* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Cutaneous Signs of Systemic Disease (1)
Childhood immunizations in the United States wikipedia , lookup
Osteochondritis dissecans wikipedia , lookup
Germ theory of disease wikipedia , lookup
Globalization and disease wikipedia , lookup
Neonatal infection wikipedia , lookup
Kawasaki disease wikipedia , lookup
Neuromyelitis optica wikipedia , lookup
Tuberculosis wikipedia , lookup
Infection control wikipedia , lookup
Onchocerciasis wikipedia , lookup
Rheumatic fever wikipedia , lookup
Multiple sclerosis signs and symptoms wikipedia , lookup
Schistosomiasis wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Inflammatory bowel disease wikipedia , lookup
Multiple sclerosis research wikipedia , lookup
Behçet's disease wikipedia , lookup
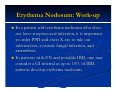
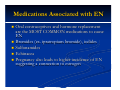
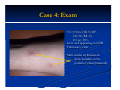
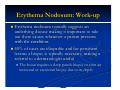
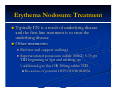
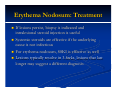
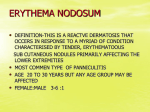
Erythema Nodosum Module Instructions The following module contains hyperlinked information which serves to offer more information on topics you may or may not be familiar with. We encourage that you read all the hyperlinked information. Case 1 Case 1: History HPI: A 35 year-old woman presents with tender erythematous nodules on the anterior shins. The lesions appeared over the course of a few days in crops and have since been resolving with faint bruises remaining. ROS: She notes a sore throat over the past 2 weeks. PMH: none All: none Meds: none FH: non-remarkable SH: lives in the city with husband and 12 year old child who also has a sore throat but no rash Case 1: Exam VS: T-101.7, HR-90, BP110/70, RR-14, O2sat 100% Gen: well appearing HEENT: erythematous oropharynx with some exudate Skin: 5-10 scattered shiny, red nodules on the anterior shins bilaterally Case 1: Question 1 What is the appropriate next step? a. Biopsy the lesion b. Drain the nodules c. Rapid strep test d. Topical clobetasol Case 1: Question 1 Answer: c What is the appropriate next step? a. Biopsy the lesion (diagnosis can be made clinically) b. Drain the nodules (not appropriate) c. Rapid strep test d. Topical clobetasol (may treat the nodules but not the underlying cause) Case 1: Lab Findings Rapid strep test came back positive as well as a positive ASO titer Throat culture shows numerous gram positive cocci in chains consistent with group A strep (GAS) Diagnosis ERYTHEMA NODOSUM CAUSED BY GROUP A STREP INFECTION! Patient received penicillin and the EN resolved. Some Causes of Erythema Nodosum Erythema nodosum can be precipitated by group A strep as well as a number of other conditions Streptococcal infections Tuberculosis GI infection with Yersinia, Salmonella, or Shigella Systemic fungal infections, such as coccidioidomycosis, histoplasmosis, sporotrichosis, and blastomycosis Sarcoidosis Inflammatory bowel disease (Crohn’s > UC) EN is the MOST COMMON skin manifestation in IBD Erythema Nodosum: Basic Facts Erythema nodosum is a form of panniculitis Panniculitis is an inflammatory disorder of the subcutaneous fat This subcutaneous location results in NODULES with poorly defined borders deep in the skin on exam Who gets it? Women are 3-6x more likely to develop erythema nodosum Typically occurs in young adult women Erythema Nodosum: Basic Facts On exam, erythema nodosum typically presents as: Erythematous, shiny tender nodules measuring 110cm in size The nodules appear SYMETRICALLY and BILATERALLY mainly on the anterior shins Scattered lesions can also be found on the upper legs, extensor arms, neck, and rarely face Lesions resolve only with a bruise and DO NOT ulcerate or drain Additionally, patients may present with malaise, leg edema, arthritis, arthralgia, fever, HA, and conjunctivitis Erythema Nodosum: Work-up In a patient with erythema nodosum who does not have streptococcal infection, it is important to order PPD and chest X-ray to rule out tuberculosis, systemic fungal infection, and sarcoidosis In patients with EN and possible IBD, one may consider a GI referral as up to 15% of IBD