid veins Brachiocephalic vein Subclavian vein Superior vena cava Veins of the head and neck, right superficial aspect © 2014 Pearson Education, Inc. Figure 18.27c Venous drainage of the head, neck, and brain. Superior sagittal sinus Falx cerebri Inferior sagittal sinus Straight sinus Cavernous sinus Transverse sinuses Sigmoid sinus Jugular foramen Right internal jugular vein Dural venous sinuses of the brain © 2014 Pearson Education, Inc. Figure 18.28a Veins of the thorax and right upper limb. Internal Subclavian jugular vein vein External Brachiocephalic jugular vein veins Axillary vein Superior vena cava Accessory hemiazygos vein Median cubital vein Azygos vein Brachial vein Hemiazygos vein Right and left posterior intercostal veins Cephalic vein Median antebrachial vein Radial vein Basilic vein Ulnar vein Deep venous palmar arch Metacarpal veins Superficial venous palmar arch Digital veins Schematic flowchart © 2014 Pearson Education, Inc. Figure 18.28b Veins of the thorax and right upper limb. Brachiocephalic veins Right subclavian vein Axillary vein Brachial vein Cephalic vein Basilic vein Internal jugular vein External jugular vein Left subclavian vein Superior vena cava Azygos vein Accessory hemiazygos vein Hemiazygos vein Posterior intercostals Inferior vena cava Ascending lumbar vein Median cubital vein Median antebrachial vein Cephalic vein Radial vein Anterior view © 2014 Pearson Education, Inc. Basilic vein Ulnar vein Deep venous palmar arch Superficial venous palmar arch Digital veins Figure 18.29a Veins of the abdomen. Inferior vena cava Cystic vein Hepatic portal system Inferior phrenic veins Hepatic veins Hepatic portal vein Superior mesenteric vein Splenic vein Suprarenal veins Renal veins Inferior mesenteric vein Gonadal veins Lumbar veins R. ascending lumbar vein L. ascending lumbar vein Common iliac veins External iliac vein Internal iliac veins Schematic flowchart. © 2014 Pearson Education, Inc. Figure 18.29b–c Veins of the abdomen. Hepatic veins Inferior vena cava Right suprarenal vein Right gonadal vein Inferior phrenic vein Left suprarenal vein Renal veins Left ascending lumbar vein Lumbar veins Left gonadal vein Common iliac vein External iliac vein Internal iliac vein Tributaries of the inferior vena cava. Venous drainage of abdominal organs not drained by the hepatic portal vein. Hepatic veins Liver Hepatic portal vein Small intestine Rectum The hepatic portal circulation. © 2014 Pearson Education, Inc. Gastric veins Spleen Inferior vena cava Splenic vein Right gastroepiploic vein Inferior mesenteric vein Superior mesenteric vein Large intestine Figure 18.29b Veins of the abdomen. Hepatic veins Inferior phrenic vein Inferior vena cava Right suprarenal vein Left suprarenal vein Renal veins Right gonadal vein External iliac vein Left ascending lumbar vein Lumbar veins Left gonadal vein Common iliac vein Internal iliac vein Tributaries of the inferior vena cava. Venous drainage of abdominal organs not drained by the hepatic portal vein. © 2014 Pearson Education, Inc. Figure 18.29c Veins of the abdomen. Hepatic veins Liver Hepatic portal vein Gastric veins Spleen Inferior vena cava Splenic vein Right gastroepiploic vein Inferior mesenteric vein Superior mesenteric vein Small intestine Large intestine Rectum The hepatic portal circulation. © 2014 Pearson Education, Inc. Figure 18.30 Veins of the right lower limb. Common iliac vein Internal iliac vein External iliac vein Inguinal ligament Femoral vein Internal iliac vein Inferior vena cava Great saphenous vein (superficial) Common iliac vein External iliac vein Femoral vein Great saphenous vein Femoral vein Small saphenous vein Anterior tibial vein Fibular (peroneal) vein Fibular (peroneal) vein Posterior tibial vein Plantar veins Dorsalis pedis vein Dorsal venous arch Deep plantar arch Dorsal metatarsal veins Digital veins Anterior Popliteal vein Anterior tibial vein Fibular vein Fibular vein Small saphenous vein (superficial) Anterior tibial vein Dorsalis pedis vein Dorsal Venous arch Posterior tibial vein Plantar veins Dorsal metatarsal veins Deep plantar arch Digital veins Posterior Schematic flowchart of the anterior and posterior veins © 2014 Pearson Education, Inc. Popliteal vein Small saphenous vein Popliteal vein Small saphenous vein Great saphenous vein Anterior view Posterior view Figure 18.30a Veins of the right lower limb. Internal iliac vein Inferior vena cava Common iliac vein External iliac vein Femoral vein Great saphenous vein Femoral vein Popliteal vein Small saphenous vein Small saphenous vein Anterior tibial vein Fibular (peroneal) vein Fibular (peroneal) vein Posterior tibial vein Plantar veins Dorsalis pedis vein Dorsal venous arch Deep plantar arch Dorsal metatarsal veins Digital veins Anterior Posterior Schematic flowchart of the anterior and posterior veins © 2014 Pearson Education, Inc. Figure 18.30b Veins of the right lower limb. Common iliac vein Internal iliac vein External iliac vein Inguinal ligament Femoral vein Great saphenous vein (superficial) Popliteal vein Small saphenous vein Fibular vein Anterior tibial vein Dorsalis pedis vein Dorsal venous arch Dorsal metatarsal veins © 2014 Pearson Education, Inc. Anterior view Figure 18.30c Veins of the right lower limb. Great saphenous vein Popliteal vein Anterior tibial vein Fibular vein Small saphenous vein (superficial) Posterior tibial vein Plantar veins Deep plantar arch Digital veins © 2014 Pearson Education, Inc. Posterior view