* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download CHAPTER VII. VII. Prescribing Psychotropic drugs
Survey
Document related concepts
Transcript
CHAPTER VII.
VII. Prescribing
Psychotropic drugs shall be prescribed only by, or under the documented delegated authority
of, a physician properly licensed in the State of Michigan. Licensed Prescribers include
physicians and midlevel Clinical Nurse Specialists, Nurse Practitioners and Certified
Physician's Assistants. Midlevel preservers will be scheduled for regular supervision meetings
with the CMHOC Medical Director, or another designated physician.
A. Rationale for Drugs Prescribed:
A psychotropic drug that may offer the most effective treatment for the basic psychiatric
disturbance exhibited by the consumer shall be selected from medications on the current
year's Michigan Medicaid Formulary. Rationale for each prescribed psychotropic drug shall
be documented in the consumer's record. The rationale for poly pharmacy will be clearly
documented as well.
MDCH PIHP/CMHSP Physician Injectable Drug Coverage
for Beneficiaries Enrolled in Medicaid and County Health
Plans
January 2011
PIHP/CMHSP physicians can only bill the Program directly for the following injectable
drugs when administered through the PIHP/CMHSP clinic to beneficiaries enrolled in
Medicaid and County Health Plans.
Procedure Code
Description
Fee
Screen
J0171
Injection, adrenalin, epinephrine, 0.1 mg
J0515
Injection, benztropine mesylate, per 1 mg
J1200
Injection, diphenhydramine HCL, up to 50 mg
$0.79
J1630
Injection, haloperidol, up to 5 mg
$5.93
J1631
Injection, haloperidol decanoate, per 50 mg
J2060
Injection, lorazepam, 2 mg
$0.71
J2358
Injection, olanzapine, long acting, 1 mg
$2.75
J2426
Injection, paliperidone palmitate extended release 1 mg
$6.50
J2680
Injection, fluphenazine decanoate, up to 25 m g
$1.70
J2794
Injection, risperidone, long acting, 0.5 mg
$5.05
J3486
Injection, ziprasidone mesylate, 10 mg
$6.48
S0166
Injection, olanzapine, short acting 2.5 mg
$7.35
$0.04
$60.55
$46.95
For injectable drugs administered through the PIHP/CMHSP clinic to beneficiaries
enrolled under fee-for-service Medicaid, refer to the Practitioner Database for covered
drugs and fee screens.
01/10/2011
Antianxiety Agents
Benzodiazepines
Alprazolam (Xanax, XR)
Chlordiazepoxide (Librium)
Clonazepam (Klonopin)
Clorazepate (Tranxene)
Diazepam (Valium)
Diazepam (Valium) intensol
Lorazepam (Ativan)
Oxazepam (Serax)
Quazepam (Doral)
Misc
Hydroxyzine (Vistaril, Atarax)
Buspirone (Buspar)
Max Daily Dose
LAB
Lithium (Eskalith, Lithobid)
10mg
SOOmg
20mg
90mg
40mg
60mg
10mg
120mg
30mg
400mg
60mg
SOOmg
250mg
300mg
300mg
300mg
200mg
40mg
20mg
80mg
300mg
62.5mg
200mg
40mg
IM Injections
Aripiprazole (Ability)
Fluphenazine decanoate (Prolixin)
Haloperidol decanoate (Haldol)
Olanzapine (Zyprexa Relprew)
Paliperidone palmitate (Invega Sustenna)
Risperidone (Risperdal Consta)
Naltrexone (Vivitrol)
400mg
450mg
600mg
100mg
120mg
375mg
225mg
A
B/P
B/P
B/P
LAB
2400mg
B*
30mg
20mg
SOOmg
900mg
40mg
100mg
24mg
250mg
80mg
400mg
12mg
20mg
12mg/50mg
64mg
10mg
750mg
16mg
SOOmg
60mg
40mg
160mg
AB*
AB*
AB*
AB*
AB*
AB*
AB*
AB*
AB*
AB*
AB*
AB*
AB*
AB*
B
AB*
AB*
AB*
AB*
AB*
AB*
30mg qd
25mg IM q2-3 wk
450mg IM q4 wks
300q2wk.405q4wk
234mg IM q 4 wks
50mg IM q 2 wks
AB*
AB*
AB*
AB*
AB*
AB*
380mg IM q 4 wks
Beta Blockers
Atenolol (tenormin)
Pindolol (Visken)
Propranolol (Inderal)
1200 mg
60mg
640mg
B/P
B/P
B/P
SNRI for ADHD
Atomoxetine (Strattera)
Guanfacine (Intuniv)
600mg
600mg
45mg
60mg
90mg
12mg
50ma
Max. Daily Dose
AntiDsvchotics
Aripiprazole (Ability)
Asenapine (Saphris)
Chlorpromazine (Thorazine)
Clozapine (Clozaril)
Fluphenazine (Prolixin)
Haloperidol (Haldol)
lloperidone (Fanapt)
Loxapine (Loxitane)
Lurasidone (Latuda)
Mesoridazine (Serentil)
Paliperidone (Invega)
Olanzapine (Zyprexa)
Olanzapine/Fluoxetine (Symbyax)
Perphenazine (Trilafon)
Pimozide (Orap)
Quetiapine (Seroquel, XR)
Risperidone (Risperdal)
Thioridazine (Mellaril)
Thiothixene (Navane)
Trifluoperazine (Stelazine)
Ziprasidone (Geodon)
Antideoressants
Tricyclic Antidepressants
Amitriptyline (Elavil)
Clomipramine (Anafranil)
Desipramine (Norpramin)
Doxepin (Sinequan)
Imipramine (Tofranil)
Nortriptyline (Pamelor)
SSRI's
Citalopram (Celexa)
Escitalopram (Lexapro)
Fluoxetine (Prozac)
Fluvoxamine (Luvox)
Paroxetine (Paxil, CR)
Sertraline (Zoloft)
Vilazodone (Viibryd)
Dopamine Reuptake Inh
Bupropion (Wellbutrin, SR)
Bupropion (Wellbutrin, XL)
5-HT/NE Reuptake Inh
Amoxapine (Asendin)
Desvenlafaxine (Pristiq)
Duloxetine (Cymbalta)
Venlafaxine (Effexor.XR)
Maprotiline (Ludiomil)
5-HT2 Receptor Antag
Nefazodone (Serzone)
Trazodone (Desyrel)
Noradrenergic Antagonist
Mirtazapine (Remeron)
MAOI Inhibitors
Isocarboxazid (Marplan)
Phenelzine (Nardil)
Selegiline (Emsam)
Tranvlcvoromine (Parnate)
Antimanic Agents
D
D
B/P
D
A= AIMS monitoring
B= Baseline Lab
B*=Baseline Lab and Monitoring
B/P=Blood Pressure
D=Special Diet
E= EKG (Routine)
Revised 6/2012
1.8mg/kg
4mg
B/P, B
B/P
Hypnotics
Diphenhydramine (Benadryl)
Estazolam (Prosom)
Eszopiclone (Lunesta)
Flurazepam (Dalmane)
Ramelton (Rozerem)
Temazepam (Restoril)
Triazolam (Halcion)
Zaloplon (Sonata)
Zolpidem (Ambien, CR)
Max. Daily Dose
300mg
2mg
J3rng
30mg
8mg
30mg
0.5mg
20mg
12.5mg
LAB
j
Mood Stabilizers/Anticonvulsants
Carbamazepine (Carbatrol)
Carbamazepine (Equetro)
Carbamazepine (Tegretol)
Gabapentin (Neurontin)
Lamotrigine (Lamictal)
Levetiracetam (Keppra)
Oxcarbazepine (Trileptal)
Phenytoin (Dilantin)
Pregabalin (Lyrica)
Tiagabine (Gabitril)
Topiramate (Topamax)
Valproic Acid (Depakote )
1 SOOmg
1600mg
1200mg
3600mg
700mg
3000mg
2400mg
SOOmg
600mg
56 mg
1600mg
60mg/kg
B*
B*
B*
250mg
2mg/kg
1.5mg/kg
2mg/kg
70mg
30mg
60mg
60mg
3mg/kg
400mg
B/P
B/P
B/P
B/P
B/P
B/P
B/P
B/P
B/P
B
B*
B*
B*
B*
Stimulants
Armodafinil (Nuvigil)
D-Amphet/Amphet (Adderall)
Dexmethylphenidate (Focalin, XR)
Dextroamphetamine (Dexedrine)
Lisdexamphetamine (Vyvanse)
Methylpheniate (Daytrana)
Methylphenidate (Metadate CD, ER)
Methylphenidate (Ritalin)
Methylphenidate (Ritalin LA, Concerta)
Modafinil (Provigil)
B/P.B
Miscellaneous
Acamprosate (Campral)
Benztropine (Cogentin)
Buprenorphone/Naloxone (Suboxone)
Clonidine (Catapres)
Disulfiram (Antabuse)
Docusate (Colace)
Donepezil (Aricept)
Guanfacine (Tenex)
Lubiprostone (Amitiza)
Memantine (Namenda)
Naltrexone (Revia)
Pramipexole (Mirapex)
Rivastigjriine (Exelon)
Ropinirole (Requip)
Trihexyphenidyl (Artane)
1 998mg
6mg
32mg
2.4mg
SOOmg
300mg
23mg
3mg
48mg
20mg
380mg
4.5mg
12mg
4mg
15mg
B/P
B/P
B/P
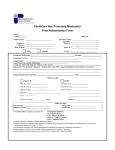
COMMUNITY MENTAL HEALTH OF OTTAWA COUNTY
Prompt for Required Monitoring of Medication Treatment
Based on Community Mental Health of Ottawa County's Mediation Committee Manual
TYPICAL ANTIPSYCHOTICS
Baseline:
•
•
•
•
Monitor:
•
CBC with differential
AIMS
Liver Enzymes
Consult with primary physician regarding baseline ECG if history of significant cardiac disorder or age *65
CBC with differential and liver enzymes annually
•
AIMS quarterly (exception for patients only taking clozaplne)
Exceptions:
•
Clozapine:: Additional weekly WBC and ANC for first six (6) months, then every two (2) weeks for next six (6) months, followed by testing
every four (4) weeks thereafter if test results remain within normal range per Fazaclo Laboratory Requirements information sheet.fsee
Clozapine Prescribing and Management)
I.
Mellarll: Routine EKG recommended
ATYPICAL ANTIPSYCHOTICS
Baseline:
•
Trlglycerldes
•
Fasting Glucose or A1C
•
AIMS Testing (not required if only antipsychotic is Clozapine)
Quarterly:
•
Triglycerides. if elevated (or refer to Primary Care Physician for monitoring)
•
Fasting Glucose or A1C if family history, symtoms or pertinent risk factors (or refer to Primary Care Physician)
•
AIMS Testing (not require if only antipsychotic Is Clozapine)
Annually:
•
Fasting glucose if no family history, symptoms or pertinent risk factors
ANTICONVULSANTS
Depakote (Valprolc Acid)
Baseline:
CBC with differential
Liver enzymes
Mo itor:
CBC with differential annually
Liver enzymes annually
Serum level within three (3) months and as clinically indicated
Tegretol (Carbamazapine)
Baseline:
•
CBC with differential
•
Liver enzymes
Monitor:
•
CBC with differential and liver enzymes annually
•
Serum level within three (3) months, and as clinically indicated
Topamax
Baseline:
•
Bicarbonate level after one (1) month of therapy (if clinically indicated)
ANTIDEPRESSANTS
Baseline:
•
Tricyclic Antidepressant: Consult with primary physician regarding baseline ECG if history of significant cardiac disorder or age *16 or *65
•
SSNRI: Blood pressure monitoring (Effexor and Cymbalta)
•
Asendin: AIMS test
Exceptions:
•
Marplan. Nardil and Parnate: Special diet recommended
LITHIUM
Baseline:
•
CBC with differential
•
Serum Creatinine, BUN. TSH. and UA annually
•
Consult with primary physician regarding baseline ECG If history of significant cardiac disorder or age +16 or * 65
Monitor:
•
Serum Creatinine. BUN. TSH, and UA annually
FOOTNOTES:
•
Lithium levels 5-14 days after a dose change, then every six (6) months 1) Drug level monitoring should be trough level
ADHD AGENTS
2) Liver enzymes= one or more enzymes
Strattera and Provigil (Modafinil): B/P
3) Baseline conditions exist when medication
•
Liver enzymes at baseline
therapy has been interrupted for more than
All Stimulants: B/P & Pulse, monitor weight for children
6 months.
Michigan Department of Community Health
Preferred Drug List
Effective 07/17/2012
Bolded Drugs do not require prior authorization, except as noted in chart at bottom of page
ANALGESICS
NARCOTICS-LONG ACTING
Kadian®
Methadone
Morphine sulfate SA tablets
Requires Prior Authorization
Avinza®
Conzip ER®
Exalgo®
Morphine sulfate ER capsules
MS Contin®
Nucynta ER®
Opana ER®
Oramorph SR®
Oxycontin®
Ryzolt ER®
NARCOTICS- SHORT AND
INTERMEDIA TE ACTING
Actiq®»
Codeine
Codeine/ APAP
Codeine/APAP/Caff./Butalbital
Codeine/APAP/Caffeine
Codeine/ASA
Codeine/ASA/Caff./Butalbital
Codeine Phosphate
Hydrocodone/APAP
Hydromorphone oral tablets
Meperidine
Morphine sulf Tabs/Soln
Oxycodone (Immed. Release)
Oxycodone/ APAP
Oxycodone/ ASA
Tramadol
Butorphanol
Capital w/Codeine®
Demerol® all forms
Dilaudid® all forms
Fentora®*
Fioricet W/Codeine®
Fiorinal W/Codeine®
Lorcet®
Lortab®
Norco®
Nucynta®
Onsolis®
Opana®
Opium
Oxydose®
Oxyfast®
OxylR®
Pentazocine and Naloxone
Percocet®
Percodan®
Roxanol®
Rybix ODT®
Roxicodone®
Stadol®, Stadol NS®
Talwin®, Talwin NX®
Tylenol #2®
Tylenol #3®
Tylenol #4®
Tylenol W/Codeine Elixir®
Tylox®
Ultracet®
Ultram®/ Ultram ER®
Vicodin®
Vopac®
Wygesic®
Xodol 5/300®
Zolvit®
Zydone®
Requires Prior Authorization
Abstral®*
1 Prior Authorization Not Required for Beneficiaries Under the Age of 12.
2 Quantity limits apply - See MPPL on website for details
3 Prior Authorization Required if Beneficiary is Over the Age of 65.
4 Prior Authorization Required for Beneficiaries Under Age of 6.
5 PA required if a benzodiazepine is found in beneficiary drug history
7 Providers should consult yearly CDC guidelines for Influenza
8 Electronic Step edit: at least 1 component of the product must be in beneficiary drug history
9 PA required if no history of oral antinausea drugs in beneficiary drug history
NARCOTICS- TRANSDERMAL
Fentanyl Patches (generic only)
Butrans®
Noxafil®
Nystatin® Tablets
Vfend®
Requires Prior Authorization
Duragesic®
ANTIVIRALS - HERPES
Acyclovir
Famciclovir
Valacyclovir
NON-STEROIDAL ANTIINFAMMATORY- COXII
INHIBITORS
Celebrex® z
ANTIBIOTICS /
ANTNNFECTIVES
ANTIFUNGALS ONYCHOMYCOSIS
Lamisil®*
Griseofulvin
Griseofulvin microsize
Griseofulvin ultramicrosize
Requires Prior Authorization
Ciclodan®
Pedipirox-4®
Penlac®
Sporanox®
ANTIFUNGALS - ORAL
Fluconazole
Nystatin Oral Susp®
Requires Prior Authorization
Diflucan®
Ketoconazole
Mycelex®
Mycostatin®
Nilstat®
Nizoral®
Requires Prior Authorization
Famvir®
Zovirax ®
Valtrex®
ANTIVIRALS - INFLUENZA7
Relenza®
Tamiflu®
ANTIVIRALS - TOPICAL
Denavir®
Zovirax® Ointment
Requires Prior Authorization
Xerese®
Zovirax® Cream
CEPHALOSPORIN 1ST GEN
Cefadroxil
Cephalexin
Requires Prior Authorization
Cephradine
Duricef®
Keflex®
Velosef®
CEPHALOSPORIN 2ND GEN
Cefuroxime axetil
Cefprozil suspension
10 Prior Authorization Required for Beneficiaries Under Age of 15.
11 Prior Authorization Required for Beneficiaries Under Age of 18.
12 Components of product must be in drug history
APAP = Acetaminophen ASA = Aspirin
CR, ER, SR, XL, XR, SA, LA = Extended Release, HCT = Hydrochlorothiazide
» Clinical PA required; refer to MPPL, Ml Provider Manual or michiqan.fhsc.com for other
restrictions
Version 07172012v1
Michigan Department of Community Health
Preferred Drug List
Effective 07/17/2012
Bolded Drugs do not require prior authorization, except as noted in chart at bottom of page