patients develop erythema nodosum CASE 2 Case 2: History HPI: A 35 year-old woman presents with tender erythematous nodules on the anterior shins. The lesions appeared over the course of a few days in crops and have since been resolving with faint bruises remaining. ROS: negative. PMH: none All: none Meds: oral contraceptive Ortho Tri-Cyclen lo FH: non-remarkable SH: lives in the city with husband, nobody else with rash Case 2: Exam VS: T-98.6, HR-70, BP110/70, RR-14, O2sat 100% Gen: well appearing HEENT: clear oropharynx Lungs: clear Skin: 10-20 scattered shiny, red nodules on the anterior and lateral leg bilaterally Case 2: Question 1 What is the likely cause of the patient’s erythema nodosum? a. Coccidioidomycosis infection b. Ortho tri-cyclen lo c. Tuberculosis d. Crohn’s disease Case 2: Question 1 Answer: b What is the likely cause of the patient’s erythema nodosum? a. Coccidioidomycosis infection (clear lungs, no fever) b. Ortho tri-cyclen lo c. Tuberculosis (clear lungs, no fever) d. Crohn’s disease (unlikely given lack of bowel symptoms although could be presenting symptom) Medications Associated with EN Oral contraceptives and hormone replacement are the MOST COMMON medications to cause EN Bromides (ex. ipratropium bromide), iodides Sulfonamides Echinacea Pregnancy also leads to higher incidence of EN suggesting a connection to estrogen Case 3 Case 3: History HPI: A 50 year-old woman presents with tender erythematous nodules on the posterior calves for the past 2 months. PMH: none All: none Meds: none FH: non-remarkable SH: lives in the city, recent immigrant from Central America Case 4: Exam VS: T-98.6, HR-70, BP120/80, RR-18, O2 sat 98% Gen: well appearing in NAD Pulmonary: clear Skin: tender erythematous shiny nodules on the posterior calves bilaterally Case 4: Question 1 What is the most likely diagnosis? a. Erythema nodosum b. Erythema induratum c. Syphilitic gumma d. none of the above Case 4: Question 1 Answer: b What is the most likely diagnosis? a. Erythema nodosum b. Erythema induratum c. Syphilitic gumma d. none of the above Case 4: Differential Diagnosis Unlikely EN given the atypical location on the posterior calf. Diagnoses considered in this case: Erythema induratum (posterior calf, associated with remote history of tuberculosis, may ulcerate) Atypical mycobacterial infection (lesions drain like abscesses) Abscess/ cellulitis Subcutaneous fat necrosis from pancreatitis Syphilitic gumma (similar to EN but unilateral) Sporotrichosis (similar to EN but unilateral) Case 4: Diagnosis The diagnosis is erythema induratum It is associated with tuberculosis as is EN Typical skin lesions Erythematous painful plaques on nodules located on the posterior calves Lesions may ulcerate if chronic Lesions resolve with scarring and atrophy if they have ulcerated Case 4: Continued If a patient like the one in case 4 had not be diagnosed for many years, the lesions would be more likely to ulcerate On exam, pt has bilateral ulcerated nodules with overlying crust and surrounding rim of erythema Some Additional Points on Erythema Nodosum Erythema Nodosum: Work-up Erythema nodosum typically suggests an underlying disease making it important to rule out these causes whenever a patient presents with the condition. 40% of cases are idiopathic and for persistent lesions a biopsy is typically necessary, making a referral to a dermatologist useful The lesion requires a deep punch biopsy or even an incisional or excisional biopsy due to its depth Erythema Nodosum: Treatment Typically EN is a result of underlying disease and the first line treatment is to treat the underlying disease Other treatments: Bed rest and support stalkings Supersaturated potassium iodide (SSKI) 5-15 gtt TID beginning at 5gtt and titrating up 1 additional gtt/day OR 300mg tablet TID Be cautious of potential HYPOTHYROIDISM Erythema Nodosum: Treatment If lesions persist, biopsy is indicated and intralesional steroid injection is useful Systemic steroids are effective if the underlying cause is not infectious For erythema nodosum, SSKI is effective as well Lesions typically resolve in 3-6wks, lesions that last longer may suggest a different diagnosis END OF MODULE