* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Complaint - Psych
David J. Impastato wikipedia , lookup
Major depressive disorder wikipedia , lookup
Mental health professional wikipedia , lookup
Emergency psychiatry wikipedia , lookup
Moral treatment wikipedia , lookup
History of psychiatry wikipedia , lookup
History of mental disorders wikipedia , lookup
History of psychiatric institutions wikipedia , lookup
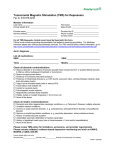
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 1 of 35
UNITED STATES DISTRICT COURT
FOR THE DISTRICT OF CONNECTICUT
CHRISTOPHER MEIDL, on his own behalf
and on behalf of all others similarly situated,
Plaintiff,
v.
)
)
)
)
)
)
AETNA, INC., AETNA LIFE INSURANCE COMP ANY )
and MCMC, LLC,
)
Defendants.
)
)
CLASS ACTION COMPLAINT
Plaintiff Christopher Meidl ("Plaintiff'), complains as follows on his own behalf and on
behalf of all others similarly situated, against Defendants Aetna, Inc. and Aetna Life Insurance
Company (collectively "Aetna"), and MCMC, LLC ("MCMC" and, collectively with Aetna,
"Defendants").
INTRODUCTION
1.
Plaintiff is a beneficiary in a health insurance plan issued on behalf of Marsh &
McLennan Companies (the "Meidl Plan"), a group health benefit plan sponsored by the privatesector employer of Plaintiffs wife. The Meidl Plan is governed by the Employee Retirement
Income Security Act ("ERISA"), 29 U.S.C. § 1001, et seq., and is administered by Aetna.
2.
Plaintiff suffers from Major Depressive Disorder, which has not been alleviated
by psychotherapy or administration of anti-depressant medication. In 2013, Plaintiff's treating
mental health care providers recommended that Plaintiff undergo therapeutic repetitive
NeuroStar Transcranial Magnetic Stimulation ("TMS") therapy. Aetna, however, denied
Plaintiff's request for pre-authorization of TMS therapy on the ground that it fell under an
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 2 of 35
exclusion in the Meidl Plan entitled "Experimental or Investigational Services or Unproven
Services" (the "E/I Exclusion").
3.
Following Aetna's denial of coverage, Plaintiff exhausted all internal appeals
provided by the Meidl Plan. Aetna responded to each level of appeal by upholding the denial of
coverage based solely on its internal policy, and without considering the substantial materials
submitted by Plaintiff and his providers supporting coverage for TMS. Thereafter, Plaintiff filed
an external appeal with MCMC, a so-called "Independent Review Organization" ("IRO"), which
upheld the denial based on Aetna's coverage policy.
4.
In denying coverage, Aetna followed its uniform TMS Medical Policy, that
mandates denial of coverage for TMS therapy for all Aetna-administered plans. In tum, MCMC
rubber-stamped Aetna's denial without conducting a true independent evaluation of whether
TMS is a proven and effective treatment for Major Depressive Disorder. Neither Aetna nor
MCMC properly applied the E/I Exclusion found in the Meidl Plan.
5.
TMS is a non-invasive procedure that uses an electromagnet to generate repeated
pulsed magnetic fields that stimulate nerve cells in the region of the brain associated with mood
control, thereby improving symptoms of depression. Unlike electroconvulsive therapy
("ECT")-sometimes known as electro-shock therapy- in which an outside electric current is
applied to the brain via electrodes, TMS only induces electrical activity within the brain, and
does not cause seizures or the related side effects.
6.
There is overwhelming evidence that TMS is safe and effective and is a generally
accepted standard of medical practice for the treatment of depression within the mental health
community: TMS has been around and well-accepted for over 20 years; the Food and Drug
Administration ("FDA")
has approved TMS for Major Depressive Disorder; the American
2
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 3 of 35
Psychiatric Association and other nationally-recognized medical organizations, and numerous
meticulous peer-reviewed studies have validated the safety and effectiveness of TMS; hundreds
of respected mental health facilities and providers, including UCLA, the Harvard Medical
System, Boston Medical Center, Johns Hopkins University, Cornell University, Boston
University, and Brown University, recommend and use TMS on a regular basis; and many
insurers, including Medicare, UnitedHealthcare, Anthem, Health Care Service Corporation, and
nearly 25 independent Blue Cross/Blue Shields cover TMS as a safe and effective treatment for
refractory Major Depressive Disorder and that it is not "experimental."
7.
TMS therapy is, therefore, a proven, efficacious treatment for depression, and is
not experimental or investigational by any fair definition of those terms, and certainly not within
the meaning of those terms as defined in the Meidl Plan or in similar Aetna-administered plans .
Aetna's TMS Medical Policy, and Defendants' resulting denial of TMS coverage for Plaintiff
and members of the Classes he seeks to represent (as defined below), violated the terms of the
relevant plans and Defendants' fiduciary obligations under ERISA.
8.
Under ERISA, Plaintiff and the members of the Classes are entitled to equitable
and declaratory relief enjoining application of Aetna's erroneous medical policy, reversing
Defendants' benefits denials of coverage for TMS therapy, and awarding such other relief and
the Court finds appropriate.
THE PARTIES
9.
Plaintiff resides in Franklin, Tennessee .
10.
Defendant Aetna Inc. is a Pennsylvania corporation headquartered at 151
.
Farmington Avenue, Hartford, Connecticut. Aetna Inc. is a global health care benefits company,
which, along with its wholly-owned and controlled subsidiaries, offers, insures, underwrites, and
3
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 4 of 35
administers health benefits plans, including Plaintiffs health benefits plan, as detailed herein.
Aetna Inc. and its subsidiaries are referred to as "Aetna" in this Complaint.
11.
Defendant Aetna Life Insurance Company ("ALIC") is a Connecticut corporation
with its principal business address at 151 Farmington Avenue, Hartford, CT 06156. ALIC is a
wholly-owned subsidiary of Aetna Inc. It is the lead operating entity for Aetna's branded life and
health insurance organization.
12.
Defendant MCMC is a Delaware limited liability managed care services company
headquartered at 300 Crown Colony Drive, Suite 203, Quincy, Massachusetts 02169. One of
MCMC's "primary processing centers" is located in Danbury, Connecticut. MCMC is registered
as a limited liability company with the Connecticut Secretary of State to do business in
Connecticut. Among other things, MCMC directly contracts with Aetna and other insurers to
serve as an IRO to adjudicate external appeals pursued by Aetna insureds or their providers.
JURISDICTION AND VENUE
13.
Defendants' actions in administering employer-sponsored health care plans,
making coverage and benefit determinations under the terms and conditions of the health care
plans, and/or processing appeals of coverage and benefit determinations under the terms and
conditions of the health care plans are governed by ERISA. This Court has jurisdiction of this
case under 28 U.S.C. § 1331 (federal question jurisdiction) and 29 U.S.C. § 1132(e) (ERISA).
14.
Venue is appropriate in this District because Aetna, Inc. is incorporated and has
its registered office located in here. Additionally, Defendants conduct significant operations in
this District and are registered with the Commonwealth of Pennsylvania to do so.
FACTUAL ALLEGATIONS
15.
The majority of the health plans underwritten and/or administered by Aetna,
4
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 5 of 35
including the Meidl Plan, are employee welfare benefit plans sponsored by private-sector
employers governed by ERISA ("ERISA plans").
16.
During all relevant times, Aetna acted as a fiduciary with respect to its
administration of ERISA plans. In particular, Aetna interpreted and applied ERISA plan terms,
made coverage and benefit decisions under the ERISA plans within its sole discretion, and
provided payment under the ERISA plans to participants/beneficiaries and their providers.
Accordingly, Aetna was required to comply with the requirements ERISA imposes on
fiduciaries.