Requires Prior Authorization
Ceclor® / Ceclor CD®
Cefaclor/ Cefaclor ER
Ceftin® tabs, suspension
Cefzil®
Lorabid®
CEPHALOSPORIN 3RD GEN
Cefdinir
Cefpodoxime
Suprax® suspension
Requires Prior Authorization
Cedax®
Spectracef®
Suprax® tablets
Vantin®
HEPATITIS C
Pegasys®
Ribavirin
Peg-lntron®
Requires Prior Authorization
Copegus®
Infergen®
Intron A®
Rebetol®
Rebetron®
Roferon-A®
HEPATITIS C-PROTEASE
INHIBITORS*
Incivek®
Victrelis®
MACROLIDES
Azithromycin
Clarithromycin
Erythromycin Base
Erythromycin Estolate
Erythromycin Ethylsuccinate
Erythromycin Stearate
Erythromycin w/Sulfisoxazole
Requires Prior Authorization
Biaxin®/Biaxin XL®/Biaxin Susp.®
Clarithromycin ER
Dificid®*
Dynabac®
E.E.S.®
EryPed®
Ery-Tab®
PCE®
Zithromax® tablets
Zithromax® suspension1
Zmax®
OXALODINONES
Zyvox®
QUINOLONES
Avelox®
Ciprofloxacin
Requires Prior Authorization
Cipro XR®
Factive®
Floxin®
Levaquin®
Maxaquin®
NegGram®
Noroxin®
Tequin®
Trovan®
OPHTHALMIC
FLUOROQUINOLONES
Ciprofloxacin
Moxeza®
Ofloxacin
1 Prior Authorization Not Required for Beneficiaries Under the Age of 12.
2 Quantity limits apply - See MPPL on website for details
3 Prior Authorization Required if Beneficiary is Over the Age of 65.
4 Prior Authorization Required for Beneficiaries Under Age of 6.
5 PA required if a benzodiazepine is found in beneficiary drug history
7 Providers should consult yearly CDC guidelines for Influenza
8 Electronic Step edit: at least 1 component of the product must be in beneficiary drug history
9 PA required if no history of oral antinausea drugs in beneficiary drug history
Vigamox®
Requires Prior Authorization
Besivance®
Ciloxan®
Iquix®
Ocuflox®
Quixin®
Zymar®
Zymaxid®
OTIC QUINOLONES
Ciprodex®
Ofloxacin otic
Requires Prior Authorization
Cetraxal®
Cipro HC®
Floxin Otic®
OPHTHALMIC MACROLIDES
Azasite®
TOPICAL ANTIBIOTICS
Mupiricin ointment
Requires Prior Authorization
Bactroban®
Altabax®
ASTHMA/ALLERGY/
COPD
COPD AGENTS
Atrovent/Atrovent HFA®
Ipratropium
Spiriva®
Combivent®
Requires Prior Authorization
Daliresp®*
Arcapta®
ANTIHISTAMINES - 2ND GEN
Cetirizine
Loratadine/ Loratadine ODT
Requires Prior Authorization
Allegra®/ Allegra® Suspension
Cetirizine chewable tablets
Clarinex®
Claritin® tablets, syrup
Claritin Redi-Tab®
Fexofenadine
Xyzal®
Zyrtec® brand
NASAL ANTIHISTAMINES
Astelin®
Astepro®
Requires Prior Authorization
Patanase Nasal®
BETA ADRENERGICS- SHORT
ACTING
Maxair Autohaler®
ProAir HFA®
Proventil HFA®
Ventolin HFA®
Requires Prior Authorization
Alupent®
Xopenex HFA®
BETA ADRENERGICS - LONG
ACTING
Serevent®
Foradil®
2
10 Prior Authorization Required for Beneficiaries Under Age of 15.
11 Prior Authorization Required for Beneficiaries Under Age of 18.
12 Components of product must be in drug history
APAP = Acetaminophen ASA = Aspirin
CR, ER, SR, XL, XR, SA, LA = Extended Release, HCT = Hydrochlorothiazide
» Clinical PA required; refer to MPPL, Ml Provider Manual or michiqan.fhsc.com for other
restrictions
Version 07172012v1
Michigan Department of Community Health
Preferred Drug List
Effective 07/17/2012
Bolded Drugs do not require prior authorization, except as noted in chart at bottom of page
Requires Prior Authorization
Brovana® nebulizer soln.
Perforomist®
BETA ADRENERGICS FOR
NEBULIZERS
Albuterol sulfate
Requires Prior Authorization
Accuneb®
Duoneb®
Metaproterenol
Xopenex®
BETA ADRENERGIC /
CORTICOSTEROID INHALER
COMBINATIONS
Advair Diskus®/ Advair HFA®
Dulera®
Symbicort®
INHALED GLUCOCORTICOIDS
Alvesco®
Asmanex®
Azmacort®
Budesonide nebulizer soln.
Flovent® Diskus/ Flovent HFA®
Pulmicort®Flexihaler
QVAR®
Requires Prior Authorization
AeroBid®
Pulmicort® Respules for nebulizer
LEUKOTRIENE INHIBITORS
Singulair®
Zafirlukast
NASAL STEROIDS
Flunisolide
Fluticasone
Nasonex®
Requires Prior Authorization
Flonase®
Nasacort®
Nasacort AQ®
Nasarel®
Omnaris®
Rhinocort® / Rhinocort Aqua®
Tri-Nasal®
Veramyst®
BEHAVIORAL HEALTH
ATYPICAL ANTIPSYCHOTICS
Abilify®
Clozapine
Fanapt®
Fazaclo®
Geodon®
Invega®
Latuda®
Olanzapine
Quetiapine
Risperidone
Saphris®
Seroquel XR®
ANTIPSYCHOTICANTIDEPRESSANT COMB.
Symbyax®
ANTIDEPRESSANTS NEWER GENERATIONS
Bupropion
Requires Prior Authorization
Buproprion Hydrobromide ER
Citalopram
Accolate®
Cymbalta®
Zyflo®
1 Prior Authorization Not Required for Beneficiaries Under the Age of 12.
2 Quantity limits apply - See MPPL on website for details
3 Prior Authorization Required if Beneficiary is Over the Age of 65.
4 Prior Authorization Required for Beneficiaries Under Age of 6.
5 PA required if a benzodiazepine is found in beneficiary drug history
7 Providers should consult yearly CDC guidelines for Influenza
8 Electronic Step edit: at least 1 component of the product must be in beneficiary drug history
9 PA required if no history of oral antinausea drugs in beneficiary drug history
Emsam®
Escitalopram
Fluoxetine
Fluvoxamine
Luvox CR®
Mirtazapine
Nefazodone
Oleptro®
Paroxetine
Pexeva®
Pristiq®
Prozac Weekly®
Sertraline
Trazodone
Venlafaxine
Venlafaxine ER
Viibryd®
CARDIAC
MEDICATIONS
ACE INHIBITORS
Benazepril/ Benazepril HCT
Captopril/_Captopril HCT
Enalapril/ Enalapril HCT
Lisinopril/ Lisinopril HCT
Vasotec® / Vaseretic®
Zestril® / Zestoretic®
ALPHA ADRENERGIC AGENTS
Clonidine
Clonidine/chlorthalidone
Guanfacine
Methyldopa
Methyldopa/HCTZ
Requires Prior Authorization
Catapres®
Catapres TTS®
Nexiclon XR®
Tenex®
ANTIHYPERTENSIVE
COMBINATIONS: ACEI-CCB
Amlodipine/benazepril
Tarka®
Requires Prior Authorization
Lotrel®
Trandolapril/verapamil
ANTIHYPERTENSIVE
COMBINATIONS: ARB-CCB
Azor®
Exforge® / Exforge HCT®
Tribenzor®
Twynsta®
Requires Prior Authorization
Accupril®
Accuretic®
Aceon®
Altace®
ANGIOTENSIN RECEPTOR
Capoten®/ Capozide®
ANTAGONISTS
Fosinipril
Benicar®
Lotensin®/ Lotensin HCT®
Benicar HCT®
Mavik®
Diovan®
Moexipril / Moexipril HCT
Diovan HCT®
Monopril® / Monopril HCT®
Losartan
Prinivil®/ Prinzide®
Losartan/HCT
Quinapril /Quinapril HCT
Micardis® / Micardis HCT®
3
Univasc®/ Unirectic ®
10 Prior Authorization Required for Beneficiaries Under Age of 15.
11 Prior Authorization Required for Beneficiaries Under Age of 18.
12 Components of product must be in drug history
APAP = Acetaminophen ASA = Aspirin
CR, ER, SR, XL, XR, SA, LA = Extended Release, HCT = Hydrochlorothiazide
» Clinical PA required; refer to MPPL, Ml Provider Manual or michiqan.fhsc.com for other
restrictions
Version 07172012v1
Michigan Department of Community Health
Preferred Drug List
Effective 07/17/2012
Bolded Drugs do not require prior authorization, except as noted in chart at bottom of page
Requires Prior Authorization
Atacand® / Atacand HCT®
Avalide®
Avapro®
Cozaar®
Edarbi®
Edarbyclor®
Hyzaar®
Teveten® / Teveten HCT®
DIRECT RENIN INHIBITORS*
Requires Prior Authorization
Amturnide®
Tekamlo®
Tekturna®
Tekturna HCT®
Valturna®
BETA BLOCKERS
Acebutolol
Atenolol
Atenolol/Chlorthalidone
Betaxolol
Bisoprolol Fumarate
Bisoprolol Fumarate/HCT
Systolic®
Carvedilol
Coreg CR®
Labetalol
Metoprolol/HCT
Metoprolol Succinate
Metoprolol Tartrate
Nadolol
Pindolol
Propranolol/ Propranolol LA
Propranolol/HCT
Sotalol/ Sotalol AF
Timolol Maleate
Requires Prior Authorization
Betapace ®/ Betapace AF®
Blocadren®
Coreg®
Dutoprol®
Inderal®
Inderal LA®
Inderide®
Innopran XL®
Kerlone®
Levatol®
Lopressor®
Normodyne®
Sectral®
Tenormin®
Toprol XL®
Trandate®
Visken®
Zebeta®
CALCIUM CHANNEL
BLOCKERSDIHYDROPYRIDINE
Afeditab CR®
Amlodipine Besylate
Dynacirc CR®
Felodipine
Isradipine
Nicardipine
Nifediac CC
Nifedical XL
Nifedipine/Nifedipine SA
Nisoldipine
Requires Prior Authorization
Adalat CC®
Cardene®/ Cardene SR®
Dynacirc®
Norvasc®
Plendil®
Procardia/ Procardia XL®
Sular®
1 Prior Authorization Not Required for Beneficiaries Under the Age of 12.
2 Quantity limits apply - See MPPL on website for details
3 Prior Authorization Required if Beneficiary is Over the Age of 65.
4 Prior Authorization Required for Beneficiaries Under Age of 6.
5 PA required if a benzodiazepine is found in beneficiary drug history
7 Providers should consult yearly CDC guidelines for Influenza
8 Electronic Step edit: at least 1 component of the product must be in beneficiary drug history
9 PA required if no history of oral antinausea drugs in beneficiary drug history
CALCIUM CHANNEL
BLOCKERS - NONDIHYDROPYRIDINE
Diltiazem/ Diltiazem XR, ER
Taztia XT®
Verapamil/ Verapamil SR
Verapamil Cap 24-hr Pellet
Colestipol
Welchol®
Requires Prior Authorization
Calan®
Cardizem® LA, SR, CD
Covera-HS®
DilacorXR®
Isoptin®
Verelan®/Verelan PM®
LIPOTROPICS: STATINS
Atorvastatin
Crestor®
Lescol®
Lescol XL®
Lovastatin
Pravastatin
Simcort© 8
Simvastatin
Vytorin®8
LIPOTROPICANTIHYPERTENSIVE
COMBINATION
Caduet®
Requires Prior Authorization
Amlodipine/ atorvastatin
LIPOTROPICS- NON-STATINS:
FIBRIC ACID DERIVATIVES
Fenofibrate, micronized
Gemfibrozil
Trilipix®
Requires Prior Authorization
Antara®
Fenoglide®
Fibricor®
Lopid®
Lipofen®
Triglide®
LIPOTROPICS: NON-STATINS
Cholestyramine
Cholestyramine Light
Requires Prior Authorization
Colestid®
Questran Light®
Questran®
Rewires Prior Authorization
Advicor®
Altoprev®
Lipitor®
Livalo®
Mevacor®
Pravachol®
Zocor®
LIPOTROPICS: NIACIN DERIV.
Niacin & Niacin ER
Niacor®
Niaspan®
LIPOTROPICS: OTHER
Zetia®
Requires Prior Authorization
Lovaza® (formerly Omacor®)
4
10 Prior Authorization Required for Beneficiaries Under Age of 15.
11 Prior Authorization Required for Beneficiaries Under Age of 18.
12 Components of product must be in drug history
APAP = Acetaminophen ASA = Aspirin
CR, ER, SR, XL, XR, SA, LA = Extended Release, HCT = Hydrochlorothiazide
» Clinical PA required; refer to MPPL, Ml Provider Manual or michiqan.fhsc.com for other
restrictions
Version 07172012v1
Michigan Department of Community Health
Preferred Drug List
Effective 07/17/2012
Bolded Drugs do not require prior authorization, except as noted in chart at bottom of page
CENTRAL NERVOUS
SYSTEM DRUGS
ALZHEIMER'S DEMENTIA
Donepezil
Exelon® capsule and patch
Galantamine
Namenda®
Requires Prior Authorization
Aricept®
Cognex®
Razadyne®
Rivastigmine capsules
ANTI-ANXIETYAlprazolam
DRUGS FOR ADHD STIMULANTS*
Adderall XR®
Amphetamine Salts
Concerta®
Dexmethylphenidate
Dextroamphetamine
Dextrostat®
Focalin®
Focalin XR®
Metadata CD®
Methylin®/Methylin®ER
Methylphenidate
Methylphenidate SR
Ritalin LA®
Vyvanse®:
GENERAL
Buspirone
Chlordiazepoxide3
Clorazepate
Diazepam3
Hydroxyzine HCL
Hydroxyzine Pamoate
Lorazepam
Oxazepam
Requires Prior Authorization
Alprazolam extended release
Atarax®
Ativan®
Buspar®
Meprobamate/ Miltown®3
Niravam®
Serax®
Tranxene®
Vistaril®
Vistaril suspension®
Xanax/Xanax XR®
Requires Prior Authorization
Adderall
Amphetamine Salts, extended release
Cylert®
Daytrana®
Dexedrine®
Methylin® chewable/ soln.
Methylphenidate LA
Procentra®
Ritalin®
Ritalin SR®
DRUGS FOR ADHD NON-STIMULANTS
Kapvay®
Intuniv®
Strattera®
AGENTS FOR MULTIPLE
SCLEROSIS:
Avonex®
Betaseron®
Copaxone®
Gilenya®
1 Prior Authorization Not Required for Beneficiaries Under the Age of 12.
2 Quantity limits apply - See MPPL on website for details
3 Prior Authorization Required if Beneficiary is Over the Age of 65.
4 Prior Authorization Required for Beneficiaries Under Age of 6.
5 PA required if a benzodiazepine is found in beneficiary drug history
7 Providers should consult yearly CDC guidelines for Influenza
8 Electronic Step edit: at least 1 component of the product must be in beneficiary drug history
9 PA required if no history of oral antinausea drugs in beneficiary drug history
Rebif®
Requires Prior Authorization
Extavia®
NON-ERGOT DOPAMINE
RECEPTOR AGONISTS
Mirapex ER®
Pramipexole
Requip XL®
Ropinirole IR
Requires Prior Authorization
Mirapex®
Neupro®
Requip®
Ropinirole ER
SEDATIVE HYPNOTIC NONBARBITURATES
Estazolam
Flurazepam10
Rozerem®5
Temazepam (excluding 22.5mg)3
Temazepam 7.5mg2'3
Triazolam3
Zolpidem11
Requires Prior Authorization
Ambien® /Ambien CR®
Doral®
Edluar®
Halcion®
Lunesta®
ProSom®
Restoril®3
Silenor®
Somnote®
Sonata®2
Zolpimist®
SEROTONIN RECEPTOR AGONISTS
Maxalt® / Maxalt MLT®
Relpax®
Sumatriptan
Treximet®
Requires Prior Authorization
Amerge®
Axert®
Frova®
Imitrex®
Sumavel®
Zomig®/ Zomig ZMT®
DIABETES
AMYLIN ANALOGS
Symlin®
SECRETIN MIMETICS
Byetta®
Victoza®
INSULINS, BASAL
Lantus®
Levemir®
INSULINS. RAPID ACTING
Apidra®
Humalog®
Novolog®
INSULIN MIXES
Humalog 50/50®
Humalog 75/25®
Humulin 50/50®
Humulin 70/30®
Novolin 70/30®
Novolog 70/30®
10 Prior Authorization Required for Beneficiaries Under Age of 15.
11 Prior Authorization Required for Beneficiaries Under Age of 18.
12 Components of product must be in drug history
APAP = Acetaminophen ASA = Aspirin
CR, ER, SR, XL, XR, SA, LA = Extended Release, HCT = Hydrochlorothiazide
» Clinical PA required; refer to MPPL, Ml Provider Manual or michLqan.fhsc.cpm for other
restrictions
Version 07172012v1
Michigan Department of Community Health
Preferred Drug List
Effective 07/17/2012
Bolded Drugs do not require prior authorization, except as noted in chart at bottom of page
INSULINS. TRADITIONAL
Humulin R 500-U®
Novolin N®
Novolin R®
Requires Prior Authorization
Humulin N®
Humulin R®
ORAL HYPOGLYCEMICS ALPHA-GLUCOSIDASE INH.
Acarbose
Glyset®
Requires Prior Authorization
Precose®
ORAL HYPOGLYCEMICS BIGUANIDES
Metformin/ Metformin XR
Requires Prior Authorization
Glucophage®
Glucophage XR®
ORAL HYPOGLYCEMICS COMBINATIONS
Actoplus Met®
Actoplus Met XR®8
Duetact®
Glyburide/Metformin
Glipizide/Meformin
Kombiglyze XR®
Janumet®
Prandimet®
Requires Prior Authorization
Avandamet®
Avandaryl®
Glucovance®
Juvisync®12
Metaglip®
Requires Prior Authorization
Avandia®
ORAL HYPOGLYCEMICS DOPAMINE RECEPTOR
AGONISTS
Cy closet®
ORAL HYPOGLYCEMICS DPP4 INHIBITORS
Januvia®
Onglyza®
Tradjenta®
ORAL HYPOGLYCEMICS MEGLITINIDES
Nateglinide
Requires Prior Authorization
Prandin®
Starlix®
ORAL HYPOGLYCEMICS - 2ND
GENERATION
SULFONYLUREAS
Glimepiride
Glipizide/Glipizide ER
Glyburide
Glyburide Micronized
Requires Prior Authorization
Amaryl®
Glucotrol®
Glucotrol XL®
Glynase®
Micronase®
ORAL HYPOGLYCEMICS THIAZOLIDINEIONES
Actos®
1 Prior Authorization Not Required for Beneficiaries Under the Age of 12.
2 Quantity limits apply - See MPPL on website for details
3 Prior Authorization Required if Beneficiary is Over the Age of 65.
4 Prior Authorization Required for Beneficiaries Under Age of 6.
5 PA required if a benzodiazepine is found in beneficiary drug history
7 Providers should consult yearly CDC guidelines for Influenza
8 Electronic Step edit: at least 1 component of the product must be in beneficiary drug history
9 PA required if no history of oral antinausea drugs in beneficiary drug history
Requires Prior Authorization
Asacol HD®
NAUSEA AGENTS - ORAL
Granisetron
Azulfidine DR®
Balsalazide
Colazal®
Dipentum®
Lialda®
Ondansetron
Sancuso®9
OPHTHALMICS
Requires Prior Authorization
Anzemet®
Kytril® Brand
Zofran®/ Zofran ODT® Brand
Zuplenz®
GLAUCOMA - ALPHA-2
ADRENERGICS
Alphagan P®
Apraclonidine
Brimonidrine tartrate
SUBSTANCE P RECEPTOR
AGONIST
Emend®
Requires Prior Authorization
lopidine®
GASTROINTESTINAL
PROTON PUMP INHIBITORS*
Nexium® capsules
Pantoprazole
Prilosec OTC®
Requires Prior Authorization
Aciphex®
Dexilant® (formerly Kapidex®)
Lansoprazole
Nexium® Susp Pkts
Omeprazole1
Prevacid/ Prevacid 24HR®
Prilosec®
Protonix®
Zegerid®/ Zegerid OTC®
ULCERATIVE COLITIS - ORAL
Apriso®
Asacol®
Pentasa®
Sulfasalazine
GLAUCOMA - BETA BLOCKERS
Betaxolol
Betimol®
Carteolol HCI
Levobunolol HCI
Metipranolol
Timolol maleate
Rectuires Prior Authorization
Betagan®
Betoptic S®
Istalol ®
Ocupress®
Optipranolol®
Timoptic®
Timoptic XE®
GLAUCOMA - PROSTAGLANDIN
INHIBITORS
Latanoprost
Travatan Z®
6
10 Prior Authorization Required for Beneficiaries Under Age of 15.
11 Prior Authorization Required for Beneficiaries Under Age of 18.
12 Components of product must be in drug history
APAP = Acetaminophen ASA = Aspirin
CR, ER, SR, XL, XR, SA, LA = Extended Release, HCT = Hydrochlorothiazide
» Clinical PA required; refer to MPPL, Ml Provider Manual or michiqan.fhsc.com for other
restrictions
Version 07172012v1
Michigan Department of Community Health
Preferred Drug List
Effective 07/17/2012
Bolded Drugs do not require prior authorization, except as noted in chart at bottom of page
Requires Prior Authorization
Lumigan®
Xalatan®
GLAUCOMA - CARBONIC
ANHYDRASE INHIBITORS
Azopt®
Dorzolamide HCI
Dorzolamide/Timolol
Requires Prior Authorization
Cosopt®
Trusopt®
GLAUCOMA - COMBINATION
ALPHA-2 ADRENERGIC-BETA
BLOCKER
Combigan®
OPHTHALMIC ANTIHISTAMINES
Ketotifen fumarate (OTC Only)
Pataday®
Patanol®
Zaditor®
Requires Prior Authorization
Bepreve®
Elestat®
Emadine®
Ketotifen fumarate (RX Only)
Lastacaft®
Livostin®
Optivar®
OPHTHALMIC MAST CELL
STABILIZERS
Alocril®
Cromolyn Sodium
OPHTHALMIC NSAIDS
Diclofenac Ophth.
Flurbiprofen sodium
Ketorolac
Requires Prior Authorization
Acular®/Acular LS®
Acuvail®
Nevanac®
Voltaren®
Bromday®
MISCELLANEOUS
GROWTH HORMONES*
Genotropin®
Norditropin®
Norditropin Flexpro®
Norditropin Nordiflex®
Nutropin®
Nutropin AQ®
Requires Prior Authorization
Humatrope®
Omnitrope®
Saizen®
Serostim®
Tev-Tropin®
Zorbtive®
OSTEOPOROSIS AGENTS:
BISPHOSPHONATES
Alendronate Sodium
Requires Prior Authorization
Actonel®
Atelvia®
Boniva®
Didronel®
Fosamax®
Requires Prior Authorization
Fosamax Plus D®
Alomide®
1 Prior Authorization Not Required for Beneficiaries Under the Age of 12.
2 Quantity limits apply - See MPPL on website for details
3 Prior Authorization Required if Beneficiary is Over the Age of 65.
4 Prior Authorization Required for Beneficiaries Under Age of 6.
5 PA required if a benzodiazepine is found in beneficiary drug history
7 Providers should consult yearly CDC guidelines for Influenza
8 Electronic Step edit: at least 1 component of the product must be in beneficiary drug history
9 PA required if no history of oral antinausea drugs in beneficiary drug history
OSTEOPOROSIS AGENTS:
OTHER
Calcitonin
Requires Prior Authorization
Forteo®
Fortical®
Miacalcin®
OSTEOPOROSIS AGENTS:
SERMS
Evista®
URINARY TRACT
ANTISPASMODICS
Detrol LA®
Oxybutynin/ Oxybutynin ER
Toviaz®
Vesicare®
Requires Prior Authorization
Detrol®
Ditropan/ Ditropan XL®
Enablex®
Flavoxate HCL
Gelnique®
Oxytrol®
Sanctura®
Urispas®
TOPICAL
IMMUNOMODULA TORS »
Elidel®
Protopic®
ELECTROLYTE DEPLETERS
Calcium acetate
Fosrenol®
Renagel®
Renvela® tablets, powder
Requires Prior Authorization
Phoslo®
BPH AGENTS
Avodart®
Finasteride
Prazosin
Tamsulosin
Terazosin
Uroxatral®
Requires Prior Authorization
Alfuzosin
Flomax®
Jalyn®
Proscar®
Rapaflo®
BIOLOGIC IMMUNOMODULATORS
Enbrel®
Humira®
Cimzia®
Simponi®
Requires Prior Authorization
Kineret®
Orencia® SC
HEMATOPOIETIC AGENTS*
Aranesp®
Epogen®
Procrit®
ANTICOAGULANTS
Arixtra®
Fragmin®
Lovenox®
Pradaxa®
Xarelto®
Warfarin
10 Prior Authorization Required for Beneficiaries Under Age of 15.
11 Prior Authorization Required for Beneficiaries Under Age of 18.
12 Components of product must be in drug history
APAP = Acetaminophen ASA = Aspirin
CR, ER, SR, XL, XR, SA, LA = Extended Release, HCT = Hydrochlorothiazide
» Clinical PA required; refer to MPPL, Ml Provider Manual or michigan.fhsc.com for other
restrictions
Version 07172012v1
Michigan Department of Community Health
Preferred Drug List
Effective 07/17/2012
Bolded Drugs do not require prior authorization, except as noted in chart at bottom of page
Requires Prior Authorization
Enoxaparin
Fondaparinux
Innohep®
COMBINATION BENZOYL
PEROXIDE AND CLINDAMYCIN
Benzaclin®
Requires Prior Authorization
Acanya® gel
Duac CS®
SKELETAL MUSCLE RELAXANTS
Baclofen
Chlorzoxazone
Cyclobenzaprine
Methocarbamol
Orphenadrine citrate
Tizanidine tablets
Requires Prior Authorization
Amrix®
Dantrium®
Dantrolene sodium
Fexmid®
Lorzone®
Norflex®
Orphenadrine Compound
Parafon Forte DSC®
Robaxin®
Skelaxin®
Zanaflex® capsules, tablets
AGENTS FOR FIBROMYALGIA
Cymbalta®
Lyrica®
Savella®
Note: Not all medications
listed are covered by all
MDCH Programs. Check
individual program
coverage.
For program drug coverage
information, go to
michigan.fhsc. com
Open "Drug Coverage"and
click on "MPPL Including
Coverage Information" for
all programs.
Michigan Department of
Community Health, in
conjunction with
Magellan Medicaid
Administration, is
pleased to offer an
alternative means to
submit pharmacy prior
authorization (PA)
requests for prescription
drugs. This web-based
process is designed to
save prescribers time by
providing a real-time
pharmacy prior
authorization. This
process will supplement
1 Prior Authorization Not Required for Beneficiaries Under the Age of 12.
2 Quantity limits apply - See MPPL on website for details
3 Prior Authorization Required if Beneficiary is Over the Age of 65.
4 Prior Authorization Required for Beneficiaries Under Age of 6.
5 PA required if a benzodiazepine is found in beneficiary drug history
7 Providers should consult yearly CDC guidelines for Influenza
8 Electronic Step edit: at least 1 component of the product must be in beneficiary drug history
9 PA required if no history of oral antinausea drugs in beneficiary drug history
the more traditional
means of requesting PAs
by phone or fax, which
will still be available to
providers. In order to
use WebPA, provider
designees will need to
register to receive a
logon and password for
the WebPA system.
Detailed information on
user registration and
WebPA, including a web
based tutorial, and a
complete instruction is
available at
michiqan.fhsc.com.
For questions or
assistance with
registration, call the
Magellan Medicaid
Administration Web
Support Call Center at
(800) 241-8726.
8
10 Prior Authorization Required for Beneficiaries Under Age of 15.
11 Prior Authorization Required for Beneficiaries Under Age of 18.
12 Components of product must be in drug history
APAP = Acetaminophen ASA = Aspirin
CR, ER, SR, XL, XR, SA, LA = Extended Release, HCT = Hydrochlorothiazide
» Clinical PA required; refer to MPPL, Ml Provider Manual or rnichiqan.fhsc.corn for other
restrictions
Version 07172012v1
VII. Prescribing (cont.):
B. Dosage Range:
Dosage levels shall not ordinarily exceed those specified in the PDR and general guidelines
from current psychiatric literature. If dosage levels are prescribed in excess of the
maximum recommended daily dose, rationale shall be documented in the consumer's
clinical record and the medication consent form must reflect the actual dose prescribed.
C. Individualized Care:
1. All individuals receiving psychiatric services from Community Mental Health of
Ottawa County (CMHOC) shall be given a Psychiatric Evaluation before the onset
of any psychiatric services and/or treatment.
2. Medication regimens must be individually determined by considering the consumer's
need, age, sex, weight, physical condition, medical history, other medications and
previous medication history including history of adverse side-effects or reactions. If
indicated, a non-formulary drug may be prescribed.
3. Psychotropic drugs are medications used for the treatment or amelioration of
disorders of thought, mood or behavior.
4. Whenever a consumer is prescribed medication, at least one treatment goal will be
written addressing medication. Specific goals might include educating the consumer
about medication, eliminating target symptoms, reducing side-effects, monitoring
adherence and/or obtaining the minimum effective dosage.
5. Medications shall not be administered unless:
a. The consumer/guardian gives written informed consent, or temporary verbal
consent. In the event of verbal consent, it shall be followed up by a written
consent as soon as possible.
b. It is required by court order.
C. Individualized Care (cont):
6. Minimal duration of medications and safe termination will be determined by the
licensed Prescriber based on the consumer's specific response and accepted
medical practice.
7. No medication will be prescribed as a punishment or for staff convenience.
8. Medication will only be administered by licensed medical staff or by personnel trained
to do so by the CMHOC Training Center.
9. Any medication administered by CMH or contractual providers will be documented in
the consumer's record, including medication errors or adverse reactions.
10. Medication will not be administered in emergency situations as a means of preventing
harm to the consumer or others. There will be no standing PRN medication orders for
behavioral control. In such situations, emergency personnel will be called for
transport to the ER for evaluation.
D. Side-Effects:
1. The prescribing professional will assess the consumer's learning needs in the
safe and effective use of medication.
2. A plan will be developed based on this assessment to assure consumers are
informed of and understand the name and description of the medication, dosage,
method of administration, intended outcomes, potential side-effects, drug and food
interactions to be avoided, and proper storage and disposal.
3. The consumer will be instructed to report any occurrence of side-effects to the
prescribing professional as soon as possible.
4. A Patient Information leaflet will be offered to the consumer/parent/guardian.
This medication-specific Patient Information leaflet summarizes common adverse
side effects, purpose of medication, etc.
E. Request for Refills/Report of Medication Issues
1. Phone calls from consumers with requests for medication refills will be transferred
to the Team Nurse's office.
2. Phone calls from consumers with problems and/or issues related to their CMH
prescribed medication will also be forwarded to the office of the Team Nurse.
3. New consumers will be informed by the teams members that medication refill
requests should to be made one week prior to running out of medication.
4. Signs will be posted in the adult and child waiting rooms, offices of prescribers
and nursing offices, reminding consumers of the need to call one week in advance
for medication refill requests.
5. Refill requests and medication-related issues will be documented utilizing the
Medication Clinic Request progress note option, and forwarded to the To Do
List of the consumer's prescriber. (see Operational Guidelines for Medication
Clinic Request)
6. Transcription of the phone message, and subsequent calls to obtain additional
detailed information regarding the consumer's medication related phone message,
will be completed by either a Nurse or CMA.
7. If the recipient's assigned prescriber is not working at CMHOC on that day, the
Team Nurse will utilize her professional judgment regarding whether the phone
request should be forwarded to another prescriber for handling, or it is able to
wait until the assigned prescriber returns to CMHOC.
8. If a CMA transcribes the medication-related phone message, and the assigned
prescriber is not present, the CMA will check with the Team Nurse regarding the
professional judgment required in #7 above.
9. All CMHOC prescribers are expected to share the responsibility of refilling
medications, responding to medication-related issues and evaluating
evaluating consumers in crisis when a consumer's assigned prescriber is not available.
COMMUNITY MENTAL HEALTH OF OTTAWA COUNTY
OPERATIONAL GUIDELINE
Page I of 2
TITLE: MEDICATION CLINIC REQUESTS ISSUED BY: Dr. Bruce Walters, Medical Director
EFFECTIVE DATE: May 1, 2010
REVISED DATE: June 23, 2010
APPROVED BY: Dr. Michael Brashears, Executive Director
I.
PURPOSE: To enact a protocol identifying a consistent manner of documentation for medication
related to requests, issues or observations of an active consumer receiving psychiatric services by utilizing
the CMHOC electronic medical record system.
II.
APPLICATION:
CMHOC treatment teams serving consumers who receive psychotropic medication.
III.
DEFINITIONS:
N/A
IV.
PROCEDURE:
A.
Any CMHOC staff person with access to the CMHOC electronic health record system may utilize the
Medication Clinic Request template by performing the following steps:
STAFF RESPONSIBILITIES:
1.
Log on to AVATAR
2.
Select the chosen consumer by name or ID number.
3.
Select AVATAR PM > PROGRESS NOTES > PROGRESS NOTE
4.
Select active TEAM EPISODE, then OK
5.
Choose INDEPENDENT NOTE, then DRAFT
6.
From dropdown listing under NOTE TYPE, choose MEDICATION CLINIC REQUEST
7.
Type message into body of NOTES FIELD, including name of caller and phone number to
return call, if provided.
8.
Click arrow on top left of field to advance to 2nd page of progress note (page 2 of 2)
9.
Select MENTAL HEALTH
10.
Select prescriber's name from dropdown listing near "User to Send Co-Sign To Do item
to" if action from a CMHOC prescriber is required.
11 .
Return to Page 1 of Progress Note using arrow icon on top of page
12.
Change DRAFT to FINAL
13.
Utilize SUBMIT icon on top of form to send message to the To Do List of chosen Prescriber.
14.
Staff utilizing the Medication Clinic Request template may choose to develop a system (log,
list, reminder on Lotus Notes Calendar, etc.) to log communication sent in this manner awaiting a
response from the prescriber. NOTE: When selecting a reminder system, consider that it may need
to be shared with your supervisor and/or other coworker(s) to follow up if you are off work due to
illness or vacation.
1 5.
The current AVATAR system does not allow Prescribers to send the item back to your
To Do List to alert you when they have responded. You will receive a response via your Lotus
Notes email.
16.
Medication Clinic Request progress note entries will also be utilized to document other
medication related consumer phone or in person contact that does not require Prescriber action. This
may include pharmacy contacts, insurance prior authorization requests, questions or education.
PRESCRIBER RESPONSIBILITES:
1
Prescribers will regularly monitor their AVATAR To Do List for incoming communication that
requires their attention.
2
Prescribers will address items when time permits between appointments, during "paperwork time"
or during times when consumers fail to keep appointments.
3
All prescribers have access to check dates of future medication review appointments, past history
of "no shows", medication reviews and prescription & pharmacy information on InfoScriber to review on an
as needed basis.
4
All Medication Clinic Requests sent to prescriber To Do Lists require written documentation
indicating that the prescriber has reviewed the communication, taken some action (or chosen not to) and/or
requests that the CMHOC staff member who originated the message take an additional action.
5
By double clicking on an entry in the To Do List, prescribers will be able to review the message and
type their response. Prior to submitting the response by clicking on the Submit icon at the top of the page
Prescribers will copy and paste the body of the reply into a new email addressed and transmitted to the
Medication Request sender The date, time and prescribed name will automatically be attached the
AVATAR entry.
Operational Guideline Page 2 of 2 Medication Clinic Requests
F. Medication Monitoring:
a. Consumer's response to medication will be monitored and recorded as clinically
indicated.
b. After the desired clinical result is obtained and the consumer's condition has
stabilized, the medication shall be maintained at the minimum maintenance dose
needed, or the consumer may be titrated off the medication.
c. If the consumer has stabilized but needs long-term maintenance medication,
The prescribing professional shall document such, and specify the frequency of
face-to-face medication review appointments.
1. Required Testing:
a. Baseline studies for psychotropic drug use are related to the pharmacology of
the specific drug used.
b. Unless the rationale for delaying/omitting tests is documented in the record,
the following guidelines for monitoring of psychotherapeutic medications are
required:
TYPICAL ANTIPSYCHOTICS
Baseline:
• CBC with differential
• AIMS
• Liver Enzymes
• Consult with primary physician regarding baseline EGG if history of significant cardiac disorder or
age >65
Monitor:
• CBC with differential and liver enzymes annually
• AIMS Test quarterly. Quarterly AIMS will be done by a medical or nursing professional to
monitor involuntary movements, and will be documented in the Psychiatric Evaluation,
Medication Review and/or AVATAR CWS.
TYPICAL ANTIPSYCHOTICS (CONT.)
EXCEPTIONS:
• Clozapine: Additional weekly WBC and ANC for first six (6) months, then every two (2) weeks
for next six (6) months, followed by testing every four (4) weeks thereafter if test results remain
within normal range per laboratory requirements information sheet.(see Clozapine Prescribing
and Management)
• Mellaril: Routine EKG recommended
ATYPICAL ANTIPSYCHOTICS
Baseline:
• Triglycerides
• Fasting Glucose or A1C
• AIMS Testing (not required if only antipsychotic is Clozapine)
Quarterly:
• Triglycerides, if elevated (or refer to Primary Care Physician for monitoring)
• Fasting Glucose or A1C if family history, symptoms or pertinent risk factors
(or refer to Primary Care Physician)
• AIMS Testing
Annually:
• Fasting glucose if no family history, symptoms or pertinent risk factors
ANTICONVULSANTS
Depakote (Valproic Acid)
Baseline:
CBC with differential
Liver enzymes
Monitor:
CBC with differential annually
Liver enzymes annually
Serum level within three (3) months and as clinically indicated
Tegretol (Carbamazapine)
Baseline:
• CBC with differential
• Liver enzymes
Monitor:
• CBC with differential and liver enzymes annually
• Serum level within three (3) months, and as clinically indicated
Topamax
Baseline:
• Bicarbonate level after one (1) month of therapy (if clinically indicated)
ANTIDEPRESSANTS
Baseline:
• Tricyclic Antidepressant: Consult with primary physician regarding baseline ECG if history of
significant cardiac disorder or age <16 or >65
• SSNRI: Blood pressure monitoring (Effexor and Cymbalta)
• Asendin: AIMS Test
Exception:
• Marplan, Nardil, and Parnate: Special diet recommended
ANTIDEPRESSANT MEDICATION FOR CHILDREN AND ADOLESCENTS
Upon initiation of prescribing an anti-depressant medication to a child or adolescent the CMH:
•
physician/PA-C/NP shall follow the agency Guidelines for the Monitoring of Children and
Adolescents being Treated with Anti-Depressants (Practice Guideline 12-008).
LITHIUM
Baseline:
• CBC with differential
• Serum Creatinine, BUN, TSH, and UA
• Consult with primary physician regarding baseline ECG if history of significant cardiac disorder or
age <16 or >65
Monitor:
• Serum Creatinine, BUN, TSH, and UA annually
• Lithium levels 5-14 days after a dose change, then every six (6) months
ADHD AGENTS
Strattera and Proviqil (Modafinil)
Baseline:
• Liver Enzymes at Baseline
All Stimulants:
• Blood pressure and pulse monitoring
• Monitor weight for children
ANTICHOLINERGICS/ANTIPARKINSONIAN
•
May be used as appropriate and monitored in the medication review record..
*Footnotes:
1.
2.
3.
Drug level monitoring should be a trough level
Liver Enzymes refers to one or more enzymes (ALT, SGPT, ALP, LAP, 5'NT, LD, GGT
and/or GGTP)
Baseline conditions exist when medication therapy has been interrupted for more than
six (6) months
COMMUNITY MENTAL HEALTH OF OTTAWA COUNTY
Prompt for Required Monitoring of Medication Treatment
TYPICAL ANTIPSYCHOTICS
Baseline:
•
CBC with differential
•
AIMS
•
Liver Enzymes
•
Consult with primary physician regarding baseline ECG if history of significant cardiac disorder or age >65
Monitor:
•
CBC with differential and liver enzymes annually
•
AIMS quarterly (exception for patient on no antipsychotic except clozapine)
Exceptions:
•
Clozapine: : Additional weekly WBC and ANC for first six (6) months, then every two (2) weeks for next six (6) months,
followed by testing every four (4) weeks thereafter if test results remain within normal range per Fazaclo Laboratory
Requirements information sheet.(see Clozapine Prescribing and Management)
1. Mellaril: Routine EKG recommended
ATYPICAL ANTIPSYCHOTICS
Baseline:
•
Triglycerides
•
Fasting Glucose or A1C
•
AIMS Testing
Quarterly:
•
Triglycerides, if elevated (or refer to Primary Care Physician for monitoring)
•
Fasting Glucose or A1C if family history, symptoms or pertinent risk factors (or refer to Primary Care Physician)
•
AIMS Testing (not require if only antipsychotic is Clozapine)
Annually:
•
Fasting glucose if no family history, symptoms or pertinent risk factors
ANTICONVULSANTS
Depakote (Valproic Acid)
Baseline:
• CBC with differential
• Liver enzymes
Monitor:
• CBC with differential annually
• Liver enzymes annually
•
Serum level within three (3) months and as clinically indicated
Teqretol (Carbamazapine)
Baseline:
• CBC with differential
• Liver enzymes
Monitor:
•
CBC with differential and liver enzymes annually
•
Serum level within three (3) months, and as clinically indicated
Topamax
Baseline:
•
Bicarbonate level after one (1) month of therapy (if clinically indicated)
Prompt for Required Monitoring of Medication Treatment (cont.)
ANTIDEPRESSANTS
Baseline:
• Tricyclic Antidepressant: Consult with primary physician regarding baseline ECG if history of significant
cardiac disorder or age <16 or >65
• SSNRI: Blood pressure monitoring (Effexor and Cymbalta)
• Asendin: AIMS test
Exceptions:
• Marplan, Nardil and Parnate: Special diet recommended
LITHIUM
Baseline:
• CBC with differential
• Serum Creatinine, BUN, TSH, and UA annually
• Consult with primary physician regarding baseline ECG
if history of significant cardiac disorder or age <16 or > 65
Monitor:
• Serum Creatinine, BUN, TSH, and UA annually
•
Lithium levels 5-14 days after a dose change, then every six (6) months
ADHD AGENTS
Strattera and Provigil (Modafinil):
• Liver enzymes at baseline
All Stimulants: B/P & Pulse for all
Monitor weight for children
FOOTNOTES
• Drug level monitoring should be trough levels
• Liver enzymes = one more liver enzyme (ALT, SGPT, ALP, LAP, 5'NT, LD, GGT and/or GGTP)
• Baseline conditions exist with therapy has been interrupted for more than 6 months.
COMMUNITY MENTAL HEALTH OF OTTAWA COUNTY
OPERATIONAL GUIDELINE
TITLE: Monitoring of Children and Adolescents Being Treated with Antidepressants
REVIEW DATES:
EFFECTIVE DATE:
5/19/10
AUTHORED BY: Muskegon County CMH
SUBJECT: Monitoring Children and Adolescents being treated with Antidepressants.
SCOPE:
CMHOC Prescribers.
PURPOSE: To ensure that all children and adolescents who are prescribed antidepressants from
Agency Physicians or Physicians Assistants are monitoring for suicidal thoughts
and behavior.
PROTOCOL: The frequency and nature of the monitoring should be individualized to the
needs of the Family and the consumer. CMH staff should enlist the
parents/guardians in the responsibility of monitoring the individual at time of the
prescription. The primary care worker or program Registered nurse will contact the
family during the first month of initiation of an antidepressant to monitor progress.
If Family members become concerned about changes they should contact Ottawa
County Community Mental Health if the child:
1. Expresses new or more frequent thoughts of wanting to die, or engages
in self destructive behavior;
2. Shows signs of increased anxiety/panic, agitation, aggressiveness, or
impulsivity;
3. Experiences involuntary restlessness (akathisia), or an extreme degree
of unwarranted elation or energy accompanied by fast, driven speech
and unrealistic plans or goals.
Adverse reactions to antidepressants are more likely to occur early in the course of
treatment or in changes of the dose. It may become appropriate to adjust the
dosage, change to a different medication, or stop using the medication.
The Physician/PA should warn the parents/guardian of abruptly discontinuing
the medication due to possibly adverse withdrawal effects such as agitation or
increased depression. The Psychiatrist/PA should convey the importance of
consulting with their Provider before changing or terminating their child's
antidepressant treatment.
G. Prescription Quantity and Refills:
1. Medication quantity for all community-based programs will be based on sound
clinical judgment. Requests for medication refills for consumers who have
missed 2 consecutive psychiatric appointments will evaluated on an individual
basis by the prescriber.
2. Unless other clinical reasons are present, prescribers shall authorize enough
prescription refills to last until the date the consumers is to schedule
a follow-up medication review appointment.
3. Consumers will be issued medication refill authorizations for no greater period
than 90 days.
H. Changes in Medications.
1. If a consumer's medication is changed between Medication Review appointments,
a progress note stating the rationale, shall be written by the prescribing professional
or other staff person to correspond with that change.
2. If a medication change occurs at the time of a Medication Review appointment, the
AVATAR CWS documentation of this appointment will include the rationale for all
medication changes.
3. When a medication is initially prescribed, or when a significant change occurs, the
consumer's primary care physician and/or other service provider will be notified
(only when a release of information form is complete and up-to-date).
I. Prescriptions:
1. Written Orders
a) The prescription shall be signed only by a physician or a PA-C./N.P.
1) Prescription medication for all consumers may be up to three month's
supply.
2) Prescribers will use CMH InfoScriber only for CMH recipients.
1. Written Orders (cont.)
b) Regular prescriptions shall be documented on InfoScriber.
1) The original shall be given to the recipient or guardian,or sent via eRx
or Fax to the pharmacy or CMH program, as needed.
c) A Health Practitioner may call or fax the prescription in to a pharmacy. This
shall be documented on the prescription with the name of the pharmacy,
date and the initial's of the Health Practitioner.
d) All written prescriptions should have corresponding documentation.
e) Class II substances shall be documented on InfoScriber, printed and signed
prior to giving it to the consumer to bring to the pharmacy for filling.
2. Verbal Medication Orders
a) Verbal medication orders from physicians, NPs or PA-Cs to RN staff will
include the name of the drug, strength, dosage, and rationale for the
medication change.
b) Nursing staff will enter the order into InfoScriber, noting on clipboard feature
that this was a verbal medication order & stating rationale.
c) Only a Health Professional may make telephone orders to a pharmacy.
d) Consent for new medications initiated by verbal order shall be obtained.
e) All changes in medication regimen shall be accompanied by documentation
in InfoScriber and a progress note
J. PRN Medication:
1. When PRN orders are written, the prescribing profession shall document in the
progress note or Medication Review documentation the justification of such.
2. There shall be an order and a dose for the specific conditions in which the PRN
order is to be administered.
3. PRN orders shall limit the number of doses to be administered within a 24 hour
time period.
J. PRN Medication (cont.)
4. The total daily dosage of PRN orders shall not exceed those specified in the PDR
or general guidelines from current psychiatric literature.
5. PRN medication will not be administered in emergency situation as a means of
preventing harm to the consumer or others; or for behavioral control.
((INSERT SCREENING FOR MEDICAL COMORBIDITIES (DR. WALTERS IS SUPPOSED TO
WRITE THIS PROCOTOL)
K. Screening for Medical Comorbidities
COMMUNITY MENTAL HEALTH OF OTTAWA COUNTY
OPERATIONAL GUIDELINE
TITLE: CLOZAPINE PRESCRIBING AND MANAGEMENT
EFFECTIVE DATE:
REVIEW DATES:
8/23/10
AUTHORED BY: Bruce Walters. MD
SUBJECT: Guideline for prescribing Clozapine when medically indicated, and to do so in
accordance with the special prescribing and monitoring requirements unique to this
medication.
SCOPE:
CMHOC MI treatment teams serving Ottawa County consumers with significant
and persistent mental illness.
PURPOSE: To establish an operational guideline for the prescribing and management of
Clozapine (name brands Clozaril and Fazaclo).
1. Clozapine prescribing and management practices shall be in accordance with
the Full Prescribing Information (package insert) approved by the FDC for
publication by manufacturers of Clozapine medications. Algorithms provided
in current FDA-approved prescribing information guides are to be followed
when making clinical decisions regarding prescribing Clozapine. It is the
responsibility of the prescriber to ensure that the most recent edition of FDAapproved full prescribing information is being followed.
2. Clozapine prescribing requires the registration of prescriber, pharmacy, and
patient (consumer) in a national registry, and periodic monitoring of WBC with
ANC for as long as Clozapine treatment continues. The results of periodic lab
testing have to be reported to the pharmacy before Clozapine can be dispensed.
3. Prescribers may exercise clinical judgment in also following recommendations
and practices regarding the use of Clozapine which may be cited in reputable
psychiatric literature and/or in generally accepted prescribing practices within
the psychiatric medical community. The clinical rationale for any deviations
from recommended prescribing practices needs to be clearly documented in the
medical record.
CLOZARIL: Starting a Patient
1.
2.
3.
4.
Call the CLOZARIL National Registry (CNR) to obtain a rechallenge number and to confirm that you and your pharmacy are registered.
Obtain a baseline WBC with ANC from patient. If within normal limits, WBC > 3500/mm3, ANC > 2000/mm3, prescribe CLOZARIL tablets.
Submit WBC and ANC information to the registered pharmacy.
Please be prepared to provide your DEA # to the CNR when you are registered for the first time.
For forms, patient enrollment, or medical information call the CLOZARIL National Registry:
1-800.448-5938
Recommended CLOZARIL (clozapine) dosage titration at start of therapy'
hs (mg][ . Total [rr
am (mg)
haL(mgJ
12.5'
|
12.5-2
50
100
100
100
100
100
50
50
100
100
'Optional
200
200
200
200
Total (mg)
150
200
200
250
250
300
300
Subsequent dosage increments should be made no more than once or twice weekly, in increments not to exceed 100 mg.
CLOZARIL: Managing the Patient
Current Monitoring Frequency
Eligibility for Monthly Monitoring
Every 2 weeks (biweekly) for 6 continuous months, following 6 continuous months of weekly
monitoring prior to May 12, 2005.
Every 2 weeks or weekly. Therapy interrupted after May 12. 2005, due to moderate leukopenia
and/or granulocytopenia*. with consecutive monitoring since restart {rechallenge) of therapy.
YES. Only if all WBC counts > 3000/mm' (and ANC >1500/mm3 if reported)
NO. Patient must have 6 continuous months of weekly monitoring, followed by 6 months of continuous
monitoring every two weeks with all WBC/ANC above increased monitoring frequency values'".
Weekly therapy for <6 months
Weekly therapy for >6 continuous months, but never monitored biweekly.
NO, Only after 1 year of continuous weekly monitoring and then 6 months of continuous every two
weeks monitoring from the date of restart (rechallenge) with all WBC/ANC above increased monitoring
frequency values**".
NO, Patient must have 6 continuous months of monitoring every two weeks with all WBC/ANC above
increased monitoring frequency values".
Increased Monitoring Frequency Requirements
Patient is currently monitored monthly and experiences a WBC < 3500/mm- and/or an ANC
< 2000/mm1.
Monitoring should be done twice weekly until WBC/ANC values are >3500 and > 2000, respectively.
The patient can return to monthly blood work.
Patient is currently monitored every 2 weeks and experiences a WBC < 3500/mrrT and/or an ANC
< 2000/mmJ.
Monitoring should be done twice weekly until WBC/ANC values are >3500 and >2000, respectively.
The patient should then be monitored every two weeks for 6 continuous months before progressing
to monthly blood work.
Patient is currently monitored weekly and experiences a WBC < 3500/'mmJ and/or an ANC
< 2000/mmJ.
Monitoring should be done twice weekly until WBC/ANC values are >3500 and >2000, respectively.
The patient should then be monitored weeWy for 6 continuous months before progressing to every two
weeks, and then monthly. Wood work.
"Prior to May 12. 2005 values for WBC and ANC counts requiring interruption of therapy were WBC < 3000/mm3 and/or ANC < 1500/mrrr. After May 12, 2005 values for counts requiring increased monitoring frequency of therapy
are WBC < 3500/ mm1 and/or ANC < 2000mm1. respectively.
Following discontinuation of therapy for any reason, the patient should have WBC and ANC count monitoring once a week for a minimum of 4 weeks. If at the end of 4 weeks WBC < 3500/mnT1 and/or ANC < 2000/mm'. weekly
monitoring should continue until WBC ^3500/mm1 and ANC 2 2000/mm3.
Clo^anf (clo^apme) use it associated with a substantial risk of seuure affected 1% to 2% of patients a; lew doses (below 300 mg/day). 3% ;c 4% at nocerate closes (300 mg/day to
600 mgAJay}. and 5% at high doses (600 Tig/day to 900 nig/day). Cloianf is contra ndicated in patients with paralyse ileus. In clinical if als. Clo£ar I was associated with a 1% r- 2%
incidence of agranulocy:csis, a ooten^iallv fatal blood disorder, which, if caught early, can te reversed. Mandatory monrtonng of WBC courts and ANC's and drug dispensing as per
the requirements specif en m the package insert, provide an erf-dent means of determining develop ng agranulocytosis. Analysis of post-rrarke-ting safety databases suggests that
Clo7anl is associated with an in-reassd risk of fatal myocarditis, especially dinng. but not limited 10. tho first mjnth o: iherany. OrthostcVic t-'yporsnsion may occur in some oatio'-is.
especially curing the i^nal phases of treatmeni. and can. in raie cases (approx -nate incidence of 1/3000). be accompanied by collapse and/or cardiac, arrest. Analysis of clinical
studies reveal that elderly pafienis with deme^tw-related psychosis treated with atypical dnt psychotic drugs are at ar increased ns.< ot death comoared ic placebo Patient;, with jn
established diagnosis of c-iabetes mellrtus who are snarled on CLOZAHIL should be n-ontored regularly for worsening plucose control (e.g.. polydipsia. potyuria. potvpriagia, and weakness)
Clozaril
(clozapine)
J
'•^SSSr
Table 1. Frequency of Monitoring based on Stage of Therapy or Results from WBC Count and ANC Monitoring Tests
Situation
Initiation of therapy
6 months - 12 months of
therapy
12 months of therapy
Immature forms present
Discontinuation of Therapy
Substantial drop in WBC or
ANC
Mild Leukopenia
Mild Granulocytopenia
Moderate Leukopenia
Moderate
Granulocytopenia
Hematological Values for Monitoring
WBC > 3500/mma
ANC > 2000/mm3
Note: Do not initiate in patients with 1) history of
myeloproliferative disorder or 2) Clozaril® (clozapine) induced
agranulocytosis or granulocytopenia
All results for
WBC > 3500/mm3 and
ANC >2000/mm3
All results for
WBC > 3500/mm3 and
ANC > 2000/mm3
N/A
N/A
Single Drop or cumulative drop within 3 weeks of
WBC > 3000/mm3 or
ANC> 1500/mm3
3500/mmJ > WBC > 3000/mmJ
and/or
2000/mm3 > ANC > 1500/mm3
3000/mmJ > WBC > 2000/mmJ
and/or
1500/mm3 > ANC >1000/mm3
Severe Granulocytopenia
WBC < 2000/mmJ
and/or
ANC < 1000/mm3
Agranulocytosis
ANC < 500/mm3
Severe Leukopenia
Frequency of WBC and ANC Monitoring
Weekly for 6 months
Every 2 weeks for 6 months
Every 4 weeks ad infmitum
Repeat WBC and ANC
Weekly for at least 4 weeks from day of discontinuation or until WBC >
3500/mm3 and ANC > 2000/mm3
1. Repeat WBC and ANC
2. If repeat values are 3000/mm3 < WBC < 3500/mm3 and ANC <
2000/mm3, then monitor twice weekly
Twice-weekly until WBC > 3500/mmJ and ANC > 2000/mmJ then return to
previous monitoring frequency
1.
2.
3.
4.
5.
Interrupt therapy
Daily until WBC > 3000/mm3 and ANC >1 500/mm3
Twice-weekly until WBC > 3500/mm3 and ANC > 2000/mm3
May rechallenge when WBC > 3500/mm3 and ANC > 2000/mm3
If rechallenged, monitor weekly for 1 year before returning to the usual
monitoring schedule of every 2 weeks for 6 months and then every 4
weeks ad infmitum
1 . Discontinue treatment and do not rechallenge patient
2. Monitor until normal and for at least four weeks from day of
discontinuation as follows:
•
Daily until WBC > 3000/mm3 and ANC > 1 500/mm3
•
Twice weekly until WBC > 3500/mm3 and ANC > 2000/mm3
•
Weekly after WBC > 3500/mm3
1 . Discontinue treatment and do not rechallenge patient
2. Monitor until normal and for at least four weeks from day of
discontinuation as follows:
•
Daily until WBC > 3000/mm3 and ANC > 1 500/mm3
• Twice weekly until WBC > 3500/mm3 and ANC > 2000/mm3
• Weekly after WBC > 3500/mm3
*WBC=white blood cell count: ANC=absolute neutrophil count; CNR=Novartis CLOZARIL National Registry; G-CSF & GM-CSF=bone marrow colony-stimulating factor
M. Medications for Behavior Management
The Behavior Treatment Review Committee (BTRC) has developed the following policy:
1. Medication may be prescribed without approval of BTRC when use of medication is part
of generally accepted medical practice for the diagnosed condition. In this instance, if
the treatment team has concerns about behavior management implications of the
medication treatment, referral to the BTRC for approval or advice would be acceptable.
All other uses of psychotropic medications will be reviewed and approved by the
Behavior Treatment Review Committee.
2. The Behavior Treatment Review Committee has its own Operation and Procedure
Manual. In summary, the BTRC will review use of medications in order to determine the
clinical appropriateness of medication versus a behavioral program for controlling
behavior. The BTRC will not recommend specific medications or dosages once approval
for medication use has been granted.
Prohibited Abbreviations
"Do Not Use List"
Abbreviation
Potential Problem(s)
Preferred Term(s)
A.S., A.D., A.U., O.S., O.D.
and O.U.
Mistake for each other
Write "left ear", "right ear",
"both ears"; "left eye",
"right eye", or "both eyes"
c.c.
Mistaken for U (units) when
poorly written
U (for unit)
Mistaken as zero, four or cc
Mistaken as IV
(intravenous or 10)
Write "ml" for milliliters
Write "unit"
Write "international unit"
Mistaken for Q.O.D., and
Q.D. (Latin abbreviation for
the period after the Q can be
once daily)
Write "daily"
mistaken for an "I"
i.
Mistaken for Q.D. and the
Q.O.D. (Latin abbreviation i
. , . 7* _
,
ji
period after the Q can be
for once every other day)
_
„:£
Write "every other day"
mistaken for an ! and the
"O" can be mistaken for "I"
Trailing Zero
Never a zero by itself after a
Decimal point is missed
decimal pqintJX nig) _
Always use a zero before a
Lack of Leading Zero
Decimal point is missed
decimal point (Q.X mg)
Confused for MSO» and
Write "morphine sulfate"
MS
MgSO4
Confused for MS and
Write "magnesium sulfate"
MSO4
MgjSO4_
Write "shartness~ofbreath"
SOB
Confused with an epithet
T.I.W.
Mistaken for three times a
day or twice weekly,
resulting in overdose
Write "3 times weekly" or
"three times weekly"
0. CONTROLLED MEDICATIONS
1. Controlled Substance Education/Contract
a. When a prescription for a controlled substance is written by a CMH prescriber for a
recipient responsible for self-administration of medication, or who will soon be responsible
for self-administration of medication,, he or she will be required to sign the consent for
that medication and the Controlled Substance Contract if one has not previously been
signed.
b. The parent of a minor child who is prescribed a controlled substance by a CMH prescriber
will be required to sign the Controlled Substance Contract.
c. A health professional will explain to the recipient, guardian or parent the Controlled
Substance Education/Contract Form and "Controlled Substance
Education" Brochure, reviewing the contents with the person(s) involved.
d. A copy of the signed Controlled Substance Education/Contract will given to the consumer,
along with the brochure to take home for reference and to read more thoroughly.
e. The original of the Controlled Substance Education/Contract will be filed in the consumer's
medical record, under the Consents Tab.
1) Controlled Substance Information Guidelines, Medical Records Form 101 Ml
2) Controlled Substance Education Brochure
CONTROLLED SUBSTANCE INFORMATION GUIDELINES
JL|
Z
Q
O
^5
£fe
^
^f
tO
••
^j
»^™
This information is being provided to make sure that you have a safe and effective treatment plan. CMHOC wants
you to be aware that there are possible adverse reactions and conditions that may develop with the use of
controlled substances. Controlled substance is a drug or chemical substance whose possession and use are
controlled by law. Examples include: Ativan & Ritalin.
Psychological dependence or addiction can occur with use, but the risk is low when the medications are used
properly. You will be given a list of some of the possible complications of treatment with controlled substances and
additional information can be found on the "Controlled Substance Education Sheet" and the information sheet that
comes with the prescription.
It is important to take the medication exactly as prescribed and exactly as instructed. If you run out of the
medication too soon or stop it suddenly, you might experience withdrawal symptoms that could be uncomfortable
or dangerous. If you have questions or concerns about the amount you are taking, or when you take them, please
contact the Medication Clinic to speak to a nurse. Do not change the dose amounts or change the time schedule of
taking the medications without first calling the medication clinic.
(392-1873 in Holland and 842-5350 in Grand Haven)
lf you become pregnant (if applicable), the baby may become addicted to the medication or experience other
unknown risks. Please let us know if you become pregnant or think you may be pregnant.
It is dangerous to get controlled substance medications from more than one doctor. Please tell us if other doctors
are prescribing these medications for you and we will coordinate our recommendations with them.
Your confidentiality is important and we will ask you to sign a release of information giving us permission to consult
with your health care providers and with your pharmacy about the use of these medications.
Please select one pharmacy to obtain all of your medications.
<
Pharmacy Name:
Pharmacy Address:
Pharmacy Telephone Number:
Prescriptions can only be filled during regular CHMOC working hours: Monday through Friday, 8:00 am to 5:00
pm. No controlled substances will be refilled after hours, on weekends or holidays.
Keep track of how much medication you have left and please allow 7 days for a prescription to be filled. It is very
important that you allow adequate time to refill your medication. We can only accept telephone requests for
controlled substance medication refills from you (or parent/guardian, if applicable).
If you are too disabled or sick to come in, the decision to allow another person to pick up your prescription will be
determined at CMHOC's discretion. Minors cannot pick up prescriptions and we can only give prescriptions to
people for whom we have a signed valid release of information form.
Please let us know immediately about any medication-related side effects. If any significant side effects occur
during regular working hours, call the medication clinic. If they occur after hours or on weekends or holidays,
please call the Helpline at 1-866-512-HELP and ask to speak to the on-call worker. If you need immediate medical
attention, please go to the nearest emergency room.
CMHOC cannot continue to prescribe controlled substances if they are not adequately monitored. You will be
scheduled for medication reviews as often as your doctor feels is necessary and it is important that you keep these
appointments. If you cannot make your scheduled appointment, please notify us a minimum of 24 hours in
advance.
For your safety, it is a federal offense to alter a prescription in any way and to transfer a controlled substance to
another person. We are required by law to report these incidents and legal action could result. Protect yourself
and others; don't let other people use your medication.
CMHOC - Controlled Substance Information Guidelines - 03/5 - 101 Ml - 10/24/07 Case Number:
CONTROLLED SUBSTANCE INFORMATION GUIDELINES
IBB
mm
D
O
I *
<
^(
|_
CMHOC cannot renew prescriptions before they expire and cannot replace prescriptions for you. This includes lost
or destroyed prescriptions or lost, damaged, or stolen medications.
If your CMHOC health care provider has concerns about your well-being, they may ask you to submit to a random
urine or blood sample for drug screens. The results of these tests will be fully explained to you, as well as any
recommendations for possible changes in your treatment.
For stimulant medications only:
•
•
•
Prescriptions can only be handwritten; we cannot call in or fax stimulant prescriptions
Refills cannot be listed on a prescription
Prescriptions must be picked up and cannot be mailed
Your signature below indicates that this information has been fully explained to you and that any questions or
concerns have been fully addressed.
Consumer's Name
DOB_
Consumer's/Guardian Signature
IL
O
X
<
CMHOC - Controlled Substance Information Guidelines - 03/5 - 101 Ml - 10/24/07 Case Number.
Conditions That May
Develop with Controlled
Substance Use
Consumer Education
Physical Dependence - after
stopping the medication you can
have withdrawal symptoms.
These may include:
ID nausea/vomiting
ID sweating
ID shaking
ID general bad feeling or
anxiety
The activities and programs of this agency are brought to you
by the members of the Ottawa County Board of
Commissioners. The Michigan Department of Community
Health provides financial support to this agency.
CONTROLLED
SUBSTANCE USE
ID runny nose
ID diarrhea and/or abdominal
cramping
Community Mental Health of Ottawa County has been
accredited by CARF for twelve of its programs.
ID soreness or aches
Psychological Dependence or
addiction - the risk is low when
you follow directions on how to
take the medication. After
stopping the medication, you
may go through withdrawal this is related to physical
dependence. If your body feels
like, or you think you have
become dependent on
medication, then you may act
like you are addicted to drugs.
Administrative Offices
12265 James Street
Holland, Ml 49424
Customer Service Phone:
(616)494-5545
Toll-free 1-866-710-SERV (7378)
Consumer Education
Rev. 08-2008
COMMUNITY
M E N T A L
H E A L T H
O T T A W A
C O U N T Y
/Consumer Education on
1 Controlled Substance Use
You have been prescribed a
controlled substance by your
health care provider. This
medication will be used to treat
your mental health concerns.
For this treatment to work, you
should follow all of these
important instructions:
Z) Please keep all of your
appointments.
Z> Be careful with your
prescriptions and
medications.
We will not replace
lost, destroyed,
damaged, or stolen
prescriptions or
medication.
ID Keep track of how much
medication you have
left and call for refills
during office hours
only.
Possible Adverse
Reactions (Side Effects)
There are possible adverse reactions
and conditions that may develop with the
use of controlled substances. We have
listed a few of these for your information.
Please refer to your medication teaching
sheet for a more complete list and let us
know if any of the following occur:
In the event of overdose, call the
Regional Poison Control Center:
1-800-222-1222
Possible Side Effects
Z> Allergy
Z> Overdose (can cause problems with
breathing and/or death)
Z> Constipation
Z> Itching
Z> Difficulty with urination
Z> Nausea or vomiting
Z) Change in mental status or
thinking ability
ID Increased sleepiness
Z) Problems with balance or feeling
clumsy (use caution when
operating a motor vehicle or
dangerous equipment)
Z) Problems having sex
Z) Other less common side effects
are possible
Z> Children born to mothers on
controlled substances
(narcotics) are usually
physically dependent at
birth
Z) Suddenly stopping the use of
medication may cause
seizures
For Medication Refills or to
cancel or reschedule an
appointment:
Holland
(616) 392-1873
Grand Haven .... (616) 842-5350
Hudsonville
(616) 669-6160
COMMUNITY MENTAL HEALTH OF OTTAWA COUNTY
OPERATIONAL GUIDELINE
TITLE: ADHD Protocol
EFFECTIVE DATE:
5/19/10
REVIEW DATES:
AUTHORED BY: Muskegon County CMH
SUBJECT: ADHD Protocol
SCOPE:
This guideline applies to all CMH employees and contract providers.
PURPOSE: To enable the Agency to provide consistent and effective treatment of individuals
diagnosed with ADHD.
PROTOCOL:
Adult ADHD:
1. Assessment
a. Anyone can initiate a request for an assessment of adult ADHD by contacting
CMHS staff. This may include the individual receiving services, family,
friends, medical, or mental health care staff (case manager, therapist,
psychologist, nurse, physician, physician assistant, etc.).
b. The following data will be gathered in making diagnosis of ADHD in adults:
1. Childhood/school records will be obtained by the primary worker
prior to treatment, if possible.
2. An Adult Rating Scale will be completed by the parent(s) and/or
spouse, when possible, and obtained by the primary worker prior to
treatment.
3. The Brown Adult ADD Scales/Conner's Adult ADHD Rating Scale
procured from a supports coordinator will be completed by the
individual and obtained by the primary worker prior to psychiatric
evaluation.
4. A developmental history and assessment of comorbid conditions will
be obtained by the Psychiatrist/Physician's Assistance/Nurse
Practitioner during a psychiatric evaluation. A diagnosis of ADHD
in an adult will me be made after consideration of the above
information.
5. For borderline ADHD cases, the Psychiatrist/Physician's
Assistant/Nurse Practitioner may request additional testing using
such instruments as the CPT, WAIS-IV, or achievement measures.
6. When an adult individual comes to Ottawa County Community
Mental Health with an existing diagnosis of ADHD, the
Psychiatrist/Physician's Assistant/Nurse Practitioner will verify the
diagnosis and request supportive documentation data when
indicated.
2. Treatment
a. Pharmacological Intervention
The decision to medication should be based on persistent target symptoms
sufficiently severe to cause functional impairment.
1. Medications used to treat ADHD include methylphenidate
preparations, amphetamines, alpha 2 Adrenergic agonists, Strattera,
Modafanil, NDRIs/Antidepressants
2. Any adult with a history of substance abuse will be prescribed nonstimulant medications as first choice and/or long-acting stimulant
medication as a second choice. If there is a less than an adequate
response or no response to this documented intervention, then shortacting stimulant Medications may be prescribed provided the
individual is also involved in substance abuse treatment.
3. Whenever possible, for the sake of differential diagnosis,
pharmacological treatment of comorbid DSM-IV conditions should be
initiated and evaluated prior to the initiation of stimulant medication
for ADHD symptoms.
4. The prescribing Psychiatrist/Physician's Assistant/Nurse Practitioner
shall be responsible for assuring there are no contraindications for
stimulant medication; and if needed, request the individual to obtain
necessary lab work or a physical exam, or consultation with specialists
(e.g. cardiologist).
b. Psychosocial, Behavioral, and Environmental Intervention
The individual receiving services should be provided information regarding
the availability of adjunct treatment modalities for ADHD, including:
1.
2.
3.
4.
Education using a biopsychosocial model.
Accommodations to help foster attention skills.
Behavioral supports.
Individual counseling/Community Support Group (CHADD) if
available.
