* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Study design
Compartmental models in epidemiology wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
Fetal origins hypothesis wikipedia , lookup
Race and health wikipedia , lookup
Public health genomics wikipedia , lookup
Alzheimer's disease research wikipedia , lookup
Multiple sclerosis research wikipedia , lookup
Forensic epidemiology wikipedia , lookup
Women's Health Initiative wikipedia , lookup
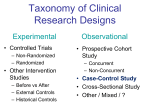
Teaching Registrars Research Methods Study design Landon Myer PhD Senior Lecturer, Infectious Diseases Epidemiology Unit, School of Public Health, UCT [email protected] Orientation to today’s session • So far: – Introduction – Study protocol – Reviewing the Literature • Today: → Study design ← • To come: – Sampling – Measurement – Data analysis – Ethics All of one interrelated process Overview • How to start to select a study design • Framework for considering different study designs – Key similarities & differences • Introduction to each major category of study design – Focus on major functional features – Strengths & limitations – Examples Ask questions throughout! • Exercises Note on terminology • “Outcomes” – Health outcome of interest in the study – Disease, death, side effect, complication • (stats: “dependent variables”) • “Exposures” – Measures that may be associated with the outcome – Possible “risk factors”, “causes”, “determinants” • (stats: “independent variables”) I. Framework for thinking about study designs What are study designs? • Structured approaches to address specific research questions • Provide general guidelines for thinking about specific aspects of study conduct: – sampling populations – systematically collecting measurements – analysing data • Strengths & limitations of specific designs are well-established How to select a study design • Start with a good study question – Relevant • Addresses topic of significance to health of local population / health care services – Novel • Makes meaningful contribution to existing knowledge ~ new insights – Feasible • Not overly ambitious Creativity Different types of study questions lead to different types of study designs • Descriptive – What is the prevalence of condition Z in a specific population? • Analytic – What are the factors associated condition Z? Is condition X a risk factor for condition Z? • Diagnostic – How good is test Q in detecting condition Z? Selecting the right study design option – Relevant • Design allows you to answer your research question – Novel • Design allows meaningful contribution to existing knowledge ~ new insights – Feasible • Design allows study to be done within available time and funds – Simple • ALWAYS avoid ALL unnecessary complexities Types of study designs • Many types – Most are some variation on general themes presented here • All designs based on same basic principles – key differences in how study design samples participants with respect to • “exposures” (risk factors, patient characteristics) • “outcomes” (diseases, conditions) Choice of study design closely related to other aspects of protocol 1. Study design choices inform how you will sample a specific study population • in a way that its understood how the participants in the study relate to the population in general 2. Study design choices inform the most appropriate measurements to collect on participants in a standardised manner (create data) 3. Study designs will point to the most appropriate analysis of data to answer study question: – Descriptive • Calculate the proportion of the study population with condition Z (incident or prevalent) – Analytic • Compare the frequency of condition Z among groups of the population – Diagnostic • Calculate the validity (sensitivity/specificity) or reliability of test Q in detecting condition Z Broad categories of options in study design • Cross-sectional • Case report / case series • Case-control • Cohort • Randomised Controlled Trial (RCT) Broad categories of options in study design • Cross-sectional Diagnostic ? • Case series Descriptive • Case-control • Cohort • Randomised Controlled Trial Analytic Broad categories of options in study design • Cross-sectional • Case report/series Observational designs: investigator is only observing distribution of variables (risk factors, diseases, etc) ‘in nature’ • Case-control • Cohort • RCT Experimental designs: investigator assigns study conditions ~ usually testing an intervention (many variations here) Key differences between study designs 1. How participants are sampled – Are participants sampled according to exposure status, disease status, neither, both? 2. When measurements are taken – Are some variables measured before others, or are measurements taken all at once? 3. How outcome variables are measured – Incident or prevalent outcomes (morb/mort)? 4. Are there comparison groups involved? 