17.
In serving in the capacity of an IRO for external appeals from Aetna's coverage
and benefit decisions under the ERISA plans, MCMC also acted as an ERISA fiduciary, in that it
was vested with discretion to make final benefit determinations as to such external appeals. In
that capacity, MCMC was also responsible for interpreting and applying ERISA plan terms,
making coverage and benefit decisions, and authorizing payments to participants/beneficiaries
and their providers. In fulfilling this responsibility, MCMC therefore was required to comply
with the requirements ERISA imposes on fiduciaries.
18.
The health insurance plans administered by Aetna are either fully-insured or self-
funded. With respect to fully-insured plans, Aetna both administers the plan by making all
benefit determinations and pays the benefits out of its own assets. With respect to self-funded
plans, Aetna administers the plan, but the underlying plan sponsor or employer through which
the insurance is provided is ultimately responsible for reimbursing Aetna for the benefit
payments.
19.
When processing benefits for a self-funded plan, Aetna makes all benefit
determinations and authorizes benefit checks to be issued out of bank accounts which Aetna
5
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 6 of 35
controls. Periodically, Aetna will notify the sponsors of the self-funded plans of the need to
replenish their accounts so that benefits can be paid. But Aetna nevertheless continues to control
these accounts and is fully responsible for processing the insurance claims and making the
determination whether to issue the check from these accounts.
20.
Thus, irrespective of whether a particular ERJSA plan is fully-insured or self-
funded, Aetna is the proper party for Plaintiff, and the putative class, to sue because Aetna - not
the underlying plan sponsor or employer - made all the relevant decisions and wielded the
authority to issue benefit checks under the ERJSA plans.
21.
The only exception to Aetna's control over benefit determinations is a situation in
which Aetna denies a claim and the relevant insured elects to pursue an external appeal with an
IRO. In this situation, Aetna agrees to comply with the decision of the IRO (which it self-selects
and with which it directly contracts), such as MCMC, but only with regard to the specific
decision from which the appeal was taken. As a result, even if an IRO disagrees with a particular
Aetna medical policy and approves coverage for a specific claim, Aetna will continue to apply its
medical policy going forward with regard to similar claims.
The Meidl Plan
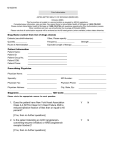
22.
The Meidl Plan is a self-funded plan, meaning that the plan sponsor, Marsh &
McLennan, is responsible for reimbursing Aetna for the benefit payments. However, Aetna
maintains control over the decision-making process and is ultimately responsible for authorizing
the issuance of checks for paying benefits.
23.
As a beneficiary to the Meidl Plan, Plaintiff was issued the Marsh & McLennan
"Benefit Handbook," entitled "Aetna Medical Plan Options - March & McLennan Companies."
The Benefit Handbook, which is a plan document governing his insurance that details the terms
6
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 7 of 35
and conditions of the Meidl Plan, defines "Covered Service(s)" as "Medically necessary health
services provided for the purpose of preventing, diagnosing or treating a sickness, injury, mental
illness, substance abuse, or their symptoms."
24.
In addition, the Benefit Handbook includes a list of "Exclusions," which are
deemed to be services which are not covered under the Meidl Plan. One such Exclusion is
entitled "Experimental or Investigational Services or Unproven Services" (the "E/I Exclusion").
The E/I Exclusion states as follows:
Medical, surgical, diagnostic, psychiatric, substance abuse or health care services,
technologies, supplies, treatments, procedures, drug therapies or devices that, at
the time the Claims Administrator makes a determination regarding coverage in a
particular case, are determined to be any of the following:
•
•
•
25.
Not approved by the US Food and Drug Administration (FDA) to be
lawfully marketed for the proposed use and not identified in the American
Hospital Formulary Service or the United States Pharmacopeia Dispensing
Information as appropriate for the proposed use;
Subject to review and approval by any institutional review board for the
proposed use;
The subject of an ongoing clinical trial that meets the definition of a Phase
1, 2 or 3 clinical trial set forth in the FDA regulations, regardless of
whether the trial is actually subject to FDA oversight.
The last two criteria under the E/I Exclusion, relating to an Institutional Review
Board or clinical trials, are not relevant to the NeuroStar TMS Therapy system. TMS therapy is
not subject to other institutional approval before it can be used. It is similarly not the subject of
an ongoing Phase 1, 2 or 3 clinical trial. Thus only the first criterion, relating to FDA approval,
bears on whether or not the E/I Exclusion applies.
26.
On October 8, 2008, the FDA approved the NeuroStar TMS Therapy system, and
designated it as a Class II Device for the treatment of Major Depressive Disorder. This
classification was codified at 21 C.F.R. § 882.5805, and describes TMS as "an external device
that delivers transcranial repetitive pulsed magnetic fields of sufficient magnitude to induce
7
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 8 of 35
neural action potentials in the prefrontal cortex to treat the symptoms of major depressive
disorder without inducing seizure in patients."
27.
Thus, at least as of October 8, 2008, the NeuroStar TMS Therapy system no
longer fit within the E/I Exclusion to the Meidl Plan.
28.
The denials at issue in this case relate to Aetna's E/I Exclusion. In applying this
policy, Defendants did not make a Medical Necessity determination, but only determined that
TMS is not covered as "experimental, investigational or unproven."
Defendants' Denial of Coverage for Plaintifrs TMS Therapy
29.
Plaintiff has been in treatment for chronic depression and anxiety disorder for
many years. While Plaintiffs doctors attempted to treat him with a variety of anti-depressant
medications as well as traditional outpatient therapy and other modalities, including ECT, all
these treatments proved ineffective in alleviating Plaintiffs long-term symptoms.
30.
Accordingly, in early 2013, Plaintiffs treating providers recommended that he
receive treatment using the NeuroStar TMS Therapy system.
31.
Although the Meidl Plan did not require Plaintiff to receive preauthorization from
Aetna, his psychiatrist wanted to verify coverage before Plaintiff incurred the expense and
therefore sought confirmation from Aetna that it would cover TMS. Aetna informed the
provider, however, that it deemed TMS to be excluded from the Meidl Plan pursuant to the E/I
Exclusion.
32.
By letter dated February 15, 2013, Plaintiff wrote to Aetna's Member Appeals
department, requesting that Aetna reconsider its denial of coverage of TMS for treatment of
depression. In support of his request, Plaintiff included several letters from his treating providers,
each of whom recommended that Plaintiff receive TMS therapy.
8
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 9 of 35
33.
In a letter dated January 8, 2013, Deb Leinart LPC, MHSP, CSAT, one of
Plaintiffs therapists, recommended that Plaintiff receive TMS with the following statement:
I am writing to support insurance coverage for Mr. Meidl to receive Trans-cranial
Magnetic Stimulation (TMS). I have seen Mr. Meidl since 6/5/2012 for
longstanding chronic depression, anxiety disorder, PTSD, eating disorder and
history of abuse. Mr. Meidl has been proactive in his willingness to participate in
therapy to address these concerns. He recently attended an inpatient eating
disorder treatment program where he was successful in addressing the compulsive
overeating, binging/purging, and some of the PTSD symptoms. Mr. Meidl is
compliant with his treatment plan of seeing a nutritionist, taking prescribed
medication, appointments with his psychiatrist, attending support meetings and
being involved in outpatient therapy. However, what remains is the chronic
depression and high levels of anxiety that traditional outpatient therapy and other
therapeutic interventions have had minimal impact on reducing.
Mr. Meidl has a history of self-harm behavior and suicidal ideation which is
exasperated by the diagnosed clinical depression and anxiety disorder. In addition
the status of Mr. Meidl's personal relationships have become extremely
problematic since the inception of this diagnosis.
