* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Part I: Quelling Cold Sores and Aphthous Ulcers Part I I: Relieving
Survey
Document related concepts
Transcript
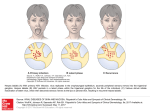
Earn 3 CE credits This course was written for dentists, dental hygienists, and assistants. Part I: Quelling Cold Sores and Aphthous Ulcers Written by Jacalyn Neceskas, PharmD, BCPS; Stacie Moore, PharmD; Susan Goodin, PharmD, FCCP, BCOP Part II: Relieving Xerostomia Written by Fiona M. Collins, BDS, MBA, MA A Peer-Reviewed Publication Published: August 2010 Expiry: July 2013 Go Green, Go Online to take your course This course has been made possible through an unrestricted educational grant. The cost of this CE course is $49.00 for 3 CE credits. Cancellation/Refund Policy: Any participant who is not 100% satisfied with this course can request a full refund by contacting PennWell in writing. Part I: Quelling cold sores and aphthous ulcers Table 1. Implicated factors and associations for RAU Educational Objectives The overall goal of this article is to provide the reader with information on the etiology, pathophysiology, and treatment of recurrent aphthous ulcers and recurrent herpes labialis. Upon completion of this course, the reader will be able to: 1. List and describe the etiology and pathophysiology related to recurrent aphthous ulcers and recurrent herpes labialis. 2. List and describe the general recommendations specific to patients experiencing recurrent herpes labialis. 3. List and describe the treatment options available for recurrent aphthous ulcers and recurrent herpes labialis. Abstract Recurrent aphthous ulcers (RAU) and recurrent herpes labialis (RHL) are two of the common oral/peri-oral lesions experienced in the general population. Treatment options include over-thecounter and prescription products. Introduction Recurrent herpes labialis (cold sores) and recurrent aphthous ulcers (canker sores) are common conditions that can be treated to relieve discomfort and, with some treatments, aid healing. Between 15% and 40% of people experience a cold sore in their lifetime, and it has been estimated that up to 80% of adults carry the herpes virus latently by age 30.1 Forty percent of carriers in the United States are under age 20.2 In addition, the age at which the virus is acquired and seropositivity vary by geography and socioeconomic status, with a greater incidence in younger patients in developing countries.3 Recurrent aphthous ulcers (RAU) are distinct from recurrent herpes labialis (RHL) in presentation and etiology. Although RAU are believed to be less prevalent than RHL, affecting around 1% of the population according to NHANES III, other studies have found an incidence of 5%-66%.4 Etiology and Pathophysiology of RAU and RHL The precise precipitating events and mechanisms for the occurrence of RAU are as yet not fully explained. A wide range of factors have been implicated in RAU (Table 1), with nonsmokers more affected than smokers.5,6 Hypersensitivity to dairy and gluten, as well as sensitivity to sodium lauryl sulfate, are considered etiological factors, and medications implicated in RAU include cardiovascular drugs, interferon, certain antibiotics, and anti-inflammatory drugs.7,8,9 In addition, a higher incidence and severity of RAU have been reported in patients with diseases that include Celiac disease, ulcerative colitis, Behçet’s syndrome, and HIV infection. No consistent association has been found with bacterial or viral factors.10 Based on research there is involvement of the immune system, with the presence of increased levels of circulating and inflammatory mediators including TNF-α, interleukin-2, natural killer cells, and antiendothelial cell autoantibodies.10 50 Sensitivity to sodium lauryl sulfate Stress Iron, folate, zinc or vitamin B12 deficiency Local trauma Medication use Systemic diseases Immune system involvement Genetics Hypersensitivity to dairy and gluten-containing foods RHL, in contrast, are caused by a prior primary infection with herpes simplex virus type 1 (HSV-1). RHL are transmitted by direct contact with the secretions from herpetic lesions, resulting in a primary infection that is often asymptomatic. Once acquired, the infection lies dormant in the peripheral sensory neurons (trigeminal ganglia) until periodic reactivation is induced by a particular trigger or stressor (Table 2). Exposure to a trigger then precipitates viral migration along sensory neurons to the epithelium where the virus replicates and, upon recognition by the immune system, prompts the release of inflammatory mediators followed by a clinically evident RHL outbreak. Table 2. Triggers and stressors for periodic reactivation of HSV-1 Anxiety/stress Infection (e.g., the common cold) Ultraviolet light Dental treatment Menstruation Ultra-violet (UV) light as a trigger has been well-studied in clinical trials. Rooney et al. investigated the effect of sunscreen (SPF-15) application compared to use of a placebo in a randomized, double-blind crossover study. No patients developed active lesions while using SPF-15 sunscreen and only one had asymptomatic viral shedding, while during the placebo phase there were 27 reactivations of lesions, suggesting not only that UV light acts as a trigger but also that sunscreen can play an important role in preventing recurrences.11,5 Clinical Presentation of RAU and RHL RAU are classified as minor, major, and herpetiform recurrent aphthous ulcers. These differ in size (<1 mm to >10 mm in diameter), number and severity of the outbreak. RAU may first cause a tingling sensation before the red raised area at the ulcer site appears prior to ulceration and the appearance of a flat or cratered, grayish-yellow area surrounded by a ring of inflamed tissue. RAU typically occur on nonkeratinized surfaces of the oral mucosa, including the tongue and palate. All 3 types can cause moderate to severe pain, and result in difficulty in eating, drinking, speaking, and swallowing. Minor and herpetiform RAU typically heal within 7-10 days. The most severe are major RAU; these can cause severe debilitating pain, take up to several weeks or months to heal, and heal with scarring. www.rdhmag.com December 2010 Figure 1a. Major recurrent aphthous ulcers Figure 2b. Crusted recurrent herpes labialis lesion Figure 2b: Courtesy of William L. Balanoff, DDS, MS, FICD Figure 1b. Minor recurrent aphthous ulcer RHL are self-limiting and typically heal without scarring; nonetheless, they can significantly affect the patient’s quality of life during outbreaks by resulting in pain, embarrassment, and temporary cosmetic disfigurement. They may also cause uncertainty about the frequency of recurrence. Treatment is most effective if initiated during the initial 48 hours of the recurrence. General Considerations for Patients Figures 1a,b: Courtesy of HIVdent RHL proceed through 8 stages of forming and healing: Prodrome; erythema; papule formation; vesicle formation; ulceration/soft crust; hard crust; desquamation (dry flake); residual swelling.12 During the prodromal phase, patients may experience tingling, numbness, pain or itching associated with the initial viral replication in the nerve endings.3,5,12 After the papules have formed, these coalesce into fluid-filled vesicles that form a crust and heal in 14-21 days during the first occurrence and within 7-10 days during recurrences.5 It is during the vesicle stage that the patient experiences the highest viral load,3 and when the vesicle bursts the patient is also at risk for bacterial superinfection, which would present with pus formation and may require the use of topical antibiotics.5 Along with their classical signs and symptoms, RHL can be definitively detected and identified using DNA amplification tests or by swabbing the lesion and culturing the virus.1 The most common location for RHL to occur is at the junction of the oral mucosa and the lip at the vermilion border. Figure 2a. Intraoral recurrent herpes labialis at vesicle stage It is important to enquire about the occurrence of RAU and RHL with all dental patients, particularly since both occur episodically and may or may not be present at the time of the initial dental visit. By doing so, patients can be proactively counseled on treatment options and care of RAU and RHL, if required. This is especially important for patients suffering from RHL, since treatment is best initiated during the early (prodromal) phase to reduce the severity of the recurrence. Patients should be advised to keep the area adjacent to RHL lesions clean by using a mild antibacterial soap and water and then dabbing the area dry. Patients with RHL should also be advised to wash their hands frequently to prevent the transmission of viral secretions and infection, and to avoid triggers such as sunlight by using sunscreen. Patients experiencing RAU should be advised to avoid spicy and/or acidic foods and drinks, as these may exacerbate discomfort associated with RAU present at that time. In recommending treatment for RAU and RHL, it is essential to stress the importance of visiting (or returning to) the dentist or physician if lesions do not heal within 14 days. Patients should also be referred to their physician for further evaluation if the severity or frequency of recurrences increases, or if they experience other signs and symptoms of infection such as a fever, as these may indicate an underlying systemic condition that needs to be investigated and addressed. If hypersensitivity to a particular food ingredient or chemical is suspected, patients can be advised to avoid these and encouraged to discuss this with their physician. Immunocompromised patients should also be referred to their primary care physician or specialist. Treatment and Care of RAU Figure 2a: Courtesy of Diane M. Daubert, RDH, MS December 2010 Over-the-counter products The mainstay of palliative care, aimed at relieving symptoms until RAU resolve, is over-the-counter (OTC) oral pastes and rinses. www.rdhmag.com 51 Wound-cleansing and debriding rinses are also available that can be applied directly to the lesion or used as a rinse in accordance with the recommendations of the clinician and product labeling. Pain-relieving topical analgesic pastes typically contain 20% benzocaine or 2% lidocaine, and barrier creams are also available that help prevent irritation. A mucosal adhesive patch (Canker Cover™) has been shown to help relieve pain, and forms a barrier over the lesion to help protect it from foods, drinks, and other irritants. This patch contains citrus oil, which has demonstrated antiseptic and anti-inflammatory properties.13 The combination of citrus oil and magnesium chloride has been found in a doubleblind, placebo-controlled clinical trial to result in a shorter healing time of 1.5 days, versus 6 days for placebo (hydroxycellulose base tablets containing no magnesium chloride or citrus oil) and 10 days for untreated patients. The mean time for the elimination of pain was also reduced (5 hours versus 48 hours and 134 hours, respectively).14 A separate study in subjects 18 years of age and older compared the use of the same patch with use of a bioadhesive oral solution (Kank-A®) containing benzocaine and compound benzoin tincture as the active ingredients. It was found that the mucoadhesive patch reduced healing time—mean healing time was 36 hours versus 134.7 hours with the oral solution, there was greater pain reduction at 24 and 48 hours, and the patch was well-tolerated.15 If lesions are widespread, a bioadherent barrier rinse (Rincinol®) can be considered and will coat all of the oral mucosa. Prescription products Prescription products have also been utilized for the treatment of RAU. Five percent tetracycline rinse has been found to reduce healing time and duration of lesions, and to be well-tolerated when used 4 times daily for 5 days or less.10 It should be noted that this is contraindicated during tooth development due to the risk of tetracycline staining. Corticosteroid rinses may be effective in reducing the duration of lesions when used 3-4 times daily, especially where multiple larger ulcers are present and topical application of pastes is impractical. Viscous lidocaine rinse (2%) may be prescribed for pain relief, for rinsing and expectoration, or direct application to the lesion. A bioadherent barrier rinse is also available (Gelclair®). Corticosteroid creams of various potencies have also been investigated for their ability to reduce inflammation and relieve pain, including medium-potency triamcinolone acetonide paste (Kenalog in Orabase®), which has been shown to reduce pain, inflammation, and ulceration when applied 2 or 3 times daily for 5 days.16 One topical cream containing 5% amlexanox (Aphthasol®) has been found in a placebo-controlled, double-blind clinical trial with 1335 subjects to increase the rate of healing while reducing the duration of pain, when applied 4 times daily.17 It is indicated for use in patients 18 years of age and older. A number of systemic treatments have been tested for severe RAU, including the use of thalidomide, orally administered corticosteroids, and levamisol. Due to their toxicity and contraindications, these are reserved for only the most severe cases of RAU; thalidomide is teratogenic and must never be 52 used in pregnant women or women who may become pregnant.18 With both topical and systemic higher potency corticosteroids, consideration must be given to adrenal suppression, which would require tapering off of their use. Table 3. Treatment options for RAU Over-the-counter Pain-relieving topical analgesic pastes Barrier creams and liquid Mucosal barrier adhesive patch (Canker Cover) Bioadherent barrier rinse (Rincinol) Bioadherent barrier analgesic rinse (Kank-A) Prescription - topical Prescription - systemic Viscous lidocaine rinse (2%) Corticosteroids Tetracycline rinse (5%) Levamisol Corticosteroid creams Thalidomide* Amlexanox (5%) Bioadherent barrier rinse Prescription - systemic * Must never be used in women who are/may become pregnant Treatment and Care of RHL Major goals of treatment of RHL include pain relief, reduction of inflammation, improved (faster) healing, avoidance of secondary bacterial infections, and prevention of transmission of viruses to others or self (e.g., autoinoculation to the eyes, which can result in severe infections and blindness). To date no cure is available. A number of controlled clinical trials have demonstrated the efficacy of oral and topical antiviral agents for the prevention and treatment of RHL.12,19,20,21 Over-the-counter treatments A number of OTC products are available for the relief of pain associated with RHL, thereby offering palliative care. These contain topical analgesics such as benzocaine and camphor, lidocaine, or pramoxine. In addition, some contain an antiseptic ingredient such as benzalkonium chloride and some contain sunscreen, skin softener (to soften the crust), and skin protectants. Most of these OTC products are safe for use in young children—the indications and directions on the product labeling should be followed. Nonprescription 10% docosanol cream (Abreva®) is FDA-approved for the treatment of RHL in patients 12 years of age or older,22 and works by inhibiting viral fusion to the host cell. In a randomized, double-blind, placebo-controlled study of 743 patients age 18 or over who experience more than 2 recurrences of RHL per year, the application of 10% docosanol cream 5 times daily resulted in a reduced healing time and time to cessation of pain, but did not reduce lesion formation. Patients were included only if their lesions had not progressed beyond the erythema phase. The median reduction in healing time was 17.5 hours and the median reduction in time to pain cessation was 13.4 hours.19 www.rdhmag.com December 2010 Natural products A number of natural products have efficacy claims for treating or preventing RHL. These include tannic acid, tea tree oil, lemon balm and rhubarb-sage topical cream. Tannic acid has been found to be ineffective, and there is insufficient data to determine the efficacy of tea tree oil;23 limited data is available to show efficacy for lemon balm and rhubarb-sage topical cream. Lysine has also been used to treat RHL. After it was found that arginine deficiency suppressed HSV growth in the laboratory, lysine—an analog of arginine—was investigated for the treatment of RHL with the hypothesis that it would prevent the utilization of arginine by HSV.24 Lysine can be given orally or applied topically. Studies on orally administered lysine, which is sold as a dietary supplement, have produced conflicting results. One crossover study in 65 patients receiving either 500 mg lysine or placebo for 12 weeks found no reduction in the number of recurrences of RHL with either treatment.25 A separate randomized study found no differences in recurrence rates whether patients were taking 624 mg or 1248 mg of lysine daily, but did find significant reductions in recurrences compared to use of placebo.26 Topical lysine (e.g., Lip Clear® Lysine+) has been shown to reduce healing time and to provide relief. An open label trial with 30 patients found that 40% of patients reported a full cure (complete disappearance and resolution of the eruption) by day 3 and 86% by day 4.27 Finally, an over-the-counter homeopathic formulation of zinc oxide with glycine (Novitra®) was studied in a randomized, double-blind clinical trial with 46 patients, where it was used every 2 hours during waking hours. The investigators found that it reduced mean healing time by 1.5 days compared to placebo (based on patient diaries and telephone interviews) and was welltolerated.28 Prescription products FDA-approved prescription products for the treatment of RHL include topical treatments and orally administered systemic treatments. Topical agents include acyclovir cream (Zovirax®) and penciclovir cream (Denavir®). Acyclovir is applied as a cream and works by interfering with the replication of the herpes simplex virus; it is recommended for use in patients age 12 years and older and should be used for 4 days, 5 times a day, as soon as the prodromal (initial) phase begins.29 In 2 randomized, doubleblind, placebo-controlled clinical trials with Zovirax®, reduced length of time to healing and reduced duration of pain were found, but acyclovir did not prevent the progression of lesions to the vesicular phase.30 Penciclovir (1%) is available for use in people age 12 and older and should be applied every 2 hours for 4 days (while awake) as soon as symptoms occur. The efficacy of penciclovir was demonstrated in a randomized, double-blind, placebo-controlled trial with 1573 patients 18 years of age and older who experienced at least 3 RHL per year. The median time to healing was reduced by 0.7 to 1 day, and the time to loss of pain was reduced by a median of 0.6 days.31 Two other identical, randomized, doubleDecember 2010 blind, placebo-controlled multicenter studies with a total of 2537 patients demonstrated the efficacy of penciclovir in reducing healing time when applied within 1 hour of the onset of symptoms. A difference was also found when the cream was used at the papule stage; its use did not prevent lesions from progressing to the vesicle stage.32 A separate small study also demonstrated reduced time to healing by 1 day compared to use of acyclovir.33 Table 4. Clinical results of treatments for RHL Treatment 10% docosanol (Abreva) Topical lysine (Lip Clear® Lysine+) Clinical Results Median pain cessation time reduced by 13.4 hours Median reduction in healing time of 17.5 hours Lesion resolution in 86% of patients by day 4 Zinc oxide with glycine (Novitra®) Median reduction in healing time of 1.5 days Acyclovir cream (Zovirax®) Reduced length of time to healing Penciclovir cream (Denavir®) Valacyclovir tablets Famciclovir tablets Reduced duration of pain Median reduction in healing time of 0.7 - 1 day Median pain cessation time reduced by 0.6 days Median reduction in healing time of 0.8 days Median pain cessation time reduced by 0.5 - 0.7 days Median reduction in healing time of 1.8 - 2.2 days Systemic orally administered tablets containing acyclovir have been found to reduce time to healing when given as 400 mg 5 times per day in a subset of patients, but not at doses of 200 mg, 5 times per day for 5 days.34,35 Valacyclovir is approved by the FDA for the treatment of RHL, administered as a dose of 2000 mg given twice for 1 day, which has been shown to decrease the median time to healing by 0.8 days and to decrease the median number of days of pain by 0.5-0.7 days. There was no effect on lesion progression.36 Oral famciclovir is also approved for the treatment of RHL. Famciclovir as 1500 mg in a single dose or 750 mg given twice for 1 day have both been found to reduce the median time to healing by 1.8-2.2 days, based on a double-blind, randomized trial of 701 patients age 18 or older who experienced at least 3 episodes of RHL annually. However, the single dose of 1500 mg was found to offer greater reduction in the time to resolution of pain or discomfort.37 Summary Recurrent aphthous ulcers and recurrent herpes lesions occur frequently in the general population. After a diagnosis has been made, patients should be given general advice regarding care of these and, in the case of RHL, avoiding transmission of the herpes virus to others. When recommending or prescribing medicaments and drugs, the severity and frequency of the lesions, health status of the individual patient and clinical efficacy of the product should be considered. www.rdhmag.com 53 Part II: Relieving Xerostomia Educational Objectives Oral Signs and Symptoms The overall goal of this article is to provide the reader with information on xerostomia and treatments for the relief of dry mouth. Upon completion of this course the reader will be able to: 1. List the etiological factors for xerostomia. 2. List and describe the signs and symptoms of xerostomia. 3. List and describe the treatment options available for the relief of dry mouth. Individual patients may experience the signs and symptoms of xerostomia to varying degrees depending on the residual level of function of the salivary glands. Symptoms associated with xerostomia include a sticky and/or dry feeling in the mouth, a sensation of pain and burning mouth, alterations in taste, stringy or ropey saliva, difficulty speaking, and a reduced ability to chew and swallow a bolus of food due to a (relative) lack of saliva. Signs of xerostomia include an increased level of carious lesions, the appearance of dryness of the oral mucosa intraorally, increased levels of plaque, bad breath, and oral irritations including angular cheilitis, dry and cracked lips. In addition, xerostomia patients are at increased risk for candidal and other oral infections. The chief complaints of patients with xerostomia are the feeling of dryness in the mouth and difficulties experienced with swallowing and speaking.7 Abstract Xerostomia (dry mouth) affects a significant number of adults and its prevalence increases with age, primarily as the result of the increased use of medications and an increased risk and incidence of diseases/conditions associated with xerostomia. The symptoms of xerostomia can be debilitating and result in a reduced quality of life. Treatment options for the relief of dry mouth include prescription and over-the-counter products, and recommendations should be tailored for the individual patient. Figure 1. Dry appearance of oral mucosa Introduction Xerostomia, or dry mouth, is a common affliction in the general population. An extensive and increasing number of medications are associated with xerostomia, including antidepressants and psychotropics, antihistamines, antihypertensives, and cardiovascular drugs. Estimates on the number of medications with xerostomia as a side effect range from more than 500 to more than 1500.1,2,3 Diseases associated with xerostomia include Sjögren’s syndrome, diabetes, AIDS, and Parkinson’s disease.4 While chemotherapy can also result in xerostomia and changes to the consistency of saliva, head and neck radiation results in severe xerostomia and, as with nerve damage, can completely destroy functioning of the salivary glands. Tobacco and alcohol use also result in a dry mouth. In addition, breathing through the mouth (and snoring) result in dry mouth – this, however, is of a temporary nature and resolves once nose breathing resumes. There is an increased prevalence of xerostomia with age, and it has been estimated that around 25% of adults in the over-65 age group experience xerostomia and at least 10% of all adults are affected.5 While older patients experience dry mouth more frequently, this is related to medication use or other conditions rather than aging itself.6 Figure 2. Angular cheilitis in patient with xerostomia Figures 1 and 2: Courtesy of Sandra L. Boody, RDH, MEd Table 1. Factors in xerostomia Medication use Nerve damage Auto-immune diseases Tobacco use Parkinson’s disease Alcohol use Head and neck radiation therapy Mouth breathing Chemotherapy 54 Detecting and Diagnosing Xerostomia in the Dental Office Patients should be screened for xerostomia. The medical and dental history forms used in the dental office should include questions on medication use, diseases, and medical conditions, and should be reviewed for any present that may result in xerostomia. The medical and dental history forms should also include specific questions on symptoms related to dry mouth, including www.rdhmag.com December 2010 whether the patient has the sensation of dryness in the mouth, dry lips, or difficulty speaking, chewing, or swallowing. Asking whether the patient has to sip water to chew and swallow helps elucidate problems. Detecting xerostomia is best accomplished in the dental office. The oral mucosa may be observed to be dry and parched in appearance, there may be dry or cracked areas on the lips or at the corners of the lips, and an increased caries experience may also indicate xerostomia. Clinical assessment should include placing the mirror against the buccal mucosa to see if it sticks to the mucosa (indicative of inadequate salivary flow). If it is suspected that a patient may have xerostomia, unstimulated and stimulated salivary flow tests will help objectively determine if xerostomia is present and to what degree. In both cases the patient salivates for five minutes and expectorates his or her saliva into a cup or other vessel. A recent protocol for collecting unstimulated saliva recommends that the patient refrain from eating, drinking anything (except water), smoking, chewing gum, and consuming caffeine for one hour before the test is conducted, and that the patient sit still while saliva is collected. For stimulated saliva, the standardized protocol recommends that the patient chew gum in time with a metronome prior to collection of saliva.8 It should be noted that while an objective salivary flow test could indicate that a patient has mild, moderate, or severe xerostomia, the patient may subjectively experience this differently (better or worse). When assessing xerostomia prior to and after initiation of dry mouth–relief treatment, subjective assessment by the patient is a key factor and is performed using either a specific questionnaire designed for the purpose or a visual analog scale (VAS). Treatment Options for Xerostomia Dental professionals are oral care experts and thus positioned to detect, diagnose and recommend primary treatment for xerostomia.9 Patients should be counseled on the importance of home care – extra thorough brushing and flossing to remove plaque is necessary to help prevent caries and periodontal disease and to reduce halitosis. Patients with xerostomia are at increased risk for caries; professional fluoride therapy is indicated as is home use of fluoride toothpaste. Toothpastes formulated for drymouth patients containing lower levels of sodium lauryl sulfate (SLS), or without SLS, and with low foaming activity to reduce the possibility of irritation are available (Biotene Dry Mouth Toothpaste; Biotene PBF Fluoride Toothpaste). As appropriate, patients can be advised to use prescription level paste/gel or over-the-counter alcohol-free adjunctive fluoride rinses. Patients should also be advised to avoid consumption of sugar-containing foods, drinks, and snacks and other fermentable carbohydrates in order to reduce caries risk, as well as to avoid tobacco, caffeine, alcohol, and alcohol-containing rinses due to their drying effect. Sipping water and sleeping with a humidifier have also been shown to help relieve the symptoms of dry mouth. Palliative care of oral irritations can be achieved using topical analgesic pastes containing 20% benzocaine or 2% lidocaine, or using a barrier cream or rinse. The main focus of this article is on the relief of the December 2010 chief symptom and complaint with xerostomia – the sensation of dryness and the discomfort this brings. A number of treatment options are available for xerostomia relief, including prescription and over-the-counter products. Dry Mouth Relief Prescription Products Prescription products used to treat xerostomia include those that stimulate salivary production and those that relieve symptoms. Orally administered systemic treatments that stimulate the production of saliva include pilocarpine hydrochloride (Salagen) and cevimeline hydrochloride (Evoxac). Side effects can include dizziness, alterations in vision, stomach upset, and, rarely, rapid or slowed heart rate and breathing trouble.10 Caphasol is a unit-dose prescription rinse containing calcium and phosphate ions and has been clinically proven to lubricate dry mouth and to reduce the occurrence and severity of mucositis associated with head and neck radiation.11 A second prescription rinse, Numoisyn Liquid, is indicated for relief of dry mouth, has a similar viscosity to saliva, and produces a barrier bioadhesive film on the dentition and oral mucosa.12 The linseed extract contained in Numoisyn has been found to relieve the symptoms of dry mouth.13 Over-the-counter products Over-the-counter products available for relief of dry mouth include mouthwashes, liquids, sprays, gums, lozenges, and a patch. Mouthwashes are formulated to help relieve dry mouth, soothe the oral mucosa, help cleanse the oral cavity, and combat halitosis. These typically contain a base of water and either hydroxyethylcellulose (Biotene Dry Mouth and PBF Mouthwashes) or carboxymethylcellulose (Oasis Moisturizing Mouthwash). Natural-based mouthwashes containing plant extracts and essential oils are also available. Over-the-counter saliva substitute gels and liquids are also available. The primary goals for these are rapid relief of dry mouth and soothing of the oral mucosa. Oral Balance Gel (Biotene) contains protective enzymes as the active ingredient in a hydroxyethylcellulose base. It has been found to be effective in relieving dry mouth, including in head-and-neck-radiation patients and patients who had received whole-body irradiation and chemotherapy.14,15 Biotene saliva substitute has also been shown to be effective in elderly patients for relief of dry mouth.16 The use of Oral Balance Gel and Dry Mouth Toothpaste has been clinically shown to provide greater relief and palliative care in head-and-neck-radiation patients than use of a carboxymethylcellulose gel and regular toothpaste.17 A second saliva substitute containing the same enzymes is available as a liquid in a small portable bottle (Oral Balance Liquid), while another product (Numoisyn Liquid) contains linseed extract. Another option is office-dispensed GC Dry Mouth Gel which can be applied with a finger. Over-thecounter spray and atomizer saliva substitutes have also been found to provide relief from xerostomia.7 www.rdhmag.com 55 Figure 3. Mouthwashes, chewing gums and patch Figure 4a. Patch placed in position with finger Figure 4b. Patch during dissolution for xerostomia relief Intraoral devices have recently also been investigated for the relief of xerostomia. One study found that a night guard fabricated as an ethylene vinyl acetate sheet covering the palate and dental arches, without any reservoir, provided relief from nocturnal xerostomia (assessed using a visual analog scale);24 replacement full dentures with reservoirs containing saliva substitute may also provide relief.25 Summary These may contain glycerin, glycerol, mucin, or carboxymethylcellulose in the base formulation (Salivart; Biotene and Oasis Moisturizing Mouth Sprays; Mouth-Kote; Moi-Stir). Spray saliva substitutes have been found to be effective and their application easy and acceptable to patients.18 Sugar-free lozenges and chewing gums are available that can be used ad libitum to stimulate saliva if salivary gland function is still present19,20 (Wrigley chewing gums). These may also contain xylitol (SalivaSure lozenges, Epic chewing gum, Biotene Dry Mouth Gum), or casein phosphopeptide-amorphous calcium phosphate (CPP-ACP) (Trident Extra chewing gum), which has been shown to help reduce demineralization.21 One brand of lozenge contains essential oils and zinc gluconate and claims to impede biofilm and to kill bacteria associated with halitosis (Salese with Xylitol).22 In addition to stimulating saliva, chewing gum may also help remove plaque and debris through the process of mastication; for many patients chewing gum is a habit they already enjoy and can modify simply by changing to the recommended gum for dry mouth. Patients should be cautioned against using chewing gums containing sugar, which would further increase their high risk for caries. An innovative patch has been introduced for dry mouth relief (OraMoist Dry Mouth Patch). Using a finger, this small mucoadhesive patch is applied to the side of the palate, or in denture/ appliance wearers to the cheek, and dissolves over the course of 2–4 hours to moisturize the mouth and stimulate saliva to provide relief from xerostomia. A recent small study comparing this patch with mouthwash found the patch to be more effective in relieving dry mouth, based on patient self-reporting. Twice as many subjects reported relief using the patch, and its use resulted in a 1.5-fold increase in unstimulated whole salivary flow.23 56 Xerostomia is a debilitating condition that affects a significant percentage of the population and results in reduced quality of life. Treatment is aimed at relieving dry mouth through the stimulation of saliva and use of oral moisturizing products, and at helping to reduce the risk of conditions associated with xerostomia. Once a patient has been diagnosed with xerostomia, treatment planning and recommendations can be made for its management. When making recommendations on products for the relief of dry mouth, the patient’s preferences and subjective assessment of relief attained should be explored – taste, vehicle, ease-of-use and portability, and perceived relief are all factors in patients’acceptance and use of these treatments.26 Dry mouth can be relieved using a number of vehicles that include toothpastes, mouthwashes, saliva substitutes, chewing gums, lozenges, or a mucoadhesive patch, and combinations of these can be used for effective relief of dry mouth. References Part I 1 Vestly JP, Norval M. Mucocutaneous infections with herpes simplex virus and their management. Clin Exp Dermatol. 1992;17:221-37. 2 Xu F, Schillinger JA, Sternberg MR, et al. Seroprevalence and coinfection with herpes simplex virus type I and type 2 in the United States, 1998-1994. J Infect Dis. 2002;185:1019-24. 3 Esmann J. The many challenges of facial herpes simplex infection. J Antimicrob Chemother. 2001;47:17-27. 4 Chattopadhyah P, Chatterjee S. Risk indicators for recurrent aphthous ulcers in the US. Community Dent Oral Epidemiol. 2007;35:152-9. 5 Oral pain and discomfort. In: Allen LV, Berardi RR, DeSimone EL, et al, eds. Handbook of Nonprescription Drugs. 12th ed. Washington, D.C.: American Pharmacists Association; 2000:585-609. 6 Natah SS, Konttinan YT, Enattah NS, et al. Recurrent aphthous ulcers today: a review of the growing knowledge. Int J Oral Maxillofac Surg. 2004;33:221-34. 7 Brokstad B, Barkvoll P. The effect of two toothpaste detergents on the frequency of recurrent aphthous ulcers. Acta Odontol Scand. 1996;54(3):150-3. 8 Abdollahi A, Radfar M. A review of drug-induced oral reactions. J Contemp Dent Pract. 2003;4:10-31. 9 Tack AD, Rogers RS. Oral drug reactions. Dermatol Ther. 2002;15:236-50. 10 Jurge S, Cuffer R, Scully C, Porter SR. Mucosal disease series number VI:Recurrent aphthous stomatitis. Oral Dis. 2006;12:1-21. www.rdhmag.com December 2010 11 Rooney JF, Bryson Y, Mannix ML, et al. Prevention of ultraviolet-light-induced herpes labialis by sunscreen. Lancet. 1991;338;1419-21. 12 Woo S, Challacombe SJ. Management of recurrent oral herpes simplex infections. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103(Suppl 1):e1-S12.e18. 13 Mizrahi B, Shapira L, Dob AJ, Had HY. Citrus oil and magnesium salt as antibacterial and anti-inflammatory agents. J Periodontol. 2006;77(6):963-8. 14 Mizrahi B, Wolnerman Y, Domb AJ. Adhesive tablet effective for treating canker sores in humans. J Pharm Sci. 2004;93(12):2927-35. 15 Shemer A, Amichai B, Trau H, Nathansohn N, Mizrahi B, Domb AJ. Efficacy of a mucoadhesive patch compared with an oral solution for treatment of aphthous stomatitis. Drugs R D. 2008;9(1) 29-35. 16 Herlofson BB, Barkvoll P. Sodium lauryl sulfate and recurrent aphthous ulcers. A preliminary study. Acta Odontol Scand. 1994;52(5):257-9. 17 Khandwala A, Waninwegen RG, Alfano MC. 5% Amlexanox oral paste, a new treatment for recurrent minor aphthous ulcers. Oral Surg Oral Med Oral Path. 1997;83(2):222-30. 18 Porter SR. Recurrent aphthous stomatitis. Crit Rev Oral Biol Med. 1998;9(3):306-21. 19 Raborn GW, Chan KS, Grace M. Treatment modalities and treatment recommended by health care professionals for treating recurrent herpes labialis. J Am Dent Assoc. 2004;135:48-54. 20 Sacks SL, Thisted RA, Jones TM, et al. Clinical efficacy of topical docosanol 10% cream for herpes simplex labialis: a multicenter, randomized placebocontrolled trial. J Am Acad Dermatol. 2001;45:222-30. 21 Gaby AR. Natural remedies for herpes simplex. Altern Med Rev. 2006;11(2):93-101. 22 About Abreva: Efficacy and use. Abreva Web site. http://www.abreva.com. 23 Carson CF, Ashton L, Dry L, et al. Melaleuca alternifolia (tea tree) oil gel (6%) for the treatment of recurrent herpes labialis. J Antimicrob Chemother. 2001;48:450-1. 24 Griffith RS, DeLong DC, Nelson JD. Relation of arginine-lysine antagonism to herpes simplex growth in tissue culture. Chemotherapy. 1981;27:209-13. 25 Tomblin FA Jr, Lucas KH. Lysine for management of herpes labialis. Am J Health Syst Pharm. 2001;58:300-4. 26 McCune MA, Perry HO, Muller SA, et al. Treatment of recurrent herpes simplex infections with L-lysine monohydrochloride. Cutis. 1984;34:366-73. 27 Singh BB, Udani J, Vinjamury SP, et al. Safety and effectiveness of an L-lysine, zinc, and herbal-based product on the treatment of facial and circumoral herpes. Altern Med Rev. 2005;10:123-7. 28 Godfrey HR, Godfrey NJ, Godfrey JC, et al. A randomized clinical trial on the treatment of oral herpes with topical zinc oxide/glycine. Alter Ther Health Med. 2001;7:49-56. 29 Zovirax cream 5% (package insert). Glaxosmithkline. 30 Spruance SL, Nett R, Marbury T, et al. Acyclovir cream for treatment of herpes simplex labialis: results of two randomized, double-blind, vehicle-controlled, multicenter clinical trials. Antimicrob Agents Chemother. 2002;46(7):2238-43. 31 Spruance SL, Rea TL, Thoming C, et al. Pencyclovir cream for the treatment of recurrent herpes simplex labialis: a randomized, multicenter, double-blind, placebo-controlled trial. J Am Med Assoc. 1997;277:1374-9. 32 Raborn GW, Martel AY, Lasonde M, et al. Effective treatment for herpes simplex labialis with penciclovir cream: combined results of two trials. J Am Dent Assoc. 2001;133:303-9. 33 Femiano F, Gambos F, Scully C. Recurrent herpes labialis: efficacy of topical therapy with penciclovir compared with acyclovir (acyclovir). Oral Dis. 2001;7:31-3. 34 Raborn GW, McGaw WT, Greace M, et al. Oral acyclovir and herpes labialis: a randomized, double-blind, placebo-controlled study. J Am Dent Assoc. 1987;115(1):38-42. 35 Spruance SL, Stewart JC, Rowe NH, et al. Treatment of recurrent herpes simplex labialis with oral acyclovir. J Infect Dis. 1990;161:185-90. 36 Spruance SL, Jones TM, Blatter MM, et al. High-dose, short-duration, early valacyclovir therapy for episodic treatment of cold sores: results of two randomized, placebo-controlled, multicenter studies. Antimicrob Agents Chemother. 2003;47:1072-80. 37 Spruance SL, Bodsworth N, Resnick H, et al. Single-dose, patient-initiated famciclovir: a randomized, double-blind, placebo-controlled trial for episodic treatment of herpes labialis. J Am Acad Dematol. 2006;55:47-53. References Part II 1 2 3 4 Porter SR, Scully C, Hegarty AM. An update of the etiology and management of xerostomia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97:2846. Sreebny LM, Schwartz SS. A reference guide to drugs and dry mouth—2nd edition. Gerodontology. 1997;14:33-47. http://www.drymouth.info/practitioner/overview.asp Mouly SJ, Orler JB, Tillet Y, Coudert AC, Oberli F, et al. Efficacy of a new oral lubricant solution in the management of psychotropic druginduced xerostomia: a randomized controlled trial. J Clin Psychopharmacol. 2007;27(5):437-43. December 2010 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 Managing xerostomia. Vital 6, 32–34 (1 March 2009) | doi:10.1038/vital944 Atkinson JC, Grisius M, Massey W. Salivary hypofunction and xerostomia: diagnosis and treatment. Dent Clin N Am. 2005;49:309- 26. Vissink A, Panders AK, Gravenmade EJ, Vermey A. Treatment of oral symptoms in Sjögren’s syndrome. Scand J Rheumatol Suppl. 1986;61:270-3. Navazesh M, Kumar SK. Measuring salivary flow: challenges and opportunities. J Am Dent Assoc. 2008;139 Suppl:35S-40S. Frost PM. Difficulties in dental prescribing of saliva substitutes for xerostomia. Gerodontology. 2002;19(2):123-4. http://www.medicinenet.com/pilocarpine-oral/article.htm Papas AS, Clark RE, Martuscelli G, O’Loughlin KT, Johansen E, et al. A prospective, randomized trial for the prevention of mucositis in patients undergoing hematopoietic stem cell transplantation. Bone MarrowTransplant. 2003;8:705-12. Christersson CE, Lindh L, Arnebrant T. Film-forming properties and viscosities of saliva substitutes and human whole saliva. Eur J Oral Sci. 2000;108:418-425. Andersson G, Johansson G, Attstrom R, Edwardsson S, Glantz P-O, et al. Comparison of the effect of the linseed extract Salinum® and a methyl cellulose preparation on the symptoms of dry mouth. Gerodontology. 1995;12:12-17. Shahdad SA, Taylor C, Barclay SC, Steen IN, Preshaw PM. A double-blind, crossover study of Biotène Oralbalance and BioXtra systems as salivary substitutes in patients with post-radiotherapy xerostomia. Eur J Cancer Care (Engl). 2005;14(4):319-26. Sugiura Y, Soga Y, Tanimoto I, Kokeguchi S, Nishide S, et al. Antimicrobial effects of the saliva substitute, Oralbalance, against microorganisms from oral mucosa in the hematopoietic cell transplantation period. Support Care Cancer. 2008;16(4):421-4. Matear DW, Barbaro J. Effectiveness of saliva substitute products in the treatment of dry mouth in the elderly: a pilot study. J R Soc Promot Health. 2005;125(1):35-41. Epstein JB, Emerton S, Le ND, Stevenson-Moore P. A double-blind crossover trial of Oral Balance gel and Biotene toothpaste versus placebo in patients with xerostomia following radiation therapy. Oral Oncol. 1999;35(2):132-7. Silvestre FJ, Minguez MP, Suñe-Negre JM. Clinical evaluation of a new artificial saliva in spray form for patients with dry mouth. Med Oral Patol Oral Cir Bucal. 2009 Jan 1;14(1):E8-E11. Itthagarun A, Wei SH. Chewing gum and saliva in oral health. J Clin Dent. 1997;8(6):159-62. Bots CP, Brand HS, Veerman EC, Korevaar JC, Valentijn-Benz M, et al. Chewing gum and a saliva substitute alleviate thirst and xerostomia in patients on haemodialysis. Nephrol Dial Transplant. 2005;20(3):578-84. Reynolds EC, Cai F, Shen P, Walker GD. Retention in plaque and remineralization of enamel lesions by various forms of calcium in a mouthrinse or sugar-free chewing gum. J Dent Res. 2003;82(3):206-11. ref Nuvora website. http://www.nuvorainc.com/salese-learn-more.html Afriamian D. Treating Xerostoma Utilizing an Adhesive Oral Tablet As Compared With Biotene Rinses. Data on file. Yamamoto K, Nagashima H, Yamachika S, Hoshiba D, Yamaguchi K, et al. The application of a night guard for sleep-related xerostomia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106(3):e11-4. Hirvikangas M, Posti J, Mäkilä E. Treatment of xerostomia through use of dentures containing reservoirs of saliva substitute. Proc Finn Dent Soc. 1989;85(1):47-50. Momm F, Volegova-Neher NJ, Schulte-Mönting J, Guttenberger R. Different saliva substitutes for treatment of xerostomia following radiotherapy. A prospective crossover study. Strahlenther Onkol. 2005 Apr;181(4):231-6. Author Profiles Dr. Jacalyn Neceskas is a pharmacist at the Cancer Institute of New Jersey, and graduated with a PharmD. Dr. Stacie Moore was a pharmacy resident at the Robert Wood Johnson University Hospital in New Brunswick and holds a PharmD. Dr. Susan Goodin graduated with a PharmD and is the director in the division of pharmaceutical sciences at the Cancer Institute of New Jersey and associate professor of medicine at the Robert Wood Johnson Medical School in New Jersey. Dr. Fiona M. Collins graduated with a dental degree from Glasgow University and holds an MBA and MA from Boston University. Disclaimer The author(s) of this course has/have no commercial ties with the sponsors or the providers of the unrestricted educational grant for this course. Reader Feedback We encourage your comments on this or any PennWell course. For your convenience, an online feedback form is available at www.ineedce.com. www.rdhmag.com 57 Online Completion Use this page to review the questions and answers. Return to www.ineedce.com and sign in. If you have not previously purchased the program select it from the “Online Courses” listing and complete the online purchase. Once purchased the exam will be added to your Archives page where a Take Exam link will be provided. Click on the “Take Exam” link, complete all the program questions and submit your answers. An immediate grade report will be provided and upon receiving a passing grade your “Verification Form” will be provided immediately for viewing and/or printing. Verification Forms can be viewed and/or printed anytime in the future by returning to the site, sign in and return to your Archives Page. Questions 1. It has been estimated that up to _________ of adults carry the herpes virus latently by age 30 and that _________ of carriers in the United States are under age 20. a. b. c. d. 60%; 20% 70%; 30% 80%; 40% 90%; 50% 2. _________ is an implicated factor/association for RAU. a. b. c. d. Hypersensitivity/sensitivity to foods/chemicals Medication use Genetics all of the above 3. RHL is caused by a _________with herpes simplex virus type 1. a. primary infection b. secondary infection c. tertiary infection d. none of the above 4. RHL is transmitted by _________. a. b. c. d. aerosols direct contact with the secretions from herpetic lesions sneezing and coughing all of the above 5. _________ is a potential trigger/stressor for periodic reactivation of HSV-1. a. b. c. d. UV light Anxiety/stress Dental treatment all of the above 6. _________ can play an important role in preventing recurrences of RHL a. b. c. d. Bitter aloe Sunscreen Lip salve all of the above 7. Recurrent aphthous ulcers _________. a. result in the appearance of a flat or cratered, grayishyellow area surrounded by a ring of inflamed tissue b. occur on nonkeratinized surfaces of the oral mucosa c. can cause moderate to severe pain d. all of the above 8. It is during the vesicle stage of RHL that the patient experiences _________. a. b. c. d. the highest viral load bacterial superinfection viral superinfection the lowest viral load 9. Patients with RHL should be advised to _________. a. wash their hands frequently to prevent the transmission of viral secretions and infection b. avoid triggers such as sunlight c. avoid spicy and/or acidic foods and drinks d. a and b 10. It is essential to stress the importance of visiting (or returning to) the dentist or physician if lesions do not heal within _________ days. a. 7 b. 10 c. 14 d. 21 58 11. _________ are the mainstay of palliative care for RAU. a. b. c. d. Prescription oral pastes and rinses Over-the-counter (OTC) oral pastes and rinses Corticosteroids none of the above 12. A mucosal adhesive patch containing citrus oil and magnesium chloride _________. a. b. c. d. has been shown to help relieve pain forms a barrier over the lesion to help protect it has been shown to reduce healing time all of the above 13. Pain-relieving topical analgesic pastes used for RAU typically contain _________. a. b. c. d. 10% benzocaine or 1% lidocaine 15% benzocaine or 2% lidocaine 20% benzocaine or 2% lidocaine none of the above 14. 5% amlexanox has been found to _________ , when applied 4 times daily. a. b. c. d. increase the rate of healing of RAU reduce the duration of pain provide only palliative relief a and b 15. 10% docosanol cream _________. a. b. c. d. has been found to reduce healing time has been found to reduce the time to cessation of pain is a nonprescription cream all of the above 16. Topical lysine has been shown to reduce healing time and to provide relief for ____. a. b. c. d. RAU RHL RAU and RHL none of the above 17. _________ is an FDA-approved prescription product for the treatment of RHL. a. b. c. d. Acyclovir cream Penciclovir cream Fanclover cream a and b 18. _________ are factors in the occurrence of xerostomia. a. b. c. d. Medication, alcohol and tobacco use Chemotherapy and head and neck radiation therapy Auto-immune diseases all of the above 19. _________ is a symptom of xerostomia. a. b. c. d. A sticky and/or dry feeling in the mouth Stringy or ropey saliva Difficulty speaking, chewing or swallowing All of the above 20. _________ can be a sign of xerostomia. a. The appearance of dryness of the oral mucosa and oral irritations b. An increased level of carious lesions c. An increased level of plaque and bad breath d. all of the above 21. If it is suspected that a patient may have xerostomia, _________will help objectively determine if xerostomia is present and to what degree. a. b. c. d. an unstimulated salivary flow test a visual analog scale a stimulated salivary flow test a and c www.rdhmag.com 22. The results of the ________of xerostomia are important to proper treatment of the patient. a. b. c. d. objective assessment subjective assessment objective and subjective assessments none of the above 23. If a mouth mirror sticks when placed against the buccal mucosa _________. a. b. c. d. this suggests enzymatic activity this is indicative of inadequate salivary flow this is indicative of adequate salivary flow a and c 24. Toothpastes specifically formulated for dry-mouth patients contain _________. a. b. c. d. lower levels of SLS or no SLS lower levels of zinc higher levels of antibacterial agents all of the above 25. Patients with xerostomia should be advised to avoid _________. a. consumption of sugar-containing foods, drinks, and snacks and other fermentable carbohydrates b. tobacco, caffeine, and alcohol c. alcohol-containing rinses d. all of the above 26. Xerostomia associated with mouthbreathing is _________. a. b. c. d. sometimes permanent always permanent always debilitating none of the above 27. _________ has been shown to help relieve the symptoms of dry mouth. a. b. c. d. Sipping water Chewing gum Sleeping with a humidifier all of the above 28. Mouthwashes for the treatment of xerostomia are formulated to effectively _________. a. b. c. d. help relieve dry mouth soothe the oral mucosa help cleanse the oral cavity, and combat halitosis all of the above 29. A small mucoadhesive patch used to treat xerostomia has been found to _________. a. b. c. d. effectively relieve dry mouth dissolve over 2-4 hours to moisturize the mouth increase whole salivary flow all of the above 30. Dry mouth can be relieved using _______. a. b. c. d. toothpastes, mouthwashes and saliva substitutes chewing gums and lozenges a mucoadhesive patch combinations of the above December 2010 ANSWER SHEET Part I: Quelling Cold Sores and Aphthous Ulcers Part I I: Relieving Xerostomia Name: Title: Address: E-mail: City: State: Telephone: Home ( ) Office ( Specialty: ZIP: ) Country: Lic. Renewal Date: Requirements for successful completion of the course and to obtain dental continuing education credits: 1) Read the entire course. 2) Complete all information above. 3) Complete answer sheets in either pen or pencil. 4) Mark only one answer for each question. 5) A score of 70% on this test will earn you 3 CE credits. 6) Complete the Course Evaluation below. 7) Make check payable to PennWell Corp. For Questions Call 216.398.7822 If not taking online, mail completed answer sheet to Educational Objectives Academy of Dental Therapeutics and Stomatology, Part I. A Division of PennWell Corp. 1. Listanddescribetheetiologyandpathophysiologyrelatedtorecurrentaphthousulcersandrecurrentherpeslabialis. 2. Listanddescribethegeneralrecommendationsspecifictopatientsexperiencingrecurrentherpeslabialis. 3. Listanddescribethetreatmentoptionsavailableforrecurrentaphthousulcersandrecurrentherpeslabialis. P.O. Box 116, Chesterland, OH 44026 or fax to: (440) 845-3447 For IMMEDIATE results, go to www.ineedce.com to take tests online. Answer sheets can be faxed with credit card payment to (440) 845-3447, (216) 398-7922, or (216) 255-6619. Part II. 1. List the etiological factors for xerostomia. 2. List and describe the signs and symptoms of xerostomia. Payment of $49.00 is enclosed. (Checks and credit cards are accepted.) 3. List and describe the treatment options available for the relief of dry mouth. If paying by credit card, please complete the following: MC Visa AmEx Discover Course Evaluation Pleaseevaluatethiscoursebyrespondingtothefollowingstatements,usingascaleofExcellent=5toPoor=0. 1. Were the individual course objectives met?Objective #1: Yes Objective #2: Yes No No NoO Yesbejcvti#e3: Objective #4:Yes No 2. To what extent were the course objectives accomplished overall? 5 4 321 0 3. Please rate your personal mastery of the course objectives. 5 4 321 0 4. How would you rate the objectives and educational methods? 5 4 3 210 5. How do you rate the author’s grasp of the topic? 5 4 3 210 6. Please rate the instructor’s effectiveness. 5 4 3 210 7. Was the overall administration of the course effective? 5 4 3 210 8. Do you feel that the references were adequate? Yes oN 9. Would you participate in a similar program on a different topic? Yes oN Acct. Number: _______________________________ Exp. Date: _____________________ Charges on your statement will show up as PennWell 10. Ifanyofthecontinuingeducationquestionswereunclearorambiguous,pleaselistthem. ___________________________________________________________________ 11. Was there any subject matter you found confusing? Please describe. ___________________________________________________________________ ___________________________________________________________________ 12. What additional continuing dental education topics would you like to see? ___________________________________________________________________ ___________________________________________________________________ AGD Code 016, 734, 739 PLEASE PHOTOCOPY ANSWER SHEET FOR ADDITIONAL PARTICIPANTS. AUTHOR DISCLAIMER The author(s) of this course has/have no commercial ties with the sponsors or the providers of the unrestricted educational grant for this course. SPONSOR/PROVIDER This course was made possible through an unrestricted educational grant. No manufacturer or third party has had any input into the development of course content. All content has been derived from references listed, and or the opinions of clinicians. Please direct all questions pertaining to PennWell or the administration of this course to Machele Galloway, 1421 S. Sheridan Rd., Tulsa, OK 74112 or [email protected]. COURSE EVALUATION and PARTICIPANT FEEDBACK We encourage participant feedback pertaining to all courses. Please be sure to complete the survey included with the course. Please e-mail all questions to: [email protected]. INSTRUCTIONS All questions should have only one answer. Grading of this examination is done manually. Participants will receive confirmation of passing by receipt of a verification form. Verification forms will be mailed within two weeks after taking an examination. EDUCATIONAL DISCLAIMER The opinions of efficacy or perceived value of any products or companies mentioned in this course and expressed herein are those of the author(s) of the course and do not necessarily reflect those of PennWell. Completing a single continuing education course does not provide enough information to give the participant the feeling that s/he is an expert in the field related to the course topic. It is a combination of many educational courses and clinical experience that allows the participant to develop skills and expertise. COURSE CREDITS/COST All participants scoring at least 70% on the examination will receive a verification form verifying 3 CE credits. The formal continuing education program of this sponsor is accepted by the AGD for Fellowship/Mastership credit. Please contact PennWell for current term of acceptance. Participants are urged to contact their state dental boards for continuing education requirements. PennWell is a California Provider. The California Provider number is 4527. The cost for courses ranges from $29.00 to $110.00. Many PennWell self-study courses have been approved by the Dental Assisting National Board, Inc. (DANB) and can be used by dental assistants who are DANB Certified to meet DANB’s annual continuing education requirements. To find out if this course or any other PennWell course has been approved by DANB, please contact DANB’s Recertification Department at 1-800-FOR-DANB, ext. 445. Customer Service 216.398.7822 RECORD KEEPING PennWell maintains records of your successful completion of any exam. Please contact our offices for a copy of your continuing education credits report. This report, which will list all credits earned to date, will be generated and mailed to you within five business days of receipt. CANCELLATION/REFUND POLICY Any participant who is not 100% satisfied with this course can request a full refund by contacting PennWell in writing. © 2010 by the Academy of Dental Therapeutics and Stomatology, a division of PennWell QUANTDEC10RDH 59