* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download 32 Isolation Methods For Individual Diseases
Human cytomegalovirus wikipedia , lookup
Brucellosis wikipedia , lookup
Chagas disease wikipedia , lookup
Hepatitis C wikipedia , lookup
Schistosomiasis wikipedia , lookup
Herpes simplex virus wikipedia , lookup
Meningococcal disease wikipedia , lookup
Ebola virus disease wikipedia , lookup
Orthohantavirus wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
West Nile fever wikipedia , lookup
Neisseria meningitidis wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
Hepatitis B wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Henipavirus wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Leptospirosis wikipedia , lookup
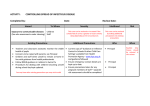
Title Document Type Infection Control Manual Section 3.2 – Isolation Methods for Individual Diseases Policy Document Number IPCT001/02 Version Number 3rd Edition Approved by Infection Control Committee Issue date December 2010 Review date March 2015 Distribution All NHS Borders Staff Prepared by Infection Prevention Control Team Developed by Infection Prevention Control Team Equality & Diversity Impact Assessed No 3.2 ISOLATION METHODS FOR INDIVIDUAL DISEASE Below is a table of possible diseases/infectious agents, together with a note of methods of minimising spread of infection. There may be others which do not appear on the list, please seek advice form the Infection Prevention Control Team CPHM = Consultant in Public Health Medicine IPCT = Infection Prevention Control Team If you suspect that a patient has an infectious condition, please notify a member of the Infection Prevention Control Team immediately DISEASE, CLINICAL CONDITION OR INFECTING AGENT AIDS Adenovirus (Respiratory) INCUBATION PERIOD 4-12 days Droplet & Contact Amoebiasis 2-4 weeks Standard Precautions Anthrax 1-7 days: pulmonary 1-60 days: Cutaneous Standard Precautions IPCT001/02 Issue Date: December 2010 PRECAUTIONS REQUIRED Contact ACCOMMODATION PRECAUTIONS TO BE LIFTED Single Room/Cohort See remarks 2 negative NPA if under two years Single room – consider transfer to ID unit On advice of IPCT UNCONTROLLED WHEN PRINTED ADDITIONAL REMARKS See HIV Spread Droplet and Contact Single Room only required if patient hygiene is poor Bacillus anthracis: Notifiable organsism Anthrax: Notifiable disease See Appendix 1 Review Date: March 2015 DISEASE, CLINICAL CONDITION OR INFECTING AGENT Antibiotic associated colitis Aspergillosis Bordetella pertussis β-haemolytic Streptococci Group A (Strep. Pyogenes) Group B Burkholderia cepacia Burkholderia (Pseudomonas) mallei Burkholderia (Pseudomonas) pseudomallei Campylobacter INCUBATION PERIOD PRECAUTIONS REQUIRED ACCOMMODATION Up to 8 weeks Enteric & contact Single room source isolation Days to weeks Standard Precautions Open Ward Not applicable Contact Single Room Not applicable Contact Single Room / cot/incubator for neonates PRECAUTIONS TO BE LIFTED 48hrs after diarrhoea stops and patient has passed a formed stool Not applicable See also Clostridium difficile See Whooping Cough 48hrs correct antibiotics 1-14 days Contact Single Room On advice of IPCT 2 daysmonths Standard Precautions Open Ward On advice of IPCT 1-10 days Enteric & Contact Single Room source isolation 48hrs after diarrhoea has stopped IPCT001/02 Issue Date: December 2010 ADDITIONAL REMARKS See Pneumonia Notifiable Disease 3 UNCONTROLLED WHEN PRINTED Review Date: December 2013 DISEASE, CLINICAL CONDITION OR INFECTING AGENT Chickenpox see also Herpes zoster/shingles INCUBATION PERIOD 12-21 days PRECAUTIONS REQUIRED Respiratory and Contact ACCOMMODATION Single room source isolation PRECAUTIONS TO BE LIFTED When last vesicle crop dry. Patients are infectious from day 10 to day 21 post exposure Cholera Hours-5 days Enteric & Contact Single room consider transfer to ID ward/ID unit 3 negative stool cultures at least 24hrs apart Clostridium difficile Not applicable Enteric & Contact Single room source isolation 48hrs after diarrhoea stops and patient has passed a formed stool IPCT001/02 Issue Date: December 2010 ADDITIONAL REMARKS KEEP DOOR CLOSED Risk to non-immune pregnant staff. Notifiable Disease: See Appendix 1 See Chickenpox Policy Notifiable disease See Appendix 1 Refer also to enteric precautions, Section 3.4 If relapse occurs reinstate precautions and inform IPCT. See C.difficile Policy Room must be subject to a terminal clean even if asymptomatic patient remains in situ 4 UNCONTROLLED WHEN PRINTED Review Date: December 2013 DISEASE, CLINICAL CONDITION OR INFECTING AGENT Conjunctivitis (neonatal) Gonococcal / Chlamydial Adenoviral INCUBATION PERIOD PRECAUTIONS REQUIRED 4-12 days Contact Not applicable 2-5 days ADDITIONAL REMARKS Conjunctival secretions infectious After 24hrs antibiotics When symptoms settle Standard Precautions Open Ward Not Applicable Droplet On advice of IPCT/ID Physician Notifiable disease See Appendix 1 3-6 days Contact 15mths-30yrs Standard Precautions Single room consider transfer to ID ward/ID unit Open Ward Open Ward On Discharge Cryptococcosis Unknown Standard Precautions Open Ward* On Discharge Cryptosporisiosis 1-21 days Enteric & Contact Single room – consider transfer to ID unit On Discharge See CJD Policy See respiratory infections in infants and young children *If immunocompromised may need protective isolation Risk to Immunocompromised patients. See enteric precautions policy Corynebacterium diphtheriae [toxigenic strain] Coxsackievirus Creutzfelt Jakob Disease Croup Contact PRECAUTIONS TO BE LIFTED Single room source isolation Single room source isolation Other 2-7 days ACCOMMODATION IPCT001/02 Issue Date: December 2010 Conjunctival and nasal secretions may be infectious 5 UNCONTROLLED WHEN PRINTED Review Date: December 2013 DISEASE, CLINICAL INCUBATION CONDITION OR PERIOD INFECTING AGENT Cytomegalovirus (CMV) 3-8 weeks PRECAUTIONS REQUIRED ACCOMMODATION PRECAUTIONS TO BE LIFTED ADDITIONAL REMARKS Standard Precautions Open Ward On Discharge Single room source isolation 48 hours clear of symptoms See Corynebacterium diphtheriae On advice of IPCT On advice of IPCT Immunocompromised patients may excrete virus in urine. Risk to pregnant staff, Infants with congenital CMV shed vast quantities of virus in their respiratory secretions and urine Diarrhoea of unknown origin Diphtheria Not applicable Enteric & Contact Dysentery Amoebic Shigella (bacillary) 2-4 weeks Enteric & Contact 8hrs-7days Enteric & Contact IPCT001/02 Issue Date: December 2010 Single room source isolation Single room source isolation Notifiable disease See Appendix 1 Shigella genus Notifiable organism See Appendix 1 6 UNCONTROLLED WHEN PRINTED Review Date: December 2013 DISEASE, CLINICAL CONDITION OR INFECTING AGENT Erysipelas (GP A Strep Streptococcus pyogenes) E. coli gastro-enteritis Enterohaemorrhagic Gas gangrene German measles Giardiasis multi drug resistant gram negative organisms INCUBATION PERIOD PRECAUTIONS REQUIRED ACCOMMODATION PRECAUTIONS TO BE LIFTED 1-3 days Contact Single room source isolation 48hrs correct antibiotics 3-8 days Enteric & Contact Single room source isolation Not applicable Standard Precautions Open Ward 48hrs after return of normal bowel habit. Note: there are specific occupational exclusions – see advice from IPCT Not applicable 5-28 days Enteric & Contact Single room source isolation n/a Standard precautions with attention to the site of infection or colonisation e.g. wound, catheter urines, sputum Single room source isolation IPCT001/02 Issue Date: December 2010 On discharge or following >48 hours free of symptoms Discuss with IPCT ADDITIONAL REMARKS Gastro-enteritis/ clinical syndrome E. coli O157/VTEC (not UTI or wound infection) Notifiable organism See Appendix 1 See Rubella 7 UNCONTROLLED WHEN PRINTED Review Date: December 2013 DISEASE, CLINICAL CONDITION OR INFECTING AGENT Glandular Fever (Infectious mononucleosis) Hand, foot and mouth disease (coxsackie A) Hepatitis A INCUBATION PERIOD PRECAUTIONS REQUIRED ACCOMMODATION PRECAUTIONS TO BE LIFTED ADDITIONAL REMARKS 4-6 weeks Standard Precautions Open Ward 3-5 days Enteric & Contact Single room source isolation On advice of IPCT 15-50 days Enteric & Contact Single room source isolation Notifiable organism See schedule 1 of Public Health Act 2008 Hepatitis B (inc HBeAg positive) 45-180 days Standard Precautions Single Room if bleeding. Renal units please check with IPCT After 2 weeks illness 7 days after onset of jaundice On discharge Hepatitis C 14-80 days Standard Precautions Single Room if bleeding. Renal units please check with IPCT On discharge Notifiable organism See Appendix 1 IPCT001/02 Issue Date: December 2010 Notifiable organism See Appendix 1 8 UNCONTROLLED WHEN PRINTED Review Date: December 2013 DISEASE, CLINICAL CONDITION OR INFECTING AGENT Hepatitis E INCUBATION PERIOD PRECAUTIONS REQUIRED ACCOMMODATION PRECAUTIONS TO BE LIFTED ADDITIONAL REMARKS 15-64 days Enteric & Contact Single room source isolation After 2 weeks illness Notifiable organism See Appendix 1 Herpes simplex (coldsore) 2-12 days Standard Precautions Open Ward Not applicable Herpes zoster (See Shingles) HIV Not applicable 1-3 mths Risk to the eczematous, the immuno-suppressed and to neonates Standard Precautions See remarks On discharge Impetigo Not applicable Contact Single room source isolation 48hrs correct antibiotics See Blood and body fluid precautions; no isolation required, unless one/more of the following: Profuse or uncontrolled bleeding Open drains Incontinent Diarrhoea/vomiting Unconscious IPCT001/02 Issue Date: December 2010 9 UNCONTROLLED WHEN PRINTED Review Date: December 2013 DISEASE, CLINICAL CONDITION OR INFECTING AGENT Influenza 1-3 days Legionnaire’s Disease Leptospirosis Lice Head Body Pubic INCUBATION PERIOD ACCOMMODATION PRECAUTIONS TO BE LIFTED ADDITIONAL REMARKS Droplet Single room source isolation Influenza virus Notifiable organism See Appendix 1 Refer to respiratory precautions, Section 3.5 2-10 days Standard Precautions Open Ward Usually after 7 days; in the absence of fever and/or other respiratory symptoms for more than 24 hours Not applicable 4-19 days Standard Precautions Open Ward Not applicable Leptospira genus Notifiable organism See Appendix 1 Not applicable Not applicable Not applicable IPCT001/02 Issue Date: December 2010 PRECAUTIONS REQUIRED Standard Precautions Open Ward Standard Precautions Open Ward Standard Precautions Open Ward Standard precautions will still apply After successful Treatment After successful Treatment [Consider referral to GUM service] Legionella genus Notifiable organism See Appendix 1 See Head Lice Policy Ensure clothing is laundered and ironed Ensure clothing is laundered and ironed 10 UNCONTROLLED WHEN PRINTED Review Date: December 2013 DISEASE, CLINICAL CONDITION OR INFECTING AGENT Listeriosis INCUBATION PERIOD 3-70 days Lyme disease PRECAUTIONS REQUIRED ACCOMMODATION PRECAUTIONS TO BE LIFTED ADDITIONAL REMARKS Enteric & Contact Single room source isolation On advice of IPCT 3-32 days Standard Precautions Open Ward Not applicable Listeria monocytogenes Notifiable organism See Appendix 1 May be open ward if stool, or discharges negative Borrelia burgdorferi Notifiable organism See Appendix 1 Malaria Strain dependent Standard Precautions Open Ward On advice of IPCT Plasmodium spp Notifiable organism See Appendix 1 Measles 7-14 days Droplet & Contact Single room source isolation 4 days after onset of rash Notifiable disease See Appendix 1 TRUE AIRBRONE INFECTION – KEEP DOOR CLOSED IPCT001/02 Issue Date: December 2010 11 UNCONTROLLED WHEN PRINTED Review Date: December 2013 DISEASE, CLINICAL CONDITION OR INFECTING AGENT Meningitis Meningococcal (known or suspected) INCUBATION PERIOD PRECAUTIONS REQUIRED ACCOMMODATION PRECAUTIONS TO BE LIFTED After 24 hours appropriate therapy 2-10 days Droplet & Contact Single room source isolation Meningitis Pre-organism identification Not applicable Droplet & Contact Single room source isolation until confirmed nonmeningococcal Meningococcal septicaemia (known or suspected) 2-10 days Droplet & Contact Single room source isolation IPCT001/02 Issue Date: December 2010 After 24 hrs appropriate therapy ADDITIONAL REMARKS Neisseria meningitides Notifiable organism Meningococcal disease: Notifiable disease See Appendix 1 Only patients with meningococcal meningitis require a single room. For all other causal organisms including viral, Standard Precautions apply Neisseria meningitides Notifiable organism Meningococcal disease: Notifiable disease See Appendix 1 12 UNCONTROLLED WHEN PRINTED Review Date: December 2013 DISEASE, CLINICAL CONDITION OR INFECTING AGENT Meticillin Resistant Staphylococcus Aureus (MRSA) INCUBATION PERIOD PRECAUTIONS REQUIRED ACCOMMODATION PRECAUTIONS TO BE LIFTED ADDITIONAL REMARKS Usually 3 negative sets of swabs at least 1 week apart 9 days after symptom onset Discuss with IPCT 48hrs correct antibiotics See Strep. pyogenes 48 hrs after symptoms stop Norovirus: Notifiable disease See Appendix 1 Not applicable Contact Single room source isolation Mumps 15-18 days Droplet Single room source isolation Necrotising enterocolitis Not applicable Not applicable Standard Precautions Open Ward Contact Single room source isolation 6-72 hrs Enteric/Contact/Droplet Cohort/Single room source isolation Necrotising fasciitis [due to Streptococcus pyogenes] Norovirus Norwalk like virus Viral gastroenteritis Orf 3-6 days IPCT001/02 Issue Date: December 2010 Standard Precautions Open Ward Mumps virus: Notifiable organism Mumps disease: Notifiable disease See Appendix 1 Aerosolisation of the virus may occur during vomiting See Last Offices SOP 13 UNCONTROLLED WHEN PRINTED Review Date: December 2013 DISEASE, CLINICAL CONDITION OR INFECTING AGENT Paratyphoid fevers INCUBATION PERIOD 3-28 days Parvovirus B19 4-20 days PRECAUTIONS REQUIRED ACCOMMODATION PRECAUTIONS TO BE LIFTED Enteric & Contact Single room source isolation Droplet Single room source isolation 48 hours after Notifiable disease symptoms cease See Appendix 1 Occupational exclusion may be an issue Duration of illness Pediculosis (see lice) Pneumocystis Pneumonia Atypical Burkholderia cepacia in cystic fibrosis patients Bronchopneumonia Chlamydia pneumoniae Legionellosis Multi-drug resistant organism ADDITIONAL REMARKS Standard Precautions 6-32 days Unknown Standard Precautions Standard precautions Open Ward Side Room 1-3 days Unknown Standard Precautions Standard Precautions Open Ward Open Ward 2-10 days Not applicable Standard Precautions Droplet & Contact Open Ward Single room source isolation IPCT001/02 Issue Date: December 2010 Not applicable On advice of IPCT Not applicable Not applicable Not applicable Duration of illness Avoid nursing with other cystic patients If ventilated take care with condensate from ventilator i.e. wear gloves and wash hands when emptying 14 UNCONTROLLED WHEN PRINTED Review Date: December 2013 DISEASE, CLINICAL CONDITION OR INFECTING AGENT Mycoplasma Pneumococcal (lobar) Staphylococcal S. pyogenes S. pneumoniae penicillin resistant S. pneumoniae penicillin sensitive Poliomyelitis (acute) Pseudomembranous colitis INCUBATION PERIOD PRECAUTIONS REQUIRED ACCOMMODATION 6-32 days 1-3 days Not applicable Droplet Standard Precautions Standard Precautions Not applicable 1-3 days Droplet 1-3 days Standard Precautions 7-14 days Droplet/Enteric/Contact Single room source After week 1, faecal isolation, consider oral route transfer to specialist neurological unit Droplet Open Ward Open Ward Open Ward [However, if this is an MRSA and the patient is expectorating, then Single room source isolation is required] Single room source isolation Single room source isolation Open Ward Up to 8 wks IPCT001/02 Issue Date: December 2010 PRECAUTIONS TO BE LIFTED ADDITIONAL REMARKS Not applicable Not applicable Not applicable 48 hrs correct antibiotics When negative specimen 48hrs correct antibiotics Not applicable Virus may be detected in faeces for up to 6 weeks Polio virus: Notifiable organism Poliomyelitis: Notifiable disease See Appendix 1 See Clostridium difficile 15 UNCONTROLLED WHEN PRINTED Review Date: December 2013 DISEASE, CLINICAL CONDITION OR INFECTING AGENT Psittacosis INCUBATION PERIOD PRECAUTIONS REQUIRED 1-4 wks Standard Precautions Puerperal sepsis Strep. pyogenes 1-3 days Contact ACCOMMODATION PRECAUTIONS TO BE LIFTED ADDITIONAL REMARKS Open Ward Coughing patients to cover mouth Person to person rare Single room source isolation 48hrs correct antibiotics Streptococcus pyogenes [Gp A Strep] from sterile space: Notifiable organism See Appendix 1 Rabies Rash undiagnosed 3-8 wks Not applicable IPCT001/02 Issue Date: December 2010 Standard Precautions Droplet & Contact Single room source isolation – consider transfer to ID unit On advice of IPCT Single room source isolation On diagnosis or after treatment Maintain precautions if specimens continue positive Rabies virus Notifiable organism Rabies: Notifiable disease See Appendix 1 Inform IPCT 16 UNCONTROLLED WHEN PRINTED Review Date: December 2013 DISEASE, CLINICAL CONDITION OR INFECTING AGENT Respiratory infections in infants and young children Bronchiolitis/Respiratory syncytial virus infections in infants, young children and immunosurppressed Ringworm Rotavirus gastroenteritis Rubella [German Measles] INCUBATION PERIOD PRECAUTIONS REQUIRED ACCOMMODATION PRECAUTIONS TO BE LIFTED ADDITIONAL REMARKS Includes Adenovirus, Parainfluenza and Influenza It may be necessary to remove some immuno-compromised patients to avoid exposure See Tinea (Aerosolisation of the virus may occur during vomiting) Rubella virus: Notifiable organism Rubella: Notifiable disease See Appendix 1 Pregnant staff should seek advice from occupational health before nursing patient 3-8 days Droplet & Contact Single room source isolation or Cohort 5-8 days Droplet Single room source isolation or Cohort 4-10 days 24-72 hrs 2 Negative NPA taken 24hrs apart On advice of IPCT in adults or two negative NPA’s in the under 2 year old Droplet & Enteric Single room source isolation or Cohort On advice of IPCT 14-17 days Droplet Single room source isolation 7 days after onset of rash IPCT001/02 Issue Date: December 2010 17 UNCONTROLLED WHEN PRINTED Review Date: December 2013 DISEASE, CLINICAL CONDITION OR INFECTING AGENT Congenital Rubella INCUBATION PERIOD PRECAUTIONS REQUIRED ACCOMMODATION PRECAUTIONS TO BE LIFTED ADDITIONAL REMARKS Infants with congenital rubella syndrome shed vast quantities of virus in their respiratory secretions and urine See also Typhoid, Paratyphoid Not applicable Droplet & Contact Single room source isolation On advice of IPCT Salmonella species 6-72 hrs Enteric & Contact Single room source isolation Scabies 2-6 wks Contact Single room source isolation required for ‘Norwegian’ Scabies [drop comment in from scabies policy] Scalded skin syndrome Not applicable Standard Precautions Open Ward 48 hours after, On advice of IPCT Completion of first course of treatment unless diagnosed with ‘Norwegian’ Scabies, then please contact IPCT for advice Not applicable 2-6 wks 8hrs-8days Standard Precautions Enteric & Contact Scarlet fever Schistomosomiasis Shigella IPCT001/02 Issue Date: December 2010 See Streptococcus pyogenes Open Ward Single room source isolation Not applicable 48 hours Shigella genus: On advice of Notifiable organism IPCT/ID physician See Appendix 1 18 UNCONTROLLED WHEN PRINTED Review Date: December 2013 DISEASE, CLINICAL CONDITION OR INFECTING AGENT Shingles (herpes zoster) (For immunocompromised treat as chickenpox) Staphylococcus aureus Most strains MRSA not VISA/VRSA Streptococcus pyogenes (Gp A) Erysipelas Tonsillitis INCUBATION PERIOD Not applicable Not applicable PRECAUTIONS REQUIRED Contact Standard Precautions ACCOMMODATION PRECAUTIONS TO BE LIFTED ADDITIONAL REMARKS Single room source isolation until vesicles dry When vesicles dry. Requires risk assessment by IPCT Non chicken pox immune staff are also advised to avoid contact with patients Open Ward Not applicable Contact Single room source isolation On advice of IPCT 1-3 days Contact 1-3 days Droplet Single room source isolation Single room source isolation 48hrs correct antibiotics 48hrs correct antibiotics IPCT001/02 Issue Date: December 2010 Staphylococcus aureus [all blood isolates]: Notifiable organism See Appendix 1 May need single room source isolation if oozing pus See section 7 19 UNCONTROLLED WHEN PRINTED Review Date: December 2013 DISEASE, CLINICAL CONDITION OR INFECTING AGENT Scarlet fever INCUBATION PERIOD 1-3 days PRECAUTIONS REQUIRED Droplet ACCOMMODATION PRECAUTIONS TO BE LIFTED ADDITIONAL REMARKS Single room source isolation 48hrs correct antibiotics Streptococcus pyogenes [Gp A Strep] from sterile space: Notifiable organism See Appendix 1 Necrotising fasciitis Not applicable Contact Single room source isolation 48hrs correct antibiotics Puerperal fever 1-3 days Contact Single room source isolation 48hrs correct antibiotics Syphilis [same as H simplex Primary or secondary Syphilis Tertiary or latent Necrotising fasciitis: Notifiable disease See Appendix 1 Streptococcus pyogenes [Gp A Strep] from sterile space: Notifiable organism See Appendix 1 10days3mths Weeks-years IPCT001/02 Issue Date: December 2010 Standard Precautions Single Room Standard Precautions Single Room if lesions present 48hrs correct antibiotics On advice of IPCT 20 UNCONTROLLED WHEN PRINTED Review Date: December 2013 DISEASE, CLINICAL CONDITION OR INFECTING AGENT Tetanus INCUBATION PERIOD 3-21 days PRECAUTIONS REQUIRED Standard Precautions ACCOMMODATION PRECAUTIONS TO BE LIFTED ADDITIONAL REMARKS Open Ward Not applicable Notifiable disease See Appendix 1 Standard Precautions Open Ward Not applicable Standard Precautions Open Ward Not applicable Single Room if severe Toxic shock syndrome [see Gp A strep] Toxocara Toxoplasmosis Not applicable Not applicable Not applicable 4-10 yrs 10-23days Single room may be needed for general care [see also ‘non meningococcal meningitis’] See Candidiasis Standard Precautions Open Ward Not applicable Standard Precautions Standard Precautions Open Ward Open Ward Not applicable Not applicable Trichomonas 4-20days Standard Precautions Open Ward Not applicable Thrush [Candidiasis] Tinea (fungus infection) IPCT001/02 Issue Date: December 2010 Toxoplasma gondii Notifiable organism See Appendix 1 21 UNCONTROLLED WHEN PRINTED Review Date: December 2013 DISEASE, CLINICAL CONDITION OR INFECTING AGENT Tuberculosis – pulmonary smear positive Tuberculosis – multiresistant (suspected or proven) INCUBATION PERIOD PRECAUTIONS REQUIRED 2-10weeks for reaction. Years for infection Droplet & Contact 2-10weeks for reaction. Years for infection IPCT001/02 Issue Date: December 2010 Droplet & Contact ACCOMMODATION PRECAUTIONS TO BE LIFTED ADDITIONAL REMARKS Single room source isolation* After 2 wk compliant treatment plus clinical improvement e.g. remaining afebrile for at least 48hrs. TB patients should not be removed from isolation unless on the advice of the IPCT M. tuberculosis & M. bovis: Notifiable organisms Tuberculosis [respiratory or nonrespiratory]: Notifiable disease See Appendix 1 Transfer to ID unit/ID ward On advice of IPCT Preferably Single room source isolation negative pressure for patients with open pulmonary TB As above 22 UNCONTROLLED WHEN PRINTED Review Date: December 2013 DISEASE, CLINICAL CONDITION OR INFECTING AGENT Tuberculosis Draining abscess or cavity e.g. meningitis Typhoid/Paratyphoid Typhoid fever and carriers INCUBATION PERIOD PRECAUTIONS REQUIRED 2-10 weeks for reaction. Years for infection Standard Precautions 8-14days Enteric & Contact ACCOMMODATION PRECAUTIONS TO BE LIFTED ADDITIONAL REMARKS Single room source isolation When lesions no longer draining Notifiable disease: See Appendix 1 Occupational exclusion may be an issue Do not aerosolise exudate from tuberculosis cavities or draining lesions Salmonella [human] species: Notifiable organisms Single room source isolation Notifiable diseases: See Appendix 1 Vancomycin resistant enterococci; Multi drug resistant gram negatives Not applicable Varicella IPCT001/02 Issue Date: December 2010 Enteric & Contact Single room source isolation – Risk assessment will be carried out in Mental Health Partnership Sites Requires risk assessment by IPCT See Chickenpox 23 UNCONTROLLED WHEN PRINTED Review Date: December 2013 DISEASE, CLINICAL CONDITION OR INFECTING AGENT Viral Haemorrhagic Fevers [VHF’s] (suspected or confirmed) INCUBATION PERIOD 6-21days PRECAUTIONS REQUIRED Contact ACCOMMODATION PRECