* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Pregnancy & Development
Plant reproduction wikipedia , lookup
Cell encapsulation wikipedia , lookup
Birth defect wikipedia , lookup
Umbilical cord wikipedia , lookup
Regeneration in humans wikipedia , lookup
Somatic cell nuclear transfer wikipedia , lookup
Sexual reproduction wikipedia , lookup
Drosophila embryogenesis wikipedia , lookup
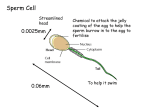
Chapter 28 From Egg to Embryo Fertilization ~ 300 million sperm enter female reproductive tract, most are lost ~2000-5000 reach egg Fertilization occurs when a sperm fuses with an egg to form a zygote. Capcitation: activation of the sperm cell membrane allows release of acrosomal enzymes. Sperm cells bind to the ZP3 glycoprotein receptor on the zona pellucida triggering the acrosomal reaction & releasing acrosomal enzymes From Egg to Embryo Figure 28.2 Hundreds of sperm cells must release their acrosomal enzymes before fertilization can occur Acrosomal enzymes cut through the zona pelucida From Egg to Embryo Figure 28.2 A protein on sperm binds to membrane receptors of oocyte activating the egg receptor to cause fusion of the egg & sperm membranes. sperm nucleus is pulled into the oocyte cytoplasm. From Egg to Embryo Figure 28.2 Polyspermy, or fertilization by more than one sperm cell, leads to a lethal number of chromosomes, & must be prevented. From Egg to Embryo Polyspermy must be prevented. fast block to polyspermy oocyte membrane depolarizes & prevents binding by other sperm cells. Calcium release from oocyte ER The slow block to polyspermy; the destruction of sperm receptors, & swelling of the membrane removes other sperm cells from the surface. From Egg to Embryo Figure 28.3 After a sperm enters an oocyte, it loses its tail & midpiece, & migrates to the center of the oocyte while the oocyte completes meiosis II. From Egg to Embryo Figure 28.3 After meiosis II is completed, male & female pronuclei fuse & produce a zygote, which almost immediately enters into mitosis. Figure 28.3 Figure 28.4 From Egg to Embryo Figure 28.4 Preembryonic Development Preembryonic development begins with fertilization & continues with the movement of the preembryo to the uterus, where it implants in the uterine wall. Cleavage results in smaller cells as mitotic divisions after fertilization occur without much growth between divisions. From Egg to Embryo Figure 28.4 Cleavage forms two identical cells, blastomeres, which by cleavage form a morula, (a hollow ball of cells) by 72 hours. After 4–5 days, the blastocyst escapes from the degrading zona pellucida to implant in the uterine wall. Implantation occurs after 6–7 days; the trophoblast adheres to the endometrium, & produces enzymes that irritate the endometrium. From Egg to Embryo Figure 28.5 Uterine capillaries become permeable & leaky, & the trophoblast proliferates, forming the cytotrophoblast & the syncytiotrophoblast. From Egg to Embryo Figure 28.5 Trophoblast cells secrete human chorionic gonadotropin (hCG), which has LH type activity keeping the corpus luteum functional. Placentation is the formation of the placenta, by proliferation of the trophoblast. Forms cytotrophoblast & syncytiotrophoblast By the end of the third month of gestation the placenta functions as a nutritive, respiratory, excretory, & endocrine organ Events of Embryonic Development Figure 28.7 Formation & Roles of the Embryonic Membranes While implantation is occurring, the blastocyst is being converted into a gastrula, in which three primary germ layers form & embryonic membranes develop. Events of Embryonic Development Figure 28.7 The amnion forms the transparent sac ultimately containing the embryo, & provides a buoyant environment that protects the embryo from physical trauma. Events of Embryonic Development Figure 28.7 The yolk sac forms part of the gut, produces the earliest blood cells & blood vessels, & is the source of germ cells that migrate into the embryo to seed the gonads. Events of Embryonic Development Figure 28.7 The allantois is the structural base for the umbilical cord that links the embryo to the placenta, & becomes part of the urinary bladder. Events of Embryonic Development Figure 28.7 The chorion helps to form the placenta, & encloses the embryonic body & all other membranes. Embryonic Disc Figure 28.8a-e Folding Figure 28.8a-e Figure 28.10a-d Gastrulation Figure 28.8a-e Gastrulation: Germ Layer Formation Gastrulation; the process of transforming the two-layered embryonic disc into a threelayered embryo. ectoderm, mesoderm, & endoderm Gastrulation Fig. 28.8 Figure 28.8f-h Gastrulation begins with the appearance of the primitive streak, which establishes the long axis of the embryo. Cells migrate into the streak to form endoderm then mesoderm Organogenesis Organogenesis: Differentiation of the Germ Layers Organogenesis is the formation of organs & organ systems; by the end of the embryonic period, all organ systems are recognizable. Organogenesis Figure 28.8f-h The ectoderm gives rise to structures of the nervous system & the epidermis. Neurulation, the formation of the brain & spinal cord, is the first event of organogenesis. Figure 28.9a-d Organogenesis Figure 28.12a-c Figure 28.8f-h Fig. 28.8 The mesoderm gives rise to all types of tissues not formed by ectoderm or endoderm, such as muscle tissue. Mesodermal specialization forms the notochord, & gives rise to the dermis, parietal serosa, bones, muscles, cardiovascular structures, & connective tissues. Organogenesis Figure 28.12a-c Figure 28.8f-h Fig. 28.8 The endoderm gives rise to epithelial linings of the gut, respiratory, & urogenital systems, & associated glands. As the embryo develops from a flat plate of cells, it rolls into a tube & the inferior endoderm becomes the lining of the primitive gut. Folding Figure 28.8f-h Figure 28.10a-d Organogenesis By 3 1/2 weeks, the embryo has a blood vessel system & a pumping heart. Vascular modifications include umbilical arteries & veins, a ductus venosus, & the foramen ovale & ductus arteriosus. Figure 28.13a Events of Fetal Development Fig. 28.14 The fetal period extends from weeks 9–38, & is a time of rapid growth of body structures established in the embryo. During the first half of the fetal period, cells are still differentiating into specific cell types to form the body’s distinctive tissues. Effects of Pregnancy on the Mother Anatomical Changes Metabolic Changes Physiological Changes Effects of Pregnancy on the Mother Fig. 28.15 Anatomical Changes Reproductive organs & breasts become more vascular. Uterus enlarges dramatically, shifts the woman’s center of gravity compensated for by accentuated lumbar curvature (lordosis). The placental hormone relaxin causes pelvic ligaments & the pubic symphysis to soften & relax. Normal weight gain of around 28 pounds. Effects of Pregnancy on the Mother Metabolic Changes The placenta produces; Human placental lactogen Promotes breast maturation (with estrogen & progesterone). Promotes the growth of the fetus, & exerts a glucose-sparing effect on maternal metabolism. Human chorionic thyrotropin which increases maternal metabolic rate. Effects of Pregnancy on the Mother Physiological Changes (p. 1135) Morning sickness may be present during the first few months of pregnancy, until adaptation to elevated levels of estrogen & progesterone occurs. Heartburn due to esophageal displacement Constipation may result due to the decreased motility of the digestive tract. Effects of Pregnancy on the Mother Physiological Changes (p. 1135) Increased urine production to dispose of additional fetal metabolic waste. Vital capacity & respiratory rate increases Decrease in residual volume Many women experience dyspnea. Blood pressure & heart rate rise. Blood volume increases to accommodate the needs of the fetus. Parturition (Birth) Parturition is the process of giving birth. Usually within 15 days of the calculated due date. 280 days from the last menstrual period Fig. 28.16 Fig. 28.17 Initiation of Labor Fig. 28.16 Estrogen levels peak: Uterine myometrial cells increase oxytocin receptors Blocks the quieting effect of progesterone on uterine muscle. Fetal cells produce oxytocin, which promotes the release of prostaglandins from the placenta, & further stimulates uterine contraction. Increasing emotional & physical stresses activate the mother’s hypothalamus, which signals the release of oxytocin. Expulsive contractions are aided by a change that occurs in an adhesive protein, fetal fibronectin, converting it to a lubricant. Stages of Labor Fig. 28.17 Stage 1 The dilation stage of labor extends from onset of labor to the time when the cervix is fully dilated by the baby’s head, at about 10 cm in diameter. Stage 2 The expulsion stage extends from full dilation until the time the infant is delivered. When the baby is in the vertex, or head first, position, the skull acts as a wedge to dilate the cervix. Crowning occurs when the baby’s head distends the vulva, & once the head has been delivered, the rest of the baby follows much more easily. After birth, the umbilical cord is clamped & cut. Stage 3 Placental stage, uterine contractions cause detachment of the placenta from the uterine wall, followed by delivery of the placenta & membranes (afterbirth). Occlusion of Special Fetal Blood Vessels & Vascular Shunts Fig. 28.13a Fig. 28.13b After birth, the umbilical arteries & veins constrict & become fibrosed, becoming the medial umbilical ligaments, superior vesical arteries of the bladder, & the round ligament of the liver, or ligamentum teres. Occlusion of Special Fetal Blood Vessels & Vascular Shunts Fig. 28.13a Fig. 28.13b The ductus venosus closes, & is eventually converted to the ligamentum venosum. A flap of tissue covers the foramen ovale, ultimately sealing it & becoming the fossa ovalis, while the ductus arteriosus constricts, becoming the ligamentum arteriosus. Occlusion of Special Fetal Blood Vessels & Vascular Shunts Fig. 28.13a Fig. 28.13b A flap of tissue covers the foramen ovale, ultimately sealing it & becoming the fossa ovalis, while the ductus arteriosus constricts, becoming the ligamentum arteriosus. Lactation Lactation is the production of milk by the hormone-prepared mammary glands. Lactation Fig. 28.18 Rising levels of placental estrogens, progesterone, & lactogen stimulate the hypothalamus to produce prolactinreleasing hormone (PRH), which promotes secretion of prolactin by the anterior pituitary. Colostrum initially secreted for the first two to three days. Nipple stimulation sends sensory input to the hypothalamus stimulating production of PRH & prolactin that maintains milk production. Oxytocin results in of milk let down from the alveoli. Breast milk has multiple advantages. Assisted Reproductive Technology & Reproductive Cloning Hormones can be used to increase sperm or egg production & surgery can be used to open blocked tubes. Assisted reproductive technology involves surgically removing oocytes from a woman’s ovaries, fertilizing the eggs & returning them to the woman’s body. Cloning involves the placing of a somatic cell nucleus into an oocyte. Fig. 28.19