3. Follow-up
Periodically, the Brown Adult ADD Scales/Conners Adult ADHD Rating Scale
should be administered by the primary worker and reported to the prescriber. For
those individuals with a history of substance abuse, a lab screen sensitive to the
medication being prescribed for ADHD as well as illicit substances may be
ordered prior to the appointment date for issuing a subsequent prescription for the
prescribed ADHD medication.
Child ADHD
1. Assessment
a. Anyone can initiate a request for an assessment of child ADHD by contact CMH
staff. This may include the individual receiving services, family, friends, medical,
or mental health care staff (case manager, therapist, psychologist, nurse,
physician, physician assistant, etc.).
b. The following data will be gathered in making a diagnosis of ADHD in children:
ADHD Protocol
Page 2 of4
1. Childhood/school records will be obtained by the primary worker prior
to treatment.
2. A Parent and Teacher Rating Scale will be completed, (Achenback or
Conners), and obtained by the primary worker prior to psychiatric
evaluation.
3. A developmental history, physical exam, and assessment of comorbid
conditions will be obtained by the Psychiatrist/Physician's
Assistant/Nurse Practitioner during a psychiatric evaluation. A
diagnosis of ADHD in a child will be made after consideration of the
above information.
4. For borderline ADHD cases, the Psychiatrist/Physician's
Assistant/Nurse Practitioner may request additional testing using such
instruments as the CPT, WISC-IV, or achievement measures.
5. When a child individual comes to CMH with an existing diagnosis of
ADHD, the Psychiatrist/Physician's Assistant/Nurse Practitioner will
verify the diagnosis and request supporting documentation data when
indicated.
2. Treatment
a. Pharmacological Intervention
The decision to medicate should be based on persistent target symptoms
sufficiently severe to cause functional impairment.
1. Medications used to treat ADHD include methylphenidate preparations,
amphetamines, alpha 2 adrenergic agonists, Strattera, Modafanil, and
NDRIs/Antidepressants.
2. Any child with a history of substance abuse will be prescribed non-stimulant
medications as first choice and/or long-acting stimulant medication as a
second choice. If there is a less than adequate reason or no response to this
documented intervention, then short-acting stimulant medication may be
prescribed provided the individual is also involved in substance abuse
treatment.
3. Whenever possible, for the sake of differential diagnosis, pharmacological
treatment of comorbid DSM-IV conditions should be initiated and evaluated
prior to the initiation of stimulant medication for ADHD symptoms.
4. The prescribing Psychiatrist/Physician's Assistant/Nurse Practitioner shall be
responsible for assuring there are no contraindications for stimulant
medication; and, if needed, request the individual to obtain necessary lab work
or a physical exam or consultation with specialists (e.g. cardiologist).
b. Psychosocial, Behavioral, and Environmental Intervention
The parent and/or individual receiving services should be provided information
regarding the availability of adjunct treatment modalities for ADHD including:
1. Education using a biopsychosocial model.
2. Accommodations to help foster attention skills.
ADHD Protocol
Page 3 of4
3. Behavioral supports.
4. Individual counseling/Community Support Group (CHADD) if available.
3. Follow-up
The Conners Parent and Child Rating Scales should be administered by the primary
worker and reported to the prescriber. For those individuals with a history of substance
abuse, a lab screen sensitive to the medication being prescribed for ADHD as well as
illicit substances may be ordered prior to the appointment date for issuing a subsequent
prescription for the prescribed ADHD medication.
REFERENCES
American Academy of Child and Adolescent Psychiatry: Practice parameters for the use of
stimulant medication in the treatment of children, adolescents, and adults with Attention Deficit
Hyperactivity Disorder. J. Am Academy of Child and Adolescent Psychiatry 2002; 41
(2suppl): 265-495
Children and Adults with Attention Deficit Hyperactivity Disorder (CHADD)
ADHD Protocol
Page 4 of4
COMMUNITY MENTAL HEALTH OF OTTAWA COUNTY
OPERATIONAL GUIDELINE
Pagel of 3
TITLE: MEDICATION PRACTICE GUIDELINES AND CONTROLLED MEDICATION PRESCRIBING
EXCEPTIONS
EFFECTIVE DATE: 12/01/2010
REVIEW DATES:
AUTHORED BY: Denise Wiswell, Ph.D, Bruce Walters, M.D., Barb Sychowski, BSN
SUBJECT:
SCOPE:
PURPOSE:
MEDICATION PRACTICE GUIDELINES AND CONTROLLED MEDICATION
PRESCRIBING EXCEPTIONS
Psychiatrists, Nurse Practitioners and Physician Assistants employed or contracted
by Community Mental Health of County (CMHOC).
To provide a consistent prescribing philosophy and procedure for CMHOC
consumers who require controlled medications.
To decrease opportunities for consumers with substance use disorders to obtain
controlled medications.
To minimize unintended consumer addiction to controlled medications.
To support safe, effective and optimum guidelines for individuals receiving
psychiatric services from CMHOC who have or have a history of substance abuse.
DEFINITION:
Any medication containing a chemical classified by the Department of Justice,
Drug Enforcement Agency (DEA), Office of Diversion Control to be a Schedule
I, II, III, IV or V Controlled Substance.
MEDICATION PRACTICE GUIDELINES:
1. Prescribers will prescribe a reasonable trial of one or more non-addictive medications before
any controlled substance (addictive medication) is prescribed (regardless of patient's history
elsewhere).
2. If controlled substances are prescribed they will be time limited as indicated in the medication
dosage and duration table. Consumers who are tried on several medications will still be
subject to the overall time limits.
3. Consumers using controlled substances will be encouraged to actively participate in a holistic
recovery program which may include individual, group or other services as recommended by
their treatment team.
4. Controlled substances will not be replaced if lost or stolen.
5. Controlled substances will not be refilled early.
6. Controlled substances may or may not be prescribed to individuals receiving controlled
substances from other prescribers. This will be determined by the CMH prescriber in
consultation with the medical and/or treatment team and the other prescriber if indicated.
7. Medications with opposing effects or those with potential additive effects may not be
prescribed at the same time (i.e. sleep medication or anti-anxiety medication for someone
taking a stimulant; or anti-anxiety medication and pain medications or others with tranquilizing
effects).
8. Verification of a history of ADHD or ADD may be required before stimulants are prescribed.
This may include getting releases of information from school records or from other reliable
sources. ADHD treatment protocol will be followed (ADHD is treated after the consumer is
treated for substance abuse, mood disorder, or an anxiety disorder).
9. Functional need for stimulants should be detailed by the prescriber or the treatment team
before this type of medication is prescribed, (e.g., consumer is working and work supervisor
verifies they have difficulty staying on task; consumer has a verified school history of ADHD
and now wishes to take classes as an adult).
10. Periodic drug screens may be requested if a consumer is being prescribed a controlled
substance.
11. Dosages of controlled substances will not be increased unless it is part of the existing
(titration) plan without being seen by the prescriber.
12. The Controlled Substance Contract is required for consumers on a controlled substance.
13. A release of information to the consumer's PCP is required before any controlled substance is
prescribed. Consumers must have a PCP (within 3 months) if CMHOC is to prescribe
medications.
14. Prescribers will seek consultation from the medical team prior to prescribing medications in a
manner that departs from the above stated guidelines.
15. Prescribers will notify the treatment team if prescribing in a manner other than consistent with
the guidelines.
16. Treatment team members will notify prescribers if they receive information that might
negatively affect a consumer's health or treatment (e.g., consumer reports street drug use, has
new medications from another prescriber, is refusing other recommended treatment options,
etc).
EXCEPTION PROTOCOL:
The Prescriber requesting an exception to CMHOC Practice Guidelines for
Controlled Medication will:
1. Complete a Request for Exception to Practice Guidelines for Controlled
Medications form. (Attachment)
2. Discuss issue at Team Meeting, obtaining feedback from other team
members.
3. Team Supervisor will record a summary of team feedback on form.
4. The prescriber requesting 'exception' will e-mail a request to the Medical Director to place a
review of exception on the agenda of the next Medical Staff Meeting.
5. Prescriber will bring the exception request form to the Medical Staff Meeting and present case
to peers.
6. Following presentation at the Medical Staff Meeting, all Prescribers present, and Registered
Nurse assigned to the consumer will record their suggestions, comments and approval or
disproval of continuation of this controlled medication for the individual.
Controlled Substance Guidelines
7. Prescriber who requested exception will follow the recommended group consensus. In
instances when a clear group recommendation is not reached, Medical Director will make the
final determination.
8. Medical Director will track review date if applicable, and be responsible for including review on
future agenda of the Medical Staff Meeting.
9. Support staff will scan completed signed Exception to Practice Guidelines For
Controlled Medications form in consumers EMR.
Controlled Substance Guidelines
Controlled Substance Practice Guideline
List of Meds Affected and Dosages
Benzodiazepine anxiolytics
Generic name
Class Brand name
Alprazolam
IV
Xanax
IV
Alprazolam XR
Xanax XR
IV
Librium
Chlordiazepoxide
IV
Chlorazepate
Tranxene
IV
Clonazepam
Klonopin
Diazepam
IV
Valium
Lorazepam
IV
Ativan
Usual maximum
1-10 mg/day
1-10 mg/day
300 mg/day
60 mg/day
20 mg/day
40 mg/day
8 mg/day
Review after
6 months
6 months
6 months
6 months
6 months
6 months
6 months
Typical dosing
5-20 mg BID
10 mg/day
10 mg/day
10-70 mg/day
5-20 mg BID
10-20mgAM
20 mg/day
20 mg/day
18-54 mg/day
30 mg/9hr
Usual maximum
40-60 mg/day
20 mg/day
20 mg day
70 mg/day
60 mg/day
60 mg/day
60 mg/day
60 mg/day
72 mg/day NTE 2 mg/kg
30 mg/9hr
Review after
2 years, then indefinite
2 years, then indefinite
2 years, then indefinite
2 years, then indefinite
2 years, then indefinite
2 years, then indefinite
2 years, then indefinite
2 years, then indefinite
2 years, then indefinite
Wakefulness medications
Generic name
Class Brand name
Armodafinil
Nuvigil
IV
IV
Provigil
Modafinil
Typical dosing
150-250 mg/am
100-200 mg/day
Usual maximum
250 mg/am
400 mg/day
Review after
2 years, then indefinite
2 years, then indefinite
Anticonvulsants
Generic name
Pregabalin
Typical dosing
150mgBID/TID
Usual maximum
600 mg/day
None (not for psych use)
Typical dosing
3-6 mg/day
3-6 mg/day
10-25mgTID/QID
10-25 nig TID/QID
l-2mgBID/QID
2-10mgBID/QID
2-6 mg/day
Psychos tim u la nts
Generic name
Amphetamine combo
Dexmethylphenidate
Dexmethylphenidate XR
Lisdexamfetamine
Methylphenidate
Methylphenidate LA
Methylphenidate SR
Methylphenidate ER
Methylphenidate CR
Methylphenidate patch
Class
II
II
II
II
II
II
II
II
II
II
Class
V
Brand name
Adderall
Focalin
Focalin XR
Vyvanse
Ritalin, Methylin
Ritalin LA
Ritalin SR
Metadate CD/ER
Concerta
Daytrana
Brand name
Lyrica
Maximum duration
Hypnotics
Generic name
Chloral hydrate
Eszopiclone
Flurazepam
Temazepam
Triazolam
Zaleplon
Zolpidem
Zolpidem CR
Class
IV
IV
IV
IV
IV
IV
IV
IV
Brand name
Noctec
Lunesta
Dalmane
Restoril
Halcion
Sonata
Ambien
Ambien CR
Typical dosing
500 mg HS
2mgHS
7.5-30 mg/HS
7.5-30 mg/HS
0.25 mg/HS
5-20 mg/HS
5-10 mg/HS
12.5 mg/HS
Usual maximum
1 gmHS
3mgHS
30 mg/HS
30 mg HS
0.25 mg/HS
20 mg/HS
10 mg/HS
12.5 mg/HS
Maximum duration41
3 months
3 months
3 months
3 months
3 months
3 months
3 months
3 months
[*Does not include occasional use in DD population if only used prior to medical or dental procedures]
Opioid dependence therapy
Generic name
Class
Buprenorphone/Naloxone III
Brand name
Suboxone
Typical dosing
<12mg/day
Usual maximum
16mg/day
Maximum duration111
6 months
REQUEST FOR EXCEPTION TO PRACTICE GUIDELINES FOR
CONTROLLED MEDICATION
z
Requested by:
u
Consumer Name:
Date:
D
O
I
<
Applicable CMHOC Practice Guidelines:
O
Ik
O
D
Prescriber will prescribe a reasonable trial of one or more non-addictive medications before
any controlled substance is prescribed regardless of patient's history elsewhere.
D
If controlled substances are prescribed; they will be time-limited, as indicated in the
medication dosage and duration table. Consumers who are tried on several medications will
still be subject to the overall time limits.
Consumers using controlled substances must be actively engaged in treatment; including
groups, individual or other services (including engagement, if pre-contemplative) as
recommended by their treatment team.
D
Controlled substances will not be replaced if lost of stolen, nor refilled early.
D
Medications with opposing effect, or those with potential additive effects, many not be
prescribed at the same time (i.e. sleep medications or anti-anxiety medication for someone
taking a stimulant; or anti-anxiety medication and pain medication, or others with
tranquilizing effects).
n
Consumers must have a Primary Care Physician within 3 months of initiating medication
services, if CMHOC prescribes medication.
Medication information:
z
3
2
5
O
O
Name and dosage of medication for which exception is requested:
Date started:
(Circle: actual/estimated)
Started by:
at
Continued by requesting prescriber since:
Relevant diagnoses:
CMHOC - Exception for Controlled Medication - 03/5 -101 - Ml- 07/16/11
Case Number:
REQUEST FOR EXCEPTION TO PRACTICE GUIDELINES FOR
CONTROLLED MEDICATION
Check all that apply to this individual:
3
O
u
O Has a history of substance abuse
O Has used illegal substances within the past year
O Has requested early refills of controlled medications within the past year
O Has reported "lost" or "stolen" controlled meds within the past year?
H] Has history or known attempt to seek controlled medication from different prescriber while receiving
them from CMHOC.
CD Is currently receiving controlled medications from another prescriber.
I
Other options tried:
HU Alternate medications
0 Alternate individual treatment (i.e. individual therapies)
1 I Alternate group supports (i.e. Dual Diagnosis Group, AA, NA, etc)
O
U.
Please comment on the above, including approximate dates, span of treatment and
response. Include attempts to wean or discontinue above medication.
O
X
H
In the space below, please give detailed rationale for continuing this prescription as
written:
Treatment team comments/recommendations summary (to be completed by Team
Supervisor).
ill
2
Following presentation of case at Medical Staff Meeting, CMHOC prescribing staff will
record their comments, suggestions and recommendations with date and signature
below.
MEDICAL STAFF RESPONSE
Signature:,
Date:
D Approve
n Disapprove
O
Comments:
O
CMHOC - Exception for Controlled Medication - 03/5 -101 - Ml- 07/16/11
Case Number:
REQUEST FOR EXCEPTION TO PRACTICE GUIDELINES FOR
CONTROLLED MEDICATION
\:
2
"•
D Approve
] Disapprove
**
Comments:
U
^
Signature:
Date:
^f
D Approve
n Disapprove
^m
Comments:
O
IL
W
Signature:
Date:
^m
D Approve
D Disapprove
••
Comments:
u
X
I
Signature:
^"
H
Date:
Team Nurse
n Approve
n Disapprove
Comments:
S
Lm
^^
Signature:
Date:
Medical Director
D Approve
n Disapprove
Comments:
O
u
CMHOC - Exception for Controlled Medication - 03/5 -101 - Ml- 07/16/11
Case Number:
REQUEST FOR EXCEPTION TO PRACTICE GUIDELINES FOR
CONTROLLED MEDICATION
>
I"
Z
D
SUMMARY OF CONSENSUS AGREEMENT (completed by Medical Director)
O
O
I
RE-EVALUATE CONSUMER'S USE OF THIS MEDICATION ON:
IL
O
K
<
Z
O
O
CMHOC - Exception for Controlled Medication - 03/5 -101 - Ml- 07/16/11
Case Number:
6. Letter to Consumers Regarding Controlled Medications
a. The letter below is printed on CMHOC letterhead paper and given to
consumers eligible for psychiatric services at CMHOC by Access Clinican
completing assessment interview.
b. The information provided in the letter will also be discussed by assigned
MDT Therapist during pretreatment planning sessions and other team
members when appropriate.
Dear Consumers:
Community Mental Health of Ottawa County has recently implemented a new set of Practice Guidelines for our medication
practices. The guidelines were developed to add consistency in our medication prescribing, to be more consistent with Psychiatric Best
Practices, and to better address our philosophy of treatment. The medications that will be effected by these guidelines are controlled
substances and include: stimulants, benzodiazepines, hypnotics (for sleep), and other medications that may foster dependence. A list of
some of these medications includes:
Xanax
Xanax XR
Librium
Tranxene
Halcion
Adderall
Focalin
Focalin XR
Vyvanse
Ritalin LA
Lunesta
Concerta
Seconal
Restoril
Ritalin SR
Valium
Dalmane
Ativan
Klonopin
Ambien
Ambien CR
Ritalin
Provigil
Other medications may also be affected but not listed above. Your prescriber will discuss your individual situation with
you at your medication review appointment. If you are prescribed medical medications such as pain pills or muscle relaxers this
may also impact the medications you will receive from us.
Guidelines from both state and federal mental health sites note that short term use of these medications may be helpful but
long term use is not recommended. The reasons for this are that the medications are not as effective after a few months and the
potential for becoming dependent on them greatly increases. If an individual is taking the types of medications mentioned above
and is actively using substances, such as: alcohol, street drugs, or certain pain medications, the potential for serious medical
problems greatly increases. National and State guidelines are clear that for individuals with a substance abuse history use of these
medications is not recommended.
Your prescriber will be following recommended guidelines for dosages of these medications and will be limiting the length of
time for these prescriptions. Other medications known to be effective but not addictive will be made available to you.
In addition to medication we will encourage active participation in our therapy program. Everyone experiences
uncomfortable or painful feelings at times and often people believe the medications will take those feelings away. However,
medications are not intended to remove normal painful feelings. Medications are meant to help the person feel the painful
feelings more accurately, and to facilitate the process of developing healthy coping skills. Our therapy program will help you
develop coping skills and better manage your feelings.
Sincerely,
CMHOC Staff
Community Mental Health
Ottawa County
Dr. Michael Brashears, Executive Director
Dear Consumers:
Community Mental Health of Ottawa County has recently implemented a new set of Practice Guidelines
for our medication practices. The guidelines were developed to add consistency in our medication
prescribing, to be more consistent with Psychiatric Best Practices, and to better address our philosophy of
treatment. The medications that will be effected by these guidelines are controlled substances and include:
stimulants, benzodiazepines, hypnotics (for sleep), and other medications that may foster dependence. A list
of some of these medications includes:
Xanax
Xanax XR
Librium
Tranxene
Halcion
Adderall
Focalin
Focalin XR
Vyvanse
Ritalin LA
Lunesta
Concerta
Seconal
Restoril
Ritalin SR
Valium
Dalmane
Ativan
Klonopin
Ambien
Ambien CR
Ritalin
Provigil
Other medications may also be affected but not listed above. Your prescriber will discuss your
individual situation with you at your medication review appointment. If you are prescribed medical
medications such as pain pills or muscle relaxers this may also impact the medications you will receive
from us.
Guidelines from both state and federal mental health sites note that short term use of these
medications may be helpful but long term use is not recommended. The reasons for this are that the
medications are not as effective after a few months and the potential for becoming dependent on them
greatly increases. If an individual is taking the types of medications mentioned above and is actively
using substances, such as: alcohol, street drugs, or certain pain medications, the potential for serious
medical problems greatly increases. National and State guidelines are clear that for individuals with a
substance abuse history use of these medications is not recommended.
Your prescriber will be following recommended guidelines for dosages of these medications and
will be limiting the length of time for these prescriptions. Other medications known to be effective but
not addictive will be made available to you.
In addition to medication we will encourage active participation in our therapy program. Everyone
experiences uncomfortable or painful feelings at times and often people believe the medications will
take those feelings away. However, medications are not intended to remove normal painful feelings.
Medications are meant to help the person feel the painful feelings more accurately, and to facilitate the
process of developing healthy coping skills. Our therapy program will help you develop coping skills
and better manage your feelings.
Sincerely,
CMHOC Staff
12265 James Street, Holland, MI 49424
(616)392-1873 • Fax (616) 393-5687
Qt
Controlled Substance Guidelines
Consumer Reactions <& CMHOC Recommended Resonses
1) Refusing to see a particular prescriber and/or
demands to change prescribers.
a. Staff explains there is (usually) only one
prescriber option per team.
b. Reinforce to consumer that all prescribers
operate from same practice guidelines.
c. Consumer's holder of record brings issue to
next Team Meeting to get input from team
regarding rationale and recommendation to
change prescribers.
i. Coordinate the transfer to an "alternate
but equal" CMHOC MDT, if available, and
consumer is agreeable to receive all CAAH
services from alternate site.
ii. Consumer has the option of finding a new
community prescriber (at his expense) to
prescribe his psychotropic medications
Page two
2) Consumer demands controlled meds from
prescribe!*.
a. Prescriber calmly explains CMHOC Practice
Guidelines, rationale <& plan for slow tapering
to consumer.
b. Prescriber stands firm in response to consumer
demands.
c. Prescriber may choose to do a MAPS search
to check for the possibility of multiple
controlled med prescribers.
d. Consumer has option of making a complaint to
Recipient Rights Officer, if desired.
e. Consumer has option of finding a new
community prescriber (at his expense) for
psycho tropic medications.
f. Prescriber utilizes "panic button" if consumer
refuses to leave office.
Page three
3) Consumer is adamant about wanting to continue
controlled meds, but has no interest in stopping
admitted substance abuse.
a. Prescriber calmly explains rationale, but
remains firm in only prescribing medications
that safe with use of illegal substances.
b. Prescriber may link prescribing practices to
results of regular or irregular urine drug
screens.
c. Consumer has option of making a formal
complaint to CMHOC Recipient Rights Officer.
d. Consumer has option of finding a new
community prescriber (at his expense) for
psycho tropic medications.
Page four
4) Consumer makes threats, either prospectively or
retrospectively, that planned or actual decreases
in controlled medications will (or have) resulted in
increased substance abuse, suicide attempt, etc.
a. Prescriber stands firm in only prescribing
medications that are safe with the use of
illegal substances.
b. Prescriber may link prescribing practices to
the results of regular, or irregular, urine drug
screens.
c. Therapist, Case Manager and Prescriber
reinforce that each consumer has a right to
make his own choices. Coach consumer in
proper steps to take if that choice causes
him/her serious problems, i.e. Call 911, go
the hospital ER, etc.
P. Medications Not Related to Mental Health
1. Only psychotropic medications to be prescribed: Prescribing professionals employed by or
under contract with CMHOC shall not routinely prescribe medications except those
specifically involved in the treatment of psychiatric disorders and side effects
2. Anti-Epileptic Drugs: Anti-epileptic medications will not routinely be prescribed, except
when used for psychiatric diagnosis and/or for behavioral management. Anti-epileptic
medications, when used for non-psychiatric convulsive disorders, will be referred to a
neurologist or other physician.
3. Non-psychotropic medication may only be prescribed temporarily in situations where:
a. The consumer is already using the medication
b. Interruption of the medication might be potentially harmful
c. No other source for obtaining the medication is readily available
d. Medications are prescribed to treat a side effect (document rationale).
Q. Substance Abuse
1. Alcohol and Other Drugs of Abuse Treatment, CMHOC Policy 4.23
2. Handling of Drugs, Weapons and Medications, CMHOC Policy 4.39
3. CMHOC Suboxone Procedure
a. CMHOC Suboxone Treatment Contract
b. Suboxone Patient Assistance Medication Log
c. Suboxone Reimbursement
COMMUNITY MENTAL HEALTH OF OTTAWA COUNTY
INDIVIDUAL CARE TO CONSUMERS
CHAPTER: 4
SECTION: 21
Page 1 of 3
SUBJECT: INDIVIDUAL CARE TO CONSUMERS
TITLE:
ALCOHOL AND OTHER DRUGS OF ABUSE TREATMENT
REVISED DATE:
EFFECTIVE DATE:
12/15/95
11/28/01, 10/19/04, 12/7/04, 8/16/05, 8/7/07, 8/2/10
ISSUED AND APPROVED BY:
vfltMwJl $wLt<4 ' -#sfcy. j)
l
EXECUTIVE DIRECTOR
I.
PURPOSE:
In providing quality mental health care to consumers with developmental disabilities
and/or mental or emotional disorders, a substance-related disorder is recognized as a
limiting factor in achieving self-sufficiency and self-reliance. Therefore, Community
Mental Health of Ottawa County (CMHOC) seeks to assess consumers for the presence
of a substance-related disorder and to address the problem as needed.
II.
APPLICATION:
To all CMHOC providers.
III.
DEFINITIONS:
Substance abuse - Individual has never met the criteria for substance dependence and
has a maladaptive pattern of substance use leading to significant impairment or distress,
as manifested by one or more of the following, occurring within a 12 month period:
a) recurrent substance use resulting in a failure to fulfill major obligation; and/or
b) recurrent substance use in situations in which it is physically hazardous; and/or
c) recurrent substance-related legal problems; and/or
d) continued substance use despite having persistent or recurrent social or
interpersonal problems caused or exacerbated by the effects of a substance
Substance dependence - Individual has a maladaptive pattern of substance use leading
to significant impairment or distress, as manifested by three or more of the following,
occurring within a 12 month period:
a) tolerance,
b) withdrawal,
c) the substance is taken in larger amounts or over longer period than was
intended;
d) there is a persistent desire or unsuccessful efforts to cut down or control
substance use;
e) a great deal of time is spent in activities necessary to obtain the substance;
f) important social, occupational, or recreational activities are given up or
reduced because of substance use;
Substance Abuse 4.21
COMMUNITY MENTAL HEALTH OF OTTAWA COUNTY
INDIVIDUAL CARE TO CONSUMERS
Page 2 of 3
g) the substance use is continued despite knowledge of having a persistent or
recurrent physical or psychological problem that is likely to have been caused or
exacerbated by the substance
IV.
POLICY:
It is the policy of CMHOC to maintain a cohort of staff who are properly credentialed as
providers of treatment for persons with mental illness and co-occurring substance use
disorders, and to be a provider of treatment for persons with mental illness and cooccurring substance use disorders.
CMHOC embraces the notion that dual diagnosis is an expectation and not an exception,
that CMHOC is the preferred provider of service for persons with serious mental illness
and co-occurring substance abuse, that integrated treatment for mental illness and
substance abuse is the preferred mode of service delivery, that both disorders should be
considered primary, that both disorders should be treated within a philosophical disease
and recovery framework, that there is no single correct intervention for individuals with
co-occurring disorders, and that clinical outcomes for individuals with co-occurring
disorders must be individualized and based on stages of change and phase of recovery.
V.
PROCEDURE:
1.
CMHOC will strive to assure that all employees are welcoming of individuals
with co-occurring disorders, and that staff who are providing services for
individuals with co-occurring disorders will display an empathic and hopeful
orientation with the individual.
2.
At the time of request for CMHOC services, persons who are eligible for services
based on their mental illness will be welcomed regardless of their alcohol or drug
abuse or dependence. If a substance-related disorder is reported to be the primary
reason for service in the absence of a co-occurring mental illness/emotional
disturbance/developmental disability, a referral will be made to a community
provider of treatment for substance use disorders.
3.
At the time of the initial psychosocial assessment, individuals will be screened
and assessed for substance use disorders. Service recommendations will be in
accordance with the individual's stage of change and phase of recovery.
4.
Individual and group services for persons with co-occurring disorders will employ
motivational interviewing strategies, substance abuse counseling, and dual
recovery support groups as appropriate to the individual's stage of change and
phase of recovery.
Substance Abuse 4.21
COMMUNITY MENTAL HEALTH OF OTTAWA COUNTY
INDIVIDUAL CARE TO CONSUMERS
Page 3 of 3
5.
Every crisis assessment will include an evaluation of the individual's current and
past substance use and treatment history. A determination will be made as to
whether there is evidence of substance abuse at the time of the assessment, and
whether substance abuse impacts the individual's psychiatric condition. When
substance abuse impacts the individual's psychiatric condition, the emergency
worker will make recommendations for treatment that are in keeping with the
individual's stage of change and phase of recovery. Inpatient detoxification will
be recommended when the individual's substance use puts them at serious
medical risk.
6.
Psychiatric services: Medications for the treatment of substance-related disorders
(e.g., Disulfiram, Methadone, Buprenorphine, Naltrexone) may be prescribed by
Agency prescribers when privileged to do so. Consumers with an identified
substance abuse history or current use may be referred for a substance use lab
screen as indicated by the prescriber.
Provision of necessary non-addictive medication for treatment of psychotic illness
and other known serious mental illness will be initiated or maintained regardless
of continuing substance use. Individuals whose substance use appears to be
significantly risky will warrant closer monitoring or supervision, not treatment
discontinuation.
7.
Referrals to CMHOC by community substance abuse treatment providers will be
accepted for mental health and/or integrated mental health and substance abuse
treatment when it is determined that the individual meets eligibility criteria for
CMHOC services.
VI.
ATTACHMENT:
Revised Controlled Substance Education document
VII.
REFERENCE:
The Michigan Department of Community Health Standards for Mental Health Services,
and DCH Administrative Rules.
Substance Abuse 4.21
COMMUNITY MENTAL HEALTH OF OTTAWA COUNTY
INDIVIDUAL CARE TO CONSUMERS
CHAPTER: 4
SECTION: 39
Page 1 of 2
SUBJECT: INDIVIDUAL CARE TO CONSUMERS
TITLE:
HANDLING OF DRUGS,WEAPONS, AND MEDICATIONS
REVISED DATE:
EFFECTIVE DATE:
9/4/07,1/27/10,12/16/11
6-7-05
ISSUED AND APPROVED BY:
Mt^wJ.
^J^LQ
-^J)
'
'
EXECUTIVE DIRECTOR
I.
PURPOSE:
To establish policy and procedure that addresses the handling of items brought into
CMHOC's program by the persons served and personnel.
II.
APPLICATION:
To all Community Mental Health of Ottawa County (CMHOC) programs.
III.
DEFINITIONS:
Legal Drug - A substance used in the diagnosis, treatment, or prevention of a disease or
as a component of a medication that has been recognized or defined by the U.S. Food,
Drug, and Cosmetic Act. Typically these are most commonly available to the general
public and referred to as:
1.
"over the counter" (OTC) medications
2.
prescription medications (those prescribed by an authorized professional
3.
Alcohol: The use of Alcohol in this country is legal. There are aspects of alcohol
use (such as drinking alcohol before driving and public order offences involving
alcohol) which are controlled by law, but generally the legal controls focus on the
sale of alcohol to others. It is not against the law to produce alcohol in the form of
beer or wine, but distillation is illegal.
Illegal Drugs - are those drugs whose use is considered illegal by any individual in the
United States (e.g. cocaine, crystal meth,) or prescription medications that have not been
prescribed to the individual (e.g. narcotics prescribed to someone else).
Weapons - are described as guns, knives, and any other implement brought to and/or
used on the premises with intent to threaten or inflict harm on someone or something, or
which can be viewed as threatening or harmful to someone or something.
IV.
POLICY:
It is the policy of CMHOC to maintain a safe environment, in conformance with the law.
V.
PROCEDURE:
1.
Consumers and staff who have a need to bring legal medications (with the
exception of alcohol) onto the premises of any CMHOC program must have those
medications in the original container. These medications must be held by the
Handling of Drugs, Weapons, and Medications 4.39
COMMUNITY MENTAL HEALTH OF OTTAWA COUNTY
INDIVIDUAL CARE TO CONSUMERS
Page 2 of 2
consumer or staff to whom they are prescribed, or in keeping with guidelines
contained in the Medication Committee Manual. These medications may not be
distributed to anyone else (consumers or staff).
2.
Illegal drugs are not permitted on the premises of any CMHOC program.
3.
Alcohol is not permitted on the premises of any CMHOC program.
4.
Weapons are not permitted on the premises of any CMHOC program. The only
allowable exception is for on duty police officers who may carry firearms and/or
other weapons in order to protect and serve the public.
5.
Should any of the procedures 1-4 be violated, the appropriate incident report must
be completed by any individual that has knowledge.
6.
Failure to comply with any of the procedures 1-4 may result in:
a. Suspension or termination of service to the consumer, and/or
b. Disciplinary action for staff, and/or
c. Report to law enforcement if harm or threat of harm is present.
VI.
ATTACHMENT:
None applicable.
VII.
REFERENCE:
CARF Standards; Ottawa County Personnel Policy and Procedure 40.000, CMHOC
Medication Manual
Handling of Drugs, Weapons, and Medications 4.39
3. CMHOC Suboxone Procedure
A. Prescribing Staff
1. Prescribers require special certification.
2. Two physicians should share on-call duties for these patients.
3. Other opiates (e.g. Vicodin) cannot be prescribed for the treatment of opiate
withdrawal.
4. Activity Code = H0033 (oral medication administration, direct observation)
B. Patient Eligibility
1. Suboxone treatment is a planned component to a comprehensive treatment
plan that includes substance use counseling. Suboxone treatment is not
available to a Meds-Only patient. The individual receiving Suboxone treatment
should be receiving services in the CMHOC IDDT program. Psychosocial
recovery is essential in addition to Suboxone medication.
2. Office-based induction should be available to those with mild to moderate
withdrawal symptoms as measured by the COW Scale.
3. Withdrawal symptoms measured as greater than moderate (i.e. when a person
becomes "dope sick") requires facility-based sub acute detox (refer to Shoreline
for Medicaid and uninsured, or Pine Rest for insured).
4. One contingency for non-compliance is discontinuing the prescription ("give
one chance to screw up").
5. Relapse is to be expected as a normal part of recovery.
6. Hand select the first patients for Suboxone treatment for better outcomes (i.e.
persons in the action stage of change).
7. Provide Suboxone for those not necessarily in the action stage, but who are
in crisis and likely to be receptive to intervention (strike when the iron is hot,
window of opportunity).
3. CMHOC Suboxone Procedure (Cont.)
C. Cost and Funding
1. Local Holland K-Mart, Walgreens and Wal-Mart stores plan to carry
Suboxone tablets.
2. Private insurance may cover the cost of Suboxone ($150-$300/month).
3. Lakeshore Coordinating Council will pay for counseling.
4. Suboxone requires prior approval for Medicaid to cover the cost. Access
the prior approval form at www.michigan.fhsc.com. When completed,
fax to number indicated on the form. If the individual has Medicaid but
prior approval was not achieved, Medicaid will not pay for this medication.
If, however, the individual received Medicaid coverage subsequent to the
initiation of Suboxone treatment, Medicaid will pay retroactively.
5.
The initial Medicaid authorization will be for 3 months. A secondary request
can be made for an additional 2 months. It's meant to be a 5 month process
for Medicaid consumers. If more than 5 months is requested, MDCH will
be involved in the decision to authorize.
6.
This is a fee-for-service arrangement, i.e. Medicaid will be billed directly for the
cost versus coming out of capitated Medicaid dollars.
7.
Prior approval requires that the individual be involved in formal substance abuse
counseling. This can be through the prescribing psychiatrist, CMH or another
substance abuse agency.
8.
If discharged from the hospital on Suboxone, seek Medicaid approval if on
Medicaid, or apply for patient assistance in conjunction with RESAT if uninsured.
3. CMHOC Suboxone Policy and Procedure (cont.)
D. Induction and Maintenance Procedure
1.
Service will be provided at the James Street CMHOC location only.
2.
Induction will take approximate 1-1/2 hours.
3.
Utilize family therapy room for induction period.
4.
Show DVD on Suboxone to patient prior to induction.
5.
Medical Procedure:
a. Perform History & Physical
b. Write prescription for Suboxone
c. Send patient to pharmacy to obtain Suboxone
d. Administer the COW Scale
e. Instruct patient to drink water.
f. Physician to administer drug sublingually
g. Team Nurse to monitor B/P, Pulse & Respirations every 30 minutes
after administration.
h. Physician to continue administration of additional Suboxone
until patient if "feeling good", usually a total of 8-12mgs.
i. No eating, drinking or talking for the first 30 minutes after medication
is given.
j. Physician to see patient back for med checks on following days, up
to one month later.
Suboxone (cont.)
k. Physician to provide script for interim period. Less than 2mg/day
may result in cravings.
I. Constipation is the most typical side effect. OD is almost impossible.
6.
The longer the taper (i.e. 6-12 months) the better.
7.
Transition out to community physicians those patients who have no mental
health treatment needs once Suboxone has been successful.
Community Mental Health of Ottawa
County
12265 James Street
Holland, MI 49424
393-5600
Fax: 616-393-5657
SUBOXONE TREATMENT CONTRACT
Consumer Name
Date
As a participant in Suboxone® treatment for opioid misuse and dependence, I freely and voluntarily agree to
accept this treatment contract as follows:
1. I agree to keep and be on time to all my scheduled appointments.
2. I agree not to sell, share, or give any of my medication to another person. I understand that such
mishandling of my medication is a serious violation of this agreement and could result in my treatment
being without any recourse for appeal.
3. I agree not to deal, steal, or conduct any illegal or disruptive activities in the doctor's office.
4. I understand that if dealing or stealing or if any illegal or disruptive activities are observed or suspected by
employees of the pharmacy where my Suboxone® filled, that the behavior will be reported to my doctor's
office and could result in my treatment being terminated without any recourse for appeal.
5. I agree that my medication/prescription can only be given to me at my regular office visits. A missed visit
may result in my not being able to get my medication/prescription until the next scheduled visit.
6.1 agree that the medication I receive is my responsibility and I agree to keep it in a safe, secure place. I
agree that lost medication will not be replaced regardless of why it was lost.
7. I agree not to obtain medications from any doctors, pharmacies, or other sources without telling my treating
physician.
8. I understand that mixing Suboxone® with other medications, especially benzodiazepines
®«
®t
®t
(for example, Valium , Klonopin , or Xanax ), can be dangerous. I also recognize that several deaths
have occurred among persons mixing Suboxone® and benzodiazepines (especially if taken outside the
care of a physician, using routes of administration other than sublingual or in higher than recommended
therapeutic doses).
9.1 understand that medication alone is not sufficient treatment for my condition, and 1 agree to participate in
counseling as discussed and agreed upon with my doctor and specified in my treatment plan.
10. I agree to abstain from alcohol, opioids, marijuana, cocaine, and other addictive substances (excepting
nicotine).
11. I agree to provide random urine samples and have my blood alcohol level tested.
12. I understand that violations of the above may be grounds for termination of treatment.
Date
Consumer Signature
t Valium
^ a registered trademark of Roche Products Inc.
Klonopin is a registered trademark of Roche Laboratories Inc.
®
Xanax is a registered trademark of Pharmacia & Upjohn Company
SUBOXONE PATIENT ASSISTANCE MEDICATION LOG
SBATE
PRESCRIBED
FOR
MEDICATION
STRENGTH
LOT NO.
RECEIVED
DISPENSED
TOTAL
INITIALS
, Suboxone Reimbursement
Consumer with Medicare, Part D Insurance
Determine detailed information regarding Medicare, Part D policy, policy number
Contact fax and/or phone numbers for insurance carrier
Do they contract with an outside agency to do prior authorizations?
Consult with CMH provider to determine diagnosis and other clinical
evidence to make a case for Suboxone therapy
Complete PA request form and fax to appropriate source.
Allow a minimum of one week to obtain written response regarding
coverage of Suboxone.
Allow 2-5 additional days for pharmacy to order & receive Suboxone.
This pharmacy order lead time may be needed for each refill of script.
Consumer with Medicaid Insurance
Determine detail information regarding Medicaid Policy
Policy number
Do they belong to a Medicaid HMO?
Contact fax and/or phone numbers for insurance carrier
Do they contract with an outside agency to do prior authorizations?
Consult with CMH provider to determine diagnosis and other clinical
evidence to make a case for Suboxone therapy.
Utilize Michigan Dept of Community Health Pharmacy Program form
(Suboxone specific) if have straight Medicaid.
Complete PA request form and fax information to appropriate source.
Allow a minimum of one week to obtain written response regarding
coverage of Suboxone.
Allow 2-5 additional days for pharmacy to order & receive Suboxone.
This pharmacy order lead time may be needed for each refill of script.
Suboxone Reimbursement (cont.)
Consumer with Medicaid & Medicare, Part D Insurance
Determine detailed information regarding both policies
Policy numbers
Do they belong to a Medicaid or Medicare HMO?
Contact fax and/or phone numbers for each insurance carrier
Do insurance carriers contract with an outside agency for prior authorizations?
Consult with CMH provider to determine diagnosis and other clinical
evidence to make a case for Suboxone therapy.
Utilize Michigan Dept. of Community Health Pharmacy Program form
(Suboxone specific) if have straight Medicaid.
Complete PA request form and fax information to appropriate source(s).
Submit request for prior authorization to Medicare, Part D carrier first. If Suboxone
coverage is denied, then submit to Medicaid insurance carrier.
Allow a minimum of two weeks for final determination by both carriers.
Allow 2-5 additional days for pharmacy to order & receive Suboxone.
This pharmacy order lead time may be needed for each refill of script.
Consumer with Adult Benefit Wavier
Determine policy number and demographic information
Consult with CMH provider to determine diagnosis and other clinical
evidence to make a case for Suboxone therapy.
Complete Michigan Dept. of Community Health Pharmacy Program PA authorization
form (Suboxone specific) and fax to First Health Services.
Allow a minimum of one week for final determination of coverage.
Allow 2-5 additional days for pharmacy to order & receive Suboxone.
This pharmacy order lead time may be needed for each refill of script.
Suboxone Reimbursement fcont.)
Consumers Without Insurance
Consumer may purchase the medication from pharmacy from own funds.
o
Allow 2-5 days for pharmacy to order & receive Suboxone.
o
This pharmacy order lead time may be needed for each refill of the script.
Consumer may complete application and submit all required documentation for Reckitt
Benckiser's Patient Assistance Program.
o Team Nurse or CMA, will coordinate and submit completed applications package
to Reckitt Benckiser.
o
Allow a minimum of four weeks after submitting all required information before we
receive medication (if accepted on their program).
o
Each qualifying patient's physician will receive a monthly supply of Suboxone for
up to 12 months (available as a 2mg or 8mg formulation) delivered directly to their
DEA-registered office location.
o
It will be necessary for consumers to reapply six months following original
application to see if they remain eligible for this program for an additional six
month period.
o
See attached forms & information for additional details.
R. Over-the-Counter (OTC) Medications
1. Over-the-Counter (OTC) Medications include vitamins, herbal products
and many other drugs or medications that can be purchased without
a prescription.
2. In residential settings and Community Based Education settings, OTC
medications require a written prescription from a MD, DO, PA-C or NP
licensed professional for staff to administer to residents/consumers.
3. OTC medications must be listed on InfoScriber, and included in the
Medication Review or Psychiatric Evaluation report. It is required to
include the drug name, strength, route, dosing instructions and the
name of the prescriber. This is the responsibility of the prescriber.
S. Prescriber Documentation
1. Psychiatric Evaluation
a. All consumers will be requested to bring the original containers of all
over-the-counter and prescription medications they receive from any
prescriber, or take without prescriber approval, to their Psychiatric
Evaluation appointment.
b. Prescriber documentation will be completed utilizing the AVATAR
CWS Psychiatric Evaluation format for the initial appointment
with a new consumer.
c. Prescriber will also complete a Psychiatric Evaluation if a consumer's
case is reopened, and the previous Psychiatric Evaluation was
completed more than one year prior.
d. Psychiatric Evaluations for children and adolescents will be scheduled
for 90 minutes.
e.
Psychiatric Evaluations for individuals over the age of 18 will be
scheduled for 60 minutes.
Psychiatric Evaluations
The Psychiatric Evaluation is a stand-alone document reflecting a
thorough assessment and description of the consumer's current and
historical circumstances as they relate to his/her mental illness,
medical conditions and significant psychosocial factors. It should
reflect a high degree of professionalism. It will include presenting
problem with current signs and symptoms, medical history, family
history, treatment history, results of a mental status exam and
document any medication side effects that are currently present or
have resulted in problems in the past. A diagnosis of Axis I-V will be
documented, as well as rationale for all treatment recommendations
and psychotropic medications prescribed.
•
•
•
•
•
•
•
•
•
Psychiatric Evaluations must be finalized within 14 days of
the face-to-face contact.
All sections of the Psychiatric Evaluation template must be
completed. If the section does not apply to the consumer,
indicate "Assessed, none noted" or a similar statement.
All narrative sections must include a complete statement
that summarizes the consumer's current condition.
A statement that the evaluation is a face-to-face meeting
shall be included.
Use full sentences.
Use spell check.
Use correct grammar (e.g. if pronouns are used, ensure that
the reader knows to whom you are referring).
Include a listing of all OTC medications/herbals and
prescriptions medications ordered by other medical health
professionals, including the name, dose, directions and
name of the prescribing professional (InfoScriber).
Ensure that adequate medication refills are authorized to
last until the consumer's next psychiatric appointment
(InfoScriber).
Communicate to the consumer and document when the next
psychiatric appointment should be scheduled.
Obtain consumer's signature on Medication Consent form
and provide adequate education for all prescribed
medications. Sign & complete all appropriate blank spaces
on form.
Obtain consumer's signature on Controlled Substance
Contract when required.
Order lab work as needed to assess the consumer's
response and assure safety of prescribed medications.
Answer all "Yes - No" questions.
PSYCHIATRIC EVALUATION
CLIENT NAME
>•
z
3
O
O
<
Date:
Start Time:
CASE COORDINATOR
Stop Time:
IDENTIFYING INFORMATION / DIAGNOSTIC RATIONALE / SIGNS AND SYMPTOMS
PRESENTING PROBLEM
MEDICAL HISTORY
I
FAMILY HISTORY
MENTAL STATUS EXAM
SIDE EFFECTS
o
u.
O
X
H
<
UJ
DIAGNOSIS
Axis I
Axis II
Axis III
Axis IV
Axis V
TREATMENT RECOMMENDATIONS
CURRENT PSYCHOTROPICS
CONTINUATIONS
X
<
EFFECTIVE
DATE
CHANGES
DOSAGE
#
REFILLS
DOSAGE
#
REFILLS
UJ
5
Ez
3
5
OTHER MEDICATIONS
(Including non-psychiatric medications, herbs, over the counter, etc.)
Is notification to the primary care physician and/or other service provider required as part of this status report or goal?
yes
no
nsumer/family advised of potential suicide risks with antidepressant and/or anticonvulsant medication therapy. O yes Q no Q n/a
RETURN VISIT
O
O
Signature/Credentials:
CMHOC - Psychiatric Evaluation- 03/7 - 046 - MI/DD - 04/22/09
Date:
Case Number:
2. Medication Review
a. After a Psychiatric Evaluation is completed, following appointments
with a prescriber will be documented utilizing the AVATAR CWS
Medication Review template.
b. Medication Review for both children and adults will be scheduled
for 30 minutes.
Medication Reviews
The Medication Review document should provide a thorough picture of
the consumer's current mental status and response to treatment. It
should reflect a high degree of professionalism. Documentation of the
following should be included.
• All sections of the Medication Review template must be
completed. If the section does not apply to the consumer,
indicate "Assessed, none noted" or a similar statement.
• All narrative sections must include a complete statement that
summarizes the consumer's current condition.
• Document whether the consumer is taking all medications as
prescribed. If not, summarize current medication adherence &
consumer's reported rationale.
• Document that the medication review was a face-to-face
meeting.
• Document whether the consumer is having any current
medication side effects. If so, describe symptoms and indicate
which medication(s) may be associated.
• If the consumer is taking antipsychotic medications (other than
Clozaril only), document that AIMS testing was completed at
least every three months.
• Review any lab work results with consumer/guardian that were
received since last psychiatric appointment. Document this
action and any recommendations.
• Review all Axis diagnoses, making changes when needed &
including the rationale.
• Document all psychotropic medication changes & rationale.
• Document all consumer reported medication changes by other
medical professionals (InfoScriber).
Ensure that adequate medication refills are authorized to last
until the consumer's next psychiatric appointment (InfoScriber).
Update & complete Medication Consent form as needed.
Order lab work, when necessary.
Provide and document any medication-related or other education
given to consumer/guardian when applicable.
Answer all "Yes-No" questions.
MEDICATIONREVIEW
I CLIENT NAME
CASE COORDINATOR
I
Date:
Site of Service:
z
Start Time:
Sjtpp Time:
REVIEW OF PROGRESS/DIAGNOSTIC RATIONALE/SIGNS AND SYMPTOMS
D
o
u
MENTAL STATUS EXAM
SIDE EFFECTS
LABORATORY TEST REVIEW
SIGNS AND SYMPTOMS OFTARDIVE DYSKINESIA (AIMS)
•_
O
l_
O
JDIAGNOSIS
Axis I
Axis II
Axis III/ Allergies
"Axislv"
Axis V
CURRENT PSYCHOTROPICS
CONTINUATIONS
EFFECTIVE
DATE
CHANGES
DOSAGE
#
REFILLS
DOSAGE
#
REFILLS
uj
5
OTHER MEDICATIONS
(Including non-psychiatric medications, herbs, over the counter, etc.)
Is notification to the primary care physician and/or other service provider required as part of this report ? Q yes D no
Does face sheet need to be updated? D Yes Q No (e.g. Change in diagnosis, address, guardianship status, advanced directives)
Consumer/family advised of potential suicide risks with antidepressant and/or anticonvulsant medication therapy. D yes D no D n/a
PLAN:
RETURN VISIT:
Prescriber's Signature:
CMHOC - Medication Review- 03/6 - 041- MI/DD - 04/22/09
Date:
Case Number:
3. InfoScriber
a. The prescriber is responsible for documenting the name, strength,
route & dose of all medications prescribed by CMHOC.
b. The prescriber is also responsible for documenting the name of
the prescriber, medication name, strength, route & dose for any overthe-counter medications, as well as prescription medications prescribed
to the consumer by other individuals.
c. Team nurses will also update the InfoScriber allergy, pharmacy and
listing of over-the-counter and non-CMH prescribed medications when
identified through Nursing Assessments and/or communication with
primary care providers.
d. During the Psychiatric Evaluation appointment, is also the prescriber's
responsibility to document on InfoScriber the consumer's Axis I & II
diagnosis, allergies, CMHOC medication prescribed and the individual's
chosen pharmacy.
e. During follow-up Medication Review appointments, the prescriber
will document all CMHOC medication changes, changes in diagnosis,
changes in preferred pharmacy, new allergies and any changes in overthe-counter or prescription medications prescribed by others.
COMMUNITY MENTAL HEALTH OF OTTAWA COUNTY
OPERATIONAL GUIDELINE
TITLE: RN Medication Review Appointments
EFFECTIVE DATE:
REVIEW DATES:
AUTHORED BY: Barb Sychowski, RN BSN
SUBJECT:
Protocol for medication review appointments with a licensed professional nurse (RN)
SCOPE:
Consumers determined to have currently stable mental illness symptoms by a
CMHOC psychiatrist, nurse practitioner or physician assistant assigned prescriber
PURPOSE: Preserve limited Psychiatrist/NP/PA-C appointments for consumers dealing with
unstable mental illness symptoms and/or medication related issues.
Reduce agency cost of providing medication review appointments at CMHOC while
maintaining quality of reviews.
PROCEDURE:
Prescriber identifies consumer as appropriate for RN Medication Review appointment.
Prescriber discusses with consumer the plan for follow-up appointment with
Treatment Team RN at conclusion of current appointment.
Prescriber emails Treatment Team RN to communicate the plan for RN Med Review
and recommendation of interval when consumer should next be scheduled.
Prescriber includes in Plan portion of documented Med Review that consumer will
schedule next appointment for RN Med Review. Plan will include any
recommendations for titration or tapering of prescribed medication, plan to alternate
prescriber and RN med reviews vs. one time only appointment, any plan to refer
consumer to primary care provider, any plan for routine seasonal medication changes
or other appropriate orders.
RN Medication Review appointments may be for one time only or alternate with
Prescriber Med Review appointments. No successive RN Med Review appointments
will be scheduled.
Team Support Staff will assist consumer to schedule a 30 minute appointment in the
appropriate nurse's Lotus Notes calendar at the interval requested by the Prescriber.
RN will utilize current AVATAR CWS Medication Review screens to document details
of appointment and bill for services via Client Charge Input for applicable number of
face to face minutes utilizing code T1002.
RN will initiate a CWS Medication Request progress note, forwarded to referring
prescriber, advising of completed RN Med Review, requesting any medication refills
needed and/or communicating any concerns/issues regarding the consumer.