5. Is design observational or experimental? Time marches on • Onset of conditions takes place over time in populations • Different study designs deal with the onset of conditions through time in different ways • Critical to understand how your choice of study design handles the timing of – Identification of participants – Measurement of variables (exposure, disease) 1 X X= onset of condition of interest Died 2 Died 3 4 5 X Died 6 7 X 8 X 9 10 Died X X Died 11 Time II. Details on categories of study designs a. b. c. d. e. Case report & case series Case-control Cross-sectional Cohort RCT & other experimental designs Case-report & case-series • Cases – people with health outcome – depends on what is of interest • Case report / series – Describes • characteristics of disease / condition • characteristics of individual that may be associated with the condition Issues in case-only designs • Useful for descriptive purposes only • Implicit comparisions to what is ‘expected’ or ‘normal’ • Why might this be problematic? vs Case-control studies • Set of cases (usually from health service) • Comparable set of controls (various sources) • Both groups evaluated on characteristics / ‘exposures’ of interest – Compare distribution of ‘exposure’ in cases and controls Exposed Cases Unexposed Exposed Controls Unexposed Exposed Cases Unexposed Exposed Controls Unexposed Time Example: Does children’s inhalation of hairspray facilitates development of asthma? • 50 new cases of severe asthma identified at RXH in 12-month period, all <5 yrs of age • These cases are compared to 90 children <5 years attending RXH for orthopedic surgery (who do not have asthma) • Cases and controls are compared on maternal hairspray use since child’s birth Hairspray No hairspray Hairspray No hairspray Children with asthma Children without asthma Odds ratio in 2x2 table Odds ratio = (A/C) / (B/D) Cases Controls E+ A B E- C D A ( C) B (D) Strengths & limitations of casecontrol study • Relatively simple & quick approach to address analytic questions • Ideal to study rare diseases (vs cohort) • Cases & potential controls are accessible in health care setting • Choice of the wrong control group ~ selection bias • Cases may over-report past exposures ~ information bias Cross-sectional studies • Most common form of research ~ “surveys” • Measure all variables on participants at same point in time (approximately) • Measure prevalent disease (not incidence) X Disease X Exposure Time Defined population Sampling Collect data on outcome (disease) and exposure (risk factors) Exposed Diseased Not exposed Diseased Exposed Not exposed Not diseased Not Diseased Example: How severe is disease among rheumatoid arthritis patients attending GSH? • Study population: patients attending rheumatology clinic at GSH during one month period • Measures: degree of disease severity (outcome); demographics, disease history, treatment history (exposures) • Analysis: prevalence of severe disease in clinic population; association between severity of disease and different exposures Benefits of cross-sectional study • Feasibility → easy to do – In health care setting, can work from existing records (consent issues) – Low cost, rapid • Not waiting for incident outcomes to develop • Can calculate prevalence – Often most relevant measure for burden of disease, informing health care strategies – Measure of association: calculate Odds Ratio for prevalent disease Issues in cross-sectional studies • Measuring prevalent disease only – Prevalence incorporates incidence of disease AND duration of disease – Risk factors for prevalent disease often different from risk factors for incident disease • Issues of timing (temporality) are a problem – Exactly when did disease develop? – Did exposures come before or after onset of disease? Cohort studies • Start with group of individuals without the outcome of interest: “at risk” • Follow forward in time to observe incidence of disease (a rate) • Can be descriptive or analytic – If analytic question, then measure exposures on cohort at the beginning of the study Cohort studies can be purely descriptive Eg: What is the rate of remission among men treated for prostate cancer at GSH? At risk participants (without outcome) Develop outcome of interest Do not develop outcome of interest Time Analytic cohort study Eg: Do β-blockers increase risk of renal transplant rejection? Develop the outcome of interest Exposure Do not develop the outcome of interest Study population without the outcome of interest Develop the outcome of interest No exposure Do not develop outcome of interest Time Types of cohort studies • Prospective – Following cohort forward through time from present – Most common approach • Retrospective – Assemble cohort from medical records, – “follow” based on records – Follow-up is in the past (can extend into present) Measure of association in a cohort study: relative risk (aka risk ratio, rate ratio) New cases of outcome Participants who do not develop outcome Exposed A B Total number of exposed = A + B Unexposed C D Total number of unexposed = C + D Total number of participants = A + B +C + D RR = [A/(A+B)] / [C/(C+D)] Strengths + problems in cohort studies • Strengths – Can calcluate rates of new events~ valuable – Timing of exposure before disease assured – Good for studying health effects of rare exposures (can select an exposed cohort) • Weaknesses – Participants ‘self-select’ their exposure status~ leads to confounding, bias – Take time, resources (if prospective) – Many subjects needed for rare outcomes Randomised controlled trials • Principal experimental design in medical research • Like a cohort study, except exposure status is assigned by investigator (randomly)– not just observed • Complex, take time → costly • RCTs are usually best design for testing the impact of a specific intervention in improving a specific health outcome Have outcome of interest Exposure Study population without the outcome of interest Do not develop outcome of interest Randomisation Have outcome of interest No exposure Do not develop outcome of interest Time Key features of RCT • Randomisation • Removes selection bias or confounding • Alternation or other assignment schemes are bad idea • Use of concurrent control groups • Vs Before/After studies • Blinding whenever possible • Blind investigators: prevents information biases • Blind participants: prevents selective behaviour change during the trial • Not just in trials • RCTs are important tools • But can encounter major problems that hinder interpretation of results – Generalizability: Trial participants are highly selected individuals • often not representative of general population at risk – Complexity: Trials procedures can be complex (and costly) • when key design features breakdown, the experiment is compromised Other experimental designs • For an experiment, need to compare 2 states: with intervention vs without • Before/after studies Introduction of Pfizer fluconazole donation programme at GFJ Median survival of cryptococcal meningitis in HIV+ before Median survival of cryptococcal meningitis in HIV+ after • Controlled before/after studies BEFORE AFTER New training in sterile procedures MMH intervention vs Rate of postoperative sepsis Rate of postoperative sepsis No new training NSH control Rate of postoperative sepsis Rate of postoperative sepsis • Time-series studies 25000 300 Rate of advanced cervical cancer cases per 100,000 250 20000 200 15000 150 10000 100 5000 # of pap smears performed in Western Cape 50 0 0 1980 1984 1990 1995 2000 III. Conclusion The “hierarchy” of study designs • Frequently see framework for comparing evidence based on the study design used ‘better evidence’ ~ more valid ‘worse evidence’ ~ less valid RCT / experiments Cohort Case-control Cross-sectional Case series/report Not (nearly) so simple • The study design alone does not make the evidence from a study better or worse • The details of how a study is conducted is what matters – Rigour in design, sampling, measurements, analysis • This is why the Methods section is the most important part of scientific papers Wrap-up • Framework for thinking about study designs when developing research ideas for MMed – Start with a good research question – Understand different study design options – Select the most feasible study design based on the study question • Balance time, funding, available data sources – Understand the strengths and limitations of your approach – Be able to justify your choice of study designs Resources to learn more • Consultations re: study design, conduct, analysis – Ask for help before you start collecting data!! – Email Dr Jim teWaterNaude (to ID appropriate support within School of Public Health) • Self-learning – – – – Hulley SB, Cummings SR. Designing Clinical Research Gordis L. Epidemiology Szklo M, Nieto J. Epidemiology: Beyond the Basics Friedman LM, Fundamentals of Clinical Trials IV. Examples #1 • An investigator is interested in studying the association between schizophrenia and measles vaccinations. – Hypothesis: childhood vaccinations predispose individuals to develop schizophrenia in later life – What study designs are possible? – Which design would you recommend and why? #2 • A study among outpatients attending the GSH diabetes clinic during 2004 collects data on 1432 patients. • Each patient is included once only in the dataset (ie, info from their first visit during 2004) • Data are collected on patient & family history, past treatment, knowledge of disease & its management, disease severity (GTT) • Medicine Registrar decides to examine whether patients with more severe disease have better knowledge of disease & management • What kind of study of this? What measures can be calculated? #3 • You have collected records from your weekly clinic with information on 152 patients– you have data on: – – – – – patient demographic characteristics detailed clinical information on morbidity medical history risk behaviours (smoking, drinking) medications – You need to write an MMed. Quickly. – Identify a research question, a study design, and describe these briefly. • What are the strengths & limitations of the study design you have selected in answering your specific question? #4 • A study of neural tube defects and antenatal folate supplementation, lasting 10 years, follows 10,000 pregnancies in which women used folate supplements, and 10,000 pregnancies in which no supplements were used. – Among women taking folate supplements, 50 cases of neural tube defects were observed – Among women not taking supplements, 150 cases of neural tube defects were observed. #4 – What type of study is this? – What is the appropriate measure of association? – Draw up a 2x2 table, calculate the measure and interpret in one sentence #5 • Another study of folate supplementation and neural tube defects uses a hospital referral system to identify all cases of neural tube defects in the local population. – 200 cases are identified over 10 years (50 among women using supplements, 150 among women not using supplements). – For comparison, investigators select 800 control pregnancies (where no neural tube defects were observed) at random from the same population (of whom 498 use folate supplements and 492 are unexposed). #5 • What type of study is this? • What is the appropriate measure of association? • Draw up a 2x2 table, calculate the measure and interpret in one sentence. • Comparing #4 and #5, what is the principle advantage of the case-control design to cohort design?