With the support of his psychiatrist Dr. Cochran and other members of his
therapeutic team the treatment of Trans-cranial Magnet Stimulation (TMS) has
been recommended. I concur with this recommendation and advocate for Mr.
Meidl to receive insurance support for this treatment.
34.
In a letter dated January 15, 2013, Harrison H. Taylor, LCSW, another of
Plaintiffs therapists, added:
I am Chris Meidl's primary therapist. I am writing in support of him receiving
Transcranial Magnetic Stimulation (TMS). I believe that this is a good additional
treatment option to treat his longstanding, and treatment resistant, depression. I
strongly recommend that Aetna be in support of this treatment.
35.
In a letter dated February 12, 2014, Alistair J. Finlayson, M.D., Plaintiffs treating
psychiatrist, further stated:
This letter is in support of your request for Transcranial Magnetic Stimulation
therapy for longstanding symptoms of anxiety and depression that have responded
incompletely to other forms of therapy.
36.
Additionally, Michelle Cochran, MD, a board-certified psychiatrist and the
9
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 10 of 35
Medical Director of the Neuroscience & TMS Treatment Center in Nashville, Tennessee, the
facility that would be providing the TMS therapy to Plaintiff, wrote Aetna a letter dated January
28, 2013, to support Plaintiff's request for coverage. In the letter, Dr. Cochran rejected Aetna's
conclusion that TMS "is not covered to the extent that it is determined to be
experimental/investigational and is an excluded benefit under the patient's plan," since
"NeuroStar TMS Therapy is a safe and effective treatment that improves depressive symptoms
for those patients diagnosed with Major Depressive Disorder that have not benefited from prior
antidepressant medication." Dr. Cochran added that "Aetna's decision does not reflect recent
medical research, published treatment guidelines, and current psychiatric practice."
37.
As described in Dr. Cochran's letter, the NeuroStar TMS Therapy system was
approved by the FDA in October 2008, with an indication "for the treatment of Major Depressive
Disorder in adult patients who have failed to achieve satisfactory improvement from one prior
antidepressant medication at or above the minimal effective dose and duration in the current
episode," a condition that Plaintiff easily satisfied. Dr. Cochran further detailed, with numerous
references, multiple studies demonstrating the effectiveness and safety of TMS. She concluded
by reporting her strong belief "that NeuroStar TMS Therapy is medically necessary and the most
effective treatment option at this time based upon this patient's specific medical history and the
clinical data present."
38.
Despite the substantial support for TMS that Plaintiff provided to Aetna, Aetna
rejected Plaintiff's request for reconsideration of its denial and concluded that TMS was not
covered, stating in an April 18, 2013, letter:
We reviewed the information you submitted as well as the provisions of the plan
and our current coverage guidelines. Based on these reviews, we have not
changed our prior position and it does not appear that the proposed services will
be eligible for coverage.
10
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 11 of 35
The member's plan does not require pre-service approval, so your request for a
reconsideration review is not considered a claim under ERISA. Therefore, there is
no formal right to appeal this evaluation decision under ERISA or under the plan.
There are no further reviews or reconsiderations available to you.
39.
After Aetna denied pre-approval for TMS, Plaintiff elected to receive the
treatment anyway, based on the recommendations of five mental health providers, including
three treating providers. He obtained the services from August 8, 2013, through October 9, 2013,
for which he paid several thousand dollars out of pocket, and then submitted his claim to Aetna
for reimbursement.
40.
Aetna again denied the claim for TMS therapy, relying on its internal policy that
deemed TMS to fall within the Ell Exclusion.
41.
Plaintiffs TMS therapy did not meet the narrow terms of the Ell Exclusion in the
Meidl Plan. The FDA approved NeuroStar's TMS Therapy system for the treatment of Major
Depressive Disorder in October 2008. As noted above, TMS therapy is not subject to other
institutional approval before it can be used and is not the subject of an ongoing Phase 1, 2 or 3
clinical trial. Thus, Aetna's decision finding TMS to be "experimental and investigational" under
the Meidl Plan was clearly erroneous, arbitrary, and capricious.
42.
Plaintiff and Dr. Cochran, who administered Plaintiffs TMS treatment, both
appealed that denial. Dr. Cochran resubmitted detailed summaries of the research showing that
TMS was generally accepted within the mental health community as being safe and effective. In
a November 13, 2013, letter accompanying Dr. Cochran's appeal, Plaintiff pointed out how
successful the treatment had been, stating:
As I considered the array of treatments and interventions I have received, TMS
has far and away yielded the most dramatic reduction of my symptoms. I sleep
better. My cognitive functioning is improved overall. I am better able to manage
my nearly incapacitating internal stress and debilitating anxiety that has plagued
11
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 12 of 35
me much of my life. I have a renewed interest in family and friends. Relationships
that have been maintained by thin threads are being rewoven. After years of
barren landscape, I am finding energy to pursue things that interest me and things
in life that need to get done. Contrast that with extended periods of time,
sometimes months on end, where it seemed impossible to get out of bed, much
less do anything of interest or go outside. Simply put, my depression and the deep
pit of despair on which I have teetered and into which I have fallen for many
years have been nearly, if not completely, eliminated. They are 'filled in,' as it
were. It seems almost miraculous. If there is such a thing, I think I may actually
feel somewhat normal.
43.
In response to Dr. Cochran's separate appeal, which she submitted to Aetna on
November 18, 2013, Aetna responded on December 20, 2013, that Plaintiff needed to complete
and sign an Authorized Representative Designation form to allow Dr. Cochran to appeal on
Plaintiffs behalf. Plaintiff submitted such a form on December 30, 2013, which explicitly named
Dr. Cochran "to act as my authorized representative in requesting an appeal from Aetna"
regarding the denial of coverage for TMS therapy.
44.
By letter dated January 14, 2014, Dr. Cochran submitted a supplemental letter in
support of the appeal in which she attached coverage policies from 16 different insurers which
found TMS to be generally accepted in the medical community as safe and effective and, thus,
covered under their respective plans.
45 .
Aetna denied the appeal by letter from its Customer Resolution Team dated
January 31, 2014. In the denial letter, Aetna noted that its original denial was based on "denial
codes" 789 and 557, with the following explanation:
A service or supply furnished by a particular provider is covered if Aetna
determines that it is appropriate for the diagnosis, care or treatment of the disease
or injury. In determining if a service or supply is appropriate, Aetna will take into
account if the service is generally recognized according to professional standards
of safety and effectiveness in the United States for diagnosis, care or treatment.
This service does not meet this requirement of your plan of benefits and is
excluded from coverage.
12
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 13 of 35
46.
Aetna then stated that it was upholding the denial, providing the following
statement:
In your appeal, you requested reconsideration of Mr. Meidl's TMS treatments
from August 08, 2013 to October 09, 2013. You provided documentation on the
test as well as multiple letters of support.
An Aetna medical director, board certified in psychiatry, a complaint and appeal
nurse, and a complaint and appeal analyst, who were not involved in the original
denial decision, have reviewed your appeal request, including all supporting
documentation submitted to date.
According to Aetna's CPB [Coverage Policy Bulletin] #469, Transcranial
Magnetic Stimulation and Cranial Electrical Stimulation, Aetna considers TMS
experimental and investigational for the diagnosis and treatment of major
depression, other neuropsychiatric disorders (e.g., schizophrenia, anxiety
disorders, panic disorder, and obsessive-compulsive disorder) or any other
indications (e.g., chronic pain, migraine headaches, spasticity, Tourette syndrome,
tinnitus, and levodopa-induced dyskinesia) because its value and effectiveness in
these roles has not been established.
Note: Our decision is limited to whether the health care services are a covered
benefit under this member's health care plan. This decision did not include a
medical necessity determination. Items and services that are denied because they
are not a benefit under the member's plan or because of administrative
requirements were not met are not reviewed for medical necessity.
Please refer to the member's SPD [Summary Plan Description] under the section
titled What's Not Covered, which states,
"Health services and supplies that do not meet the definition of a Covered
Service."
Based on the information described above, we are upholding the original
determination.
47.
Notably, in denying coverage, Aetna failed to discuss or even acknowledge the
information provided by Dr. Cochran and Plaintiff supporting TMS, including the many studies
verifying its safety and efficacy and the coverage policies of numerous other insurers, which
recognize and reimburse TMS. Thus, Aetna provided Plaintiff with no basis for its negative
coverage determination aside from its reliance- to the exclusion of all contrary evidence-on
13
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 14 of 35
Aetna's pre-existing policy that TMS falls under the E/I Exclusion.
48.
According to Aetna's letter upholding the denial, Aetna based its decision on a
clause in the "SPD" which states that services are not covered which "do not meet the definition
of a Covered Service." This provision, actually found in a document titled "Benefit Handbook,"
is listed under a heading "All Other Exclusions," which detailed various exclusions applicable to
the Meidl Plan. Significantly, Aetna failed to cite to the applicable provision of the Benefit
Handbook.
The "Covered Service" provision of the Benefit Handbook merely defines
"medically necessary" services, and does not include the E/I Exclusion, which is a separate
provision. However, Aetna's denial did not include a medical necessity determination regarding
Plaintiffs TMS therapy, but rather relied solely on the E/I Exclusion.
49.
Indeed, the Glossary definition of "Covered Service(s)" in the Benefits Handbook
further confirms that Aetna' s application of its E/I Exclusion to TMS is improper. The definition
states: "Decisions about whether to cover new technologies, procedures and treatments will be
consistent with conclusions of prevailing medical research based on well-conducted randomized
trials or group studies." While TMS is not a "new" technology, but has been around and wellaccepted for twenty years, the use of TMS as a safe and effective treatment for depression is
entirely consistent with "prevailing medical research," based on numerous "well-conducted
randomized trials or group studies" which Aetna has persistently ignored when applying its Ell
Exclusion to deny coverage for TMS therapy to Plaintiff and the class he seeks to represent.
50.
By letter dated February 7, 2014, Plaintiff filed a second level appeal with Aetna.
51.
Dr. Cochran followed up on February 28, 2014 with an appeal letter of her own.
In this letter, Dr. Cochran detailed why the FDA-approved NeuroStar TMS Therapy "was the
safest and most effective treatment option" for Plaintiff. Dr. Cochran first demonstrated that
14
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 15 of 35
TMS therapy satisfies the five criteria used by the Blue Cross Blue Shield Technology
Evaluation Center ("BCBS TEC") to assess if a treatment is generally accepted and thereby
should be covered treatment:
•
The NeuroStar TMS Therapy had been approved by FDA to treat depression when an
adult patient failed to received "satisfactory improvement" from one antidepressant
medication, and Plaintiff "had failed for more than 20 antidepressant trials which did not
cause remission of his symptoms";
•
Scientific studies have proven "the acute safety and efficacy of TMS Therapy, including
through "two independent level one trials" which Dr. Cochran explicitly identified, as
well as many other studies demonstrating the efficacy ofTMS;
•
Scientific studies have proven that the benefits of TMS far outweigh any potential risks,
including through the results of two Level 1 sham-controlled randomized studies which
"provide consistent data documenting that TMS Therapy using a specific NeuroStar
treatment protocol results in significant improvement in acute depression" and that "the
health benefits of TMS Therapy outweigh the risks, therefore meeting the criterion that
TMS improves net health outcome";
•
Scientific studies have proven that TMS is "as beneficial as the established alternative
treatments," a conclusion reinforced here where Plaintiff did not achieve success through
medication or other treatments and "there is adequate evidence that TMS is at least as
effective as antidepressant drug therapy in treating depression," such that "TMS Therapy
presents a strong benefit to risk ration"; and
•
TMS Therapy has been proven safe and effective outside of investigational settings,
given that it "is now in widespread clinical use across the country at over 500
centers/offices, including institutions such as the Mayo Clinic - Rochester, University of
Michigan Depression Center of Excellence, Walter Reed Army Hospital, Brown
University, UCLA, the Harvard medical system, Boston Medical Center, Johns Hopkins
University, Cornell University, Loma Linda University, Sheppard Pratt Center for
Anxiety and Depression, the Linder Center of Hope, and at freestanding psychiatric
hospitals and private physician's offices."
52.
In addition, citing numerous other studies, Dr. Cochran argued that "there is
strong evidence to support long term durability, efficacy, and safety of' TMS Therapy. Dr.
Cochran specifically noted the benefits of TMS Therapy compared to the alternative of ECT, in
which electric currents are passed through the brain, intentionally triggering a brief seizure, an
15
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 16 of 35
invasive treatment Plaintiff had previously undergone, without success. As Dr. Cochran pointed
out, studies demonstrate that ECT' s "efficacy and durability of effect may be limited" and its
adverse effects are worse than TMS: "TMS has a more benign safety profile than ECT and does
not include the complications associated with anesthesia, the cardiac risks, or the risks of
cognitive disturbance," including memory loss.
53.
Taking all of the evidence together, and applying it to Plaintiffs mental health
history and the failure of numerous prior treatment efforts, Dr. Cochran concluded that "TMS
Therapy was the safest and most effective treatment option for my patient at the time of
treatment." She further asked Aetna "to consider the fact that [Plaintiff] has not benefited from
multiple exposures to psychopharmacologic agents" and other treatments, including "failed trials
of: ECT in 2003 with side effects of memory problems resulting; [f]ailures of SSRis pre-date
ECT (Celexa, Luvox, Zoloft); failures of SNRis (Effexor XR up to 450 mg, Cymbalta); failures
of Serzone, Remeron & Trazodone; failures of augmentation with Seroquel, Risperdal, Abilify,
Lithium, Lamictal, and Adderall." In contrast to those failed treatments, Plaintiff "responded
well to TMS Therapy with a marked reduction in symptoms and tolerated the treatments well
with no side effects," while experiencing "additional benefits such as a highly improved level of
daily functioning, and increased socialization."
54.
Finally, Dr. Cochran requested that, in order for Aetna to comply with mandatory
URAC (an independent nonprofit organization, formerly known as the Utilization Review
Accreditation Commission, that accredits healthcare organizations) standards and to ensure a full
and fair review, the reviewer of the appeal be a board certified psychiatrist with education and
training "in the clinical management of patients with mood disorders, including complicated and
treatment-resistant
Major Depressive Disorder," and
16
in "neuoromodulation treatment
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 17 of 35
modalities," including Vagus Nerve Stimulation ("VNS") and ECT. Dr. Cochran also asked that
the reviewer have completed "a TMS clinical training program for use of a FDA-cleared TMS
delivery system."
55.
Notwithstanding the clear and definite evidence presented by Dr. Cochran and
other providers in support of the safety and efficacy of TMS in general, and its proven
effectiveness for Plaintiff, Aetna denied the second level appeal by letter dated March 15, 2014.
It also failed to respond to Dr. Cochran's request to use a reviewer with proper TMS-related
training and experience. The substantive portion of the denial letter (excerpted in full) stated:
Our decision
Based on our review of the above information [detailing all the information
provided by Plaintiff and his providers as well as Aetna CPB #469 and the Benefit
Handbook], we are upholding the previous decision to deny benefits for the TMS
treatments.
How we made our decision
You are appealing the denial that treatment was considered experimental. You as
well as your provider and experts disagree. You have enclosed additional material
for reconsideration.
According to Aetna's CPB #469, Transcranial Magnetic Stimulation and Cranial
Electrical Stimulation, Aetna considers TMS experimental and investigational for
the diagnosis and treatment of major depression, other neuropsychiatric disorders
(e.g., schizophrenia, anxiety disorders, panic disorder, and obsessive-compulsive
disorder) or any other indications (e.g., chronic pain, migraine headaches,
spasticity, Tourette syndrome, tinnitus, and levodopa-induced dyskinesia) because
its value and effectiveness in these roles has not been established. This decision
was made utilizing Aetna's CPB #469. You may obtain a copy of this CPB.
Our decision is limited to whether the health care services are a covered benefit
under your health care plan. This decision did not include a medical necessity
determination. Items and services that are denied because they are not a benefit
under the member's plan or because of administrative requirements were not met
are not reviewed for medical necessity.
56.
In the letter, Aetna then referred to "your plan material under topic 'What's Not
Covered' lists," this time quoting the proper section of "Experimental or Investigational
17
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 18 of 35
Services or Unproven Services." Once again, Aetna provided no further explanation or analysis
as to why the E/I Exclusion applied to TMS Therapy. Instead, Aetna merely stated: "A medical
director, board certified in adult psychiatry and child/adolescent psychiatry, and complaint and
appeal analysts, who were not involved in any prior decision, participated in the review of the
appeal." Thus, Aetna issued its decision by repeating virtually verbatim that language used in its
denial of the first level of appeal, and failed to acknowledge or rebut any of the analysis provided
by Plaintiff, Dr. Cochran or other providers concerning why TMS Therapy should be covered.
Aetna engaged in no discretionary analysis of the facts, but simply applied in a formalistic way
Aetna's pre-existing policy under CBP #469 that TMS is "experimental and investigational."
57.
Aetna's March 15, 2014 denial of Plaintiffs second level appeal exhausted his
internal remedies available to challenge Aetna's benefits denial. Aetna notified Plaintiff that he
had "the right to bring a civil action under Section 502(a) of ERISA," or, prior to doing so, to
pursue an "external review." According to Aetna, "[e]xternal reviews are conducted by
independent physicians with expertise in the medical service or supply at issue," and who "have
no association with [Aetna]." Aetna further confirmed that "[o]nce a review is complete, Aetna
accepts the decision of the external reviewer."
58.
In an effort to avoid litigation and with the (false) hope of receiving an impartial
review of Aetna's denials, Plaintiff requested an external review by letter dated May 29, 2014.
Aetna assigned Plaintiffs external appeal to its self-selected, contracted "Independent" Review
Organization, Defendant MCMC, which it identified in a June 3, 2014 letter as Medical Care
Management Corporation.
59.
In facilitating the MCMC appeal, Aetna prepared a Clinical Case Summary
relating to Plaintiffs claim, dated June 5, 2014. In it Aetna noted that Plaintiff had a diagnosis of
18
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 19 of 35
296.33, a code representing "major depressive disorder, recurrent episode, severe degree, without
mention of psychotic behavior." Summarizing Patient's medical history, Aetna reported:
Member w/long standing treatment resistant depression who underwent TMS
August 8, 2013 - October 9, 2013 - denied experimental and investigational
(E&I) .... Records outline compliance with medications and outpatient therapy,
w/depressive symptoms persisting. The member describes a history of treatment
including inpatient/outpatient care, ECT, talk therapy, CBT, DBT, EMDR,
mindfulness training, IFS, hypnosis, psycho-drama, and experimental therapy.
Due to the history of self-harm behavior, SI, and treatment resistant depression,
TMS was recommended.
60.
Aetna then detailed the "Denial Rationale" relating to its adverse benefit
determination, stating:
As per Aetna's Clinical Policy Bulletin (CPB) #0469: Transcranial Magnetic
Stimulation and Cranial Electrical Stimulation (Reviewed 08/289/2012) and the
Summary Plan Description (SPD) for March & McLennan Companies, the
requested serves were denied E/I.
Aetna considers TMS E&I for the diagnosis and treatment of major depression,
other neuropsychiatric disorders (e.g., schizophrenia, anxiety disorders, panic
disorder, and obsessive-compulsive disorder) or any other indication (e.g., chronic
pain, migraine headaches, spasticity, Tourette syndrome, tinnitus, and levodopainduced syskinesia) because its value and effectiveness in these roles has not been
established SPD: experimental: page 33 (what's not covered).
61.
By letter dated June 6, 2014, Aetna forwarded to MCMC a series of documents it
had regarding Plaintiffs request for coverage of TMS and related appeals, dating from early
2013 through June 2014, as well as Aetna's CPB #469 and the Marsh & McLennan Benefits
Handbook. MCMC therefore theoretically had all of the information previously submitted to
Aetna by Plaintiff and his providers for purposes of handling the external review.
62.
To confirm MCMC's receipt of his records forwarded by Aetna and to verify the
contents of the information in MCMC's possession, on June 13, 2014 Plaintiff faxed MCMC the
following request:
In order to ascertain whether additional documentation is needed from my
providers or me, and to confirm everything contained in my Aetna file is in
19
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 20 of 35
MCMC's possession, please provide an itemized list of any and all documents
and/or material MCMC has received from Aetna related to my claim, including
but not limited to, treatment and claims records, provider letters, memos,
attachments to cover letters, research, and bibliographic references. Unless and
until I know what MCMC has, I cannot know if anything is missing and/or that
additional documents are needed.
63.
Then, on July 7, 2015, Plaintiff repeated his request with another fax to MCMC:
Please consider this my final request for: ( 1) copies of any and all documents
related to this External Review (ER) that will be in the possession of the
Independent Reviewer (IR) not submitted by my providers or me, including
policy and coverage documents and the Summary Plan Description for Marsh &
McLennan Companies; and (2) references to and copies of any and all additional
material in any way accessed and reviewed by the IR as it relates to this ER.
64.
Although on August 23, 2010 the United States Department of Labor ("DOL")
issued Technical Release 2010-01, Interim Procedures for Federal External Review, in which it
required IROs to maintain all external appeal records for six years and instructed "that an IRO
must make such records available for examination by the claimant ... upon request," by letter
dated July 8, 2014 from Paul Gilleece, Vice President for Independent Peer Review, MCMC
categorically declined to provide Plaintiff with "an itemized list of any and all documents and/or
material[s] MCMC has received from Aetna related to [your] claim," falsely stating: "As there is
no legal basis under either federal or state law for your requests for documents or information,
MCMC will not comply with such requests."
65.
In addition to his previous correspondence to Aetna, Plaintiff also sent MCMC a
letter dated June 26, 2014 to supplement the information to be considered for the external appeal.
In this letter, Plaintiff described his mental health history and the many treatments he had sought
without success prior to turning to TMS. Among other things, Plaintiff pointed out that TMS did
not fall within the E/I Exclusion in the Meidl Plan given that it was approved by the FDA for the
very purposes for which he received the treatment. In addition, Plaintiff reiterated the many
20
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 21 of 35
sources that support the safety and effectiveness of TMS Therapy, including the following
statements:
•
The Johns Hopkins Department of Psychiatry: "rTMS [repetitive TMS] has been shown
to be a safe and well-tolerated procedure that can be an effective treatment for patients
with depression who have not benefitted from antidepressant medications or cannot
tolerate antidepressant medications due to side-effects. We offer rTMS at Johns Hopkins
using the only TMS device approved by the FDA for the treatment of major depression."
www .hopkinsmedicine.org/psychiatry/specialty_areas/brain-stimulation/tms/index.html.
•
Linda Carpenter, Chief of Mood Disorders and Nueromodulation at Butler Hospital:
"TMS is a game changer for the treatment of depression. And now that Medicare has
approved coverage for TMS for the patients who need it, we're hopeful that other insures
will follow. Since it was approved by FDA in 2008, ongoing research has consistently
shown the benefits of TMS for patients with depression." www.butler.org/news/TMSCovered-By-Medicare.cfm.
•
Dr. Kit Simpson, P.H., Professor of Health and Science Research at the Medical
University of South Carolina: "NeuroStar TMS Therapy is cost effective compared to
standard drug treatment for MDD [Major Depressive Disorder]. This economic
advantage of TMS over standard drug therapy is due to the substantially larger proportion
of patients who get better with TMS during acute treatments and who maintain those
results long-term." www.marketwatch.com/story/non-drug-neurostar-tms-therapy-showsfavorable-outcomes-compared-to-oral-antidepressants-in-treating-major-depressivedisorder-2014-05-06.
66.
MCMC issued its reviewer's decision on the external appeal by letter dated July
14, 2014, in which it informed Plaintiff that it was upholding Aetna' s coverage denial for TMS
therapy as "experimental/unproven," stating as follows:
Review question:
Is the requested service a Plan/Benefit exclusion as defined by the Summary
Plan Description?
The requested service is a Plan/Benefit exclusion as the treatment does not have
evidence of an overall health benefit based on the lack of long term studies of
efficacy. The treatment is not found to be as or more effective than established
alternatives such as selective serotonin uptake inhibitor (SSRI)/serotoninnorepinephrine reuptake inhibitors (SNRI) medication, ECT and psychotherapy
approaches. The treatment is not currently recognized as a standard of care but is
considered to be experimental/unproven.
21
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 22 of 35
Per the Summary Plan Description:
What's Not Covered:
Services or supplies for the diagnosis or treatment of mental illness, alcoholism
or substance abuse disorders that, in reasonable judgment of the Plan's
preauthorization review service, are any of the following:
67.
•
Not consistent with prevailing national standards of clinical practice for
the treatment ofsuch conditions;
•
Not consistent with prevailing professional research demonstrating that
the services or supplies will have a measurable and beneficial health
outcome;
•
Typically do not result in outcomes demonstrably better than other
available treatment alternatives that are less intensive or more cost
effective;
•
Not consistent with the Plan's preauthorization review service's
guidelines or best practices as modified from time to time.
In upholding Aetna's decision, MCMC failed to acknowledge, address or consider
the detailed information provided by Plaintiff or his providers, including the many referenced,
contemporaneous studies and supporting documentation, and merely rubber-stamped Aetna's
position without analysis.
68.
In support of its conclusion, MCMC cited to a series of outdated studies and did
not reference any sources published in the past three years. Strikingly, while MCMC cited to a
2001 ECT practice parameter by the American Psychiatric Association, it completely failed to
reference the far more recent inclusion of TMS as a valid treatment option for refractory
depression in the 2010 American Psychiatric Association Practice Guideline for the Treatment of
Patients With Major Depressive Disorder. MCMC's decision, as was true for Aetna, was without
support or validity, and was contrary to generally accepted standards of medical practice.
69.
Undermining any measure of transparency, MCMC's letter did not identify the
reviewer who made the decision on behalf of MCMC, but instead provided the following
22
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 23 of 35
(inadequate) background information:
I am board certified in Psychiatry with subcertification in Child & Adolescent
Psychiatry. I am an attending staff Psychiatrist at several hospitals located in the
Northeast. I am also a clinical instructor. My areas of expertise include all
psychiatric disorders, forensic psychiatry, and child & adolescent psychiatry. I am
published in the peer reviewed medical literature and I am a member of the
American Academy of Child and Adolescent Psychiatry, American
Psychoanalytic Association, and Academy of Occupational and Organizational
Psychiatrists.
70.
Nothing in this summary indicates that the reviewer had any training or
experience with TMS or related treatments for Major Depressive Disorder, or with patients - like
Plaintiff - who suffered from long-term treatment resistant depression. Notably, while the
reviewer's primary area of expertise related to child and adolescent psychiatry, TMS is not
performed on children and rarely performed on adolescents, and has been approved by the FDA
solely for adults. MCMC therefore did not use a reviewer who was qualified to make a judgment
about the safety and effectiveness of TMS therapy.
71.
MCMC's determination was as legally defective as it was clinically substandard.
Instead of reviewing Plaintiffs external appeal pursuant to the express terms of the Meidl Plan
restricting MCMC's ability to deem as "experimental" only treatments: (1) not approved by the
FDA; (2) subject to review and approval by any institutional review board for the proposed use;
or (3) subject to an ongoing clinical trial that meets the definition of a Phase 1, 2 or 3 clinical
trial set forth in the FDA regulations, MCMC cited to the above-referenced "Mental
Health/Substance Abuse" subsection of "What's Not Covered" under the Meidl Plan. MCMC
therefore failed to assess Plaintiffs appeal using the correct criteria.
72.
Moreover, by basing its denial rationale on an exclusion provision of the Meidl
Plan applicable only to mental health and substance abuse claims, MCMC ignored the Paul
Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act of 2008 ("Parity
23
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 24 of 35
Act," incorporated into ERISA at 29 U.S.C. § 1185(a)), which forbids treatment limitations
imposed only on mental health or substance abuse claims (rather than also on medical/surgical
claims).
The "Mental Health/Substance Abuse" subsection of "What's Not Covered" is a
treatment limitation imposed only on mental health and substance abuse claims under the Meidl
Plan, and is far more stringent than the general "medical necessity" requirement for claims under
the plan, (which is the only analogous requirement applicable to medical/surgical claims).
73.
In fact, the Meidl Plan defines "medically necessary" as:
•
in accordance with Generally Accepted Standards of Medical Practice;
•
clinically appropriate, in terms of type, frequency, extent, site and duration, and
considered effective for your sickness, injury, mental illness, substance use
disorder disease or its symptoms;
•
not mainly for your convenience or that of your doctor or other health care
provider; and
•
not more costly than an alternative drug, service(s) or supply that is at least as
likely to produce equivalent therapeutic or diagnostic results as to the diagnosis or
treatment of your Sickness, Injury, disease, or symptoms.
Generally Accepted Standards of Medical Practice are standards that are based on
credible scientific evidence published in peer-reviewed medical literature
generally recognized by the medical community, relying primarily on controlled
clinical trials, or, if not available, observational studies from more than one
institution that suggest a causal relationship between the service or treatment and
health outcomes.
If no credible scientific evidence is available, then standards that are based on
Physician specialty society recommendations or professional standards of care
may be considered ....
74.
For example, the mental health "What's Not Covered" prov1s1on states that
services will not be covered if they are "not consistent with prevailing professional research
demonstrating that the services or supplies will have a measurable and beneficial health
outcome." No such provision is found in the medical necessity definition applicable to all health
care services, which merely requires that the services be "clinical appropriate" and "not mainly"
for the patient's or the provider's "convenience." Similarly, while the mental health provision is
24
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 25 of 35
tied entirely to "professional research," the medical necessity provision allow "recommendations
or professional standards of care" from Physician specialty societies. Moreover, while covered
mental health services must "typically" have outcomes "demonstrably better" than less costly
services, medical/surgical care is covered unless less costly services are "as least as likely to
produce equivalent ... results."
75.
MCMC informed Plaintiff that "there is no further review available under the
appeals process," but that he "may have other remedies available under State or Federal law,
such as filing a lawsuit."
Defendants' ERISA Violations
76.
As the claims administrator responsible for interpreting and administering the
Meidl Plan, and similar Aetna plans issued nationwide, vested with responsibility for making
final benefit determinations, Aetna is an ERISA fiduciary.
77.
Similarly, when MCMC assumes the responsibility for making a final benefit
determination as part of an external review, it also assumes responsibility for administering the
Meidl Plan and similar Aetna plans, and making benefit determinations thereunder. Thus, when
acting in this capacity, MCMC is an ERISA fiduciary.
78.
As ERISA fiduciaries, Defendants were required to discharge their duties
consistent with 29 U.S.C. Section 1104, which requires (among other things) that they do so
"solely in the interest of the participants and beneficiaries" and for the "exclusive purpose" of
providing benefits to participants and their beneficiaries" and paying reasonable expenses of
administering the plan. They must do so with the "care, skill, prudence, and diligence" and in
accordance with the terms of the plans they administer. Defendants violated all of these
requirements.
25
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 26 of 35
79.
Aetna violated these duties when it prepared and promulgated the TMS Medical
Policy, because Aetna relied upon outdated evidence, ignored evidence indicating that TMS was
not experimental, and unreasonably concluded that TMS was "experimental, investigational or
unproven." Aetna then compounded that breach of duty by relying upon the TMS Medical Policy
to deny insurance claims submitted by Plaintiff and members of the Class in contravention of the
terms of their Aetna plans.
80.
In doing so, Aetna elevated its own interests above the interests of plan
participants and beneficiaries, reflecting its conflict of interest when determining whether to
cover TMS. By promulgating and applying the TMS Medical Policy, Aetna sacrificed the
interests of insureds like Plaintiff and the Class so that it could artificially decrease the number
and value of claims it was required to pay from its own assets (i.e., with respect to fully-insured
plans and self-funded plans with stop-loss provisions requiring Aetna to cover benefits above a
certain threshold) and the assets of its employer-sponsor customers (i.e., with respect to other
self-funded plans); moreover, by prioritizing the assets of its employer-sponsor customers, Aetna
also advanced its own interests in retaining and expanding its business with such customers.
81.
MCMC violated these duties when it similarly concluded that TMS Therapy was
experimental based on outdated evidence and because it ignored evidence indicating that TMS
was not experimental as defined by the terms of the Meidl Plans.
82.
MCMC has a self-serving motive to uphold Aetna's policies and coverage denials
made pursuant to those policies, since Aetna decides whether it will continue to hire MCMC to
review a large volume of appeals. As such, MCMC operates with a conflict of interest when it
serves as an IRO in reviewing Aetna appeals.
83.
Defendants' continued reliance on Aetna's internal policy to deny coverage for
26
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 27 of 35
TMS therapy based on its Ell Exclusion is particularly egregious given that in a number of
external appeals relating to TMS coverage, IRO's - other than MCMC - have frequently made
independent determinations that TMS does not fall within experimental and investigational
exclusions, but is generally accepted in the mental health community as safe and effective,
including with respect to Aetna. Defendants are fully aware of these holdings in support of TMS
therapy, but choose to ignore them.
CLASS ACTION ALLEGATIONS
84.
Plaintiff Christopher Meidl brings his claims on his own behalf and on behalf of a
"TMS Aetna Class," defined as:
All participants or beneficiaries in ERISA Plans underwritten or administered by
Defendant Aetna (or any of its operating divisions) who, during the relevant
limitations period were denied health insurance coverage for TMS provided for
the treatment of Major Depressive Disorder on grounds that included the assertion
that it was "experimental or investigational."
85.
The definition of "experimental or investigational services" in Aetna's health
insurance policies at all relevant times has been substantially similar to the definition in the
Meidl Plan.
86.
In addition, Plaintiff brings his claims on his own behalf and on behalf of a "TMS
MCMC Class," defined as:
All participants or beneficiaries in ERISA Plans underwritten or administered by
Defendant Aetna (or any of its operating divisions) who, during the relevant
limitations period, were denied health insurance coverage for TMS provided for
the treatment of Major Depressive Disorder following an external appeal in which
MCMC upheld a denial of coverage, on grounds that included the assertion that it
was "experimental or investigational."
87.
The E/I Exclusion contained in the Meidl Plan and relied upon by both Aetna and
MCMC in denying coverage for Plaintiff is largely identical to, and is interpreted by Defendants
27
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 28 of 35
as having the same meaning as, comparable exclusions included in the Aetna plans applicable to
all Class members.
88 .
The TMS Classes meet all requirements of F. R. Civ. P. 23(a) and 23(b). In
particular:
(a) The members of the TMS Classes are so numerous that joinder of all members is
impractical. While the precise number of members in this Classes is known only to
Defendants, Aetna is the ERISA fiduciary and has issued the policies providing
coverage under tens of thousands of employer-sponsored ERISA plans, and TMS
therapy has become so widespread that at a minimum, requests numbering in the
thousands must have been submitted to and denied by Aetna for coverage of this
therapy. Similarly, MCMC is a national IRO that has likely reviewed hundreds of
claims for TMS, if not more. The identities of the class members are readily
identifiable. Aetna maintains claims databases that record each instance in which it
denies coverage for TMS for treatment of Major Depressive Disorder and MCMC
maintains records of each of its external reviews, including those relating to requests
for coverage for TMS. TMS therapy is described with a discrete set of procedure
codes under the Current Procedural Terminology ("CPT") promulgated by the
American Medical Association, and depression is likewise described with a discrete
set of diagnostic codes under the Diagnostic and Statistical Manual of Mental
Disorders ("DSM"). Accordingly, the members of the Classes can be readily and
objectively ascertained through use of records maintained by Defendants.
(b) There exist issues of fact and law common to all members of this class, the most
obvious and important of which is whether TMS therapy is an "experimental or
28
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 29 of 35
investigational service." The facts that determine the answer to this question do not
vary among class members.
(c) Plaintiffs claims are typical of the claims of the TMS Class members because
Defendants based their denial of coverage in Plaintiff's case on a medical policy that
Aetna employs and an incomplete research database that MCMC references with
respect to all requests for coverage for TMS for treatment of Major Depressive
Disorder.
(d) Plaintiff will fairly and adequately protect the interests of the members of the Class, is
committed to the vigorous prosecution of this action, has retained counsel competent
and experienced in class action litigation and the prosecution of ERISA claims, and
has no interests antagonistic to or in conflict with those of the Classes.
(e) The prosecution of separate actions by individual members of the Classes would
create a risk of inconsistent or varying adjudications that could establish incompatible
standards of conduct for Defendant.
(f) By applying a uniform medical policy treating TMS therapy services as
"experimental, investigational or unproven," Defendants have acted and refused to act
on grounds that apply generally to the Classes.
(g) A class action is superior to other available methods for the fair and efficient
adjudication of this controversy because joinder of all members of the Classes is
impracticable. Further, because the unpaid benefits denied Class members are small
relative to the expense and burden of individual litigation, it would be impossible for
the Class members to redress individually the harm done to them.
COUNT I
29
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 30 of 35
CLAIM FOR VIOLATION OF FIDUCIARY OBLIGATIONS
BROUGHT ON BEHALF OF PLAINTIFF AND THE CLASSES
89.
Plaintiff incorporates by reference the preceding paragraphs as though such
paragraphs were fully stated herein.
90.
This count is brought pursuant to 29 U.S.C. § 1132(a)(l)(B).
91.
As the entity responsible for making mental health and substance abuse benefit
determinations under the Meidl Plan and the Aetna TMS Class members' similar plans, and
responsible for developing internal practices and policies to facilitate such determinations, Aetna
is an ERISA fiduciary.
92.
Similarly, as the entity that assumed responsibility for making the final benefit
determinations with respect to the Meidl Plan and the MCMC TMS Class members' similar
plans, while serving as an IRO, MCMC is an ERISA fiduciary.
93.
As ERISA fiduciaries, and pursuant to 29 U.S.C. Section 1104(a), Aetna and
MCMC are required to discharge their duties "solely in the interests of the participants and
beneficiaries" and for the "exclusive purpose" of providing benefits to participants and their
beneficiaries" and paying reasonable expenses of administering the plan. They must do so with
reasonable "care, skill, prudence, and diligence" and in accordance with the terms of the plans
they administer. They must conform their conduct to a fiduciary duty of loyalty and may not
make misrepresentations to their insureds.
94.
Aetna violated these duties by adopting and implementing a policy to deny
coverage for TMS based on the experimental and investigational exclusions under its plans,
when such a finding was contrary to generally accepted practices and to the terms of the plans.
Similarly, MCMC violated these duties by improperly applying the E/I Exclusion to TMS during
the course of issuing its final denial through the IRO process. In particular, both Aetna and
30
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 31 of 35
MCMC ignored current evidence, and widespread acceptance of TMS as a safe and effective
treatment for depression in improperly applying the E/I Exclusion to TMS. In doing so, Aetna
and MCMC did not act "solely in the interests of the participants and beneficiaries" for the
"exclusive purpose" of "providing benefits." They did not utilize the "care, skill, prudence, and
diligence" of a "prudent man" acting in a similar capacity. They did not act in accordance with
the terms of the Meidl Plan and other Aetna plans, all of which contain E/I Exclusions.
95.
Instead, Aetna and MCMC elevated their own interests and those of their
corporate affiliate above the interests of plan participants and beneficiaries. By adhering to an
incorrect and outdated policy with regard to TMS, Aetna artificially decreased the number and
value of covered claims thereby benefiting its corporate affiliates at the expense of insureds. By
improperly applying the E/I Exclusion to TMS, MCMC artificially decreased the number and
value of covered claims thereby benefiting its client Aetna, and by extension, itself.
96.
Plaintiff and the members of the Classes have been harmed by breaches of
fiduciary duty of Aetna and MCMC (with respect to the MCMC TMS Class) because their
claims have been subjected improperly to the Ell Exclusion, leading to denials of coverage for
TMS, when TMS is actually a Covered Service within the definition of the Aetna plans.
97.
Plaintiff and the members of the Class seek the relief identified below to remedy
this claim.
COUNT II
CLAIM FOR IMPROPER DENIAL OF BENEFITS BROUGHT
ON BEHALF OF PLAINTIFF AND THE AETNA TMS CLASS
98.
Plaintiff incorporates by reference the preceding paragraphs as though such
paragraphs were fully stated herein.
99.
This count is brought pursuant to 29 U.S.C. §1132(a)(l)(B).
31
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 32 of 35
100.
Aetna denied the insurance claims for TMS submitted by Plaintiff and other
members of the Class in violation of the terms of the Meidl Plan and the other Aetna plans that
insure members of the Class. Aetna denied these claims based on its E/I Exclusion, which does
not properly apply to TMS.
101.
Plaintiff and the members of the Class have been harmed by Aetna' s improper
benefit denials because they were deprived of insurance benefits they were owed.
102.
Plaintiff and the members of the Class seek the relief identified below to remedy
this claim.
COUNT III
CLAIM FOR INJUNCTIVE RELIEF
BROUGHT ON BEHALF OF PLAINTIFF AND THE CLASSES
103.
Plaintiff incorporates by reference the preceding paragraphs as though such
paragraphs were fully stated herein.
104.
This count is brought pursuant to 29 U.S.C. § 1132(a)(3)(A) only to the extent
that the Court finds that the injunctive relief sought to remedy Counts I and/or II are unavailable
pursuant to 29 U.S.C. § 1132(a)(l)(B). Plaintiff and the Class have been harmed, and are likely
to be harmed in the future, by the breaches of fiduciary duty of Aetna and MCMC described
above.
105.
In order to remedy these harms, Plaintiff and the Class are entitled to enjoin these
acts and practices pursuant to 29 U.S.C. § 1132(a)(3)(A).
COUNT IV
CLAIM FOR OTHER APPROPRIATE EQUITABLE RELIEF
BROUGHT ON BEHALF OF PLAINTIFF AND THE CLASSES
32
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 33 of 35
106.
Plaintiff incorporates by reference the preceding paragraphs as though such
paragraphs were fully stated herein.
107.
This count is brought pursuant to 29 U.S.C. § 1132(a)(3)(B) only to the extent
that the Court finds that the equitable relief sought to remedy Counts I and II are unavailable
pursuant to 29 U.S.C. § 1132(a)(l)(B).
108.
Plaintiff and the Class have been harmed, and are likely to be harmed in the
future, by the breaches of fiduciary duty of Aetna and MCMC described above.
109.
Additionally, by engaging in this misconduct, Aetna was unjustly enriched in two
ways: first, with regard to fully-insured plans or plans that include a stop-loss provision requiring
Aetna to pay all benefits above a certain threshold, it avoided paying benefits out of its own
funds and/or the funds of its corporate affiliates; second, with regard to other self-funded plans,
Aetna charged its corporate customers fees for serving as claims administrator while improperly
denying TMS benefits based on the inapplicable E/I Exclusion and also lowered costs for its
corporate customers, allowing Aetna to retain current customers and expand its business to new
customers.
110.
Similarly, MCMC was unjustly enriched by charging fees for serving as an IRO
and by maintaining and/or expanding its business with Aetna and by improperly denying benefits
based on the application of the inapplicable E/I Exclusion to TMS
111.
In order to remedy these harms, Plaintiff and the Class are entitled to appropriate
equitable relief, including an appropriate monetary award based on restitution, disgorgement or
surcharge, pursuant to 29 U.S.C. § 1132(a)(3)(B).
PRAYER FOR RELIEF
WHEREFORE, Plaintiff demands judgment in her favor against Defendant as follows:
33
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 34 of 35
A.
Certifying the Classes, as set forth in this Complaint, and appointing Plaintiff as
Class Representative;
B.
Declaring that Aetna violated the ERISA Plans, and awarding appropriate
benefits;
C.
Ordering Aetna to make payment, with interest, of unpaid benefits to Plaintiff and
all Aetna TMS Class members;
D.
Permanently enjoining Defendants from treating TMS therapy services as
"experimental or investigational" when provided to treat clinical depression;
E.
Declaring that Defendants violated the Meidl Plan and the similar Aetna plans of
the other members of both Classes and that Defendants violated their fiduciary duties under
ERISA, and awarding appropriate equitable relief including disgorgement and surcharges;
F.
Awarding Plaintiff disbursements and expenses of this action, including
reasonable attorneys' fees, in amounts to be determined by the Court; and
G.
Granting such other and further relief as is just and proper.
Isl Elizabeth K. Acee
Elizabeth K. Acee
Elizabeth K. Acee
Daniel P. Elliott
LeCLAIRRYAN, P.C.
545 Long Wharf Drive, Ninth Floor
New Haven, CT 06511
Tel. 203.672.3200
Fax 203.672.3201
[email protected]
[email protected]
34
Case 3:15-cv-01319 Document 1 Filed 09/03/15 Page 35 of 35
D. Brian Hufford (Pro Hae Vice Pending)
Jason S. Cowart (Pro Hae Vice Pending)
ZUCKERMAN SPAEDERLLP
1185 Avenue of the Americas
31st Floor
New York, NY 10036
212.704.9600
212.704.4256 (fax)
[email protected]
j [email protected]
Andrew Caridas (Pro Hae Vice Pending)
ZUCKERMAN SPAEDER LLP
1800 M StreetN.W.
Suite 1000
Washington. D.C. 20036
202.778.1855
202.822.8106 (fax)
[email protected]
Meiram Bendat (Pro Hae Vice Pending)
PSYCH-APPEAL, INC.
8560 West Sunset Boulevard, Suite 500
West Hollywood, CA 90069
310.598.3690 Ext: 101
888-975-1957 (fax)
[email protected]
Counsel for Plaintiff and the Putative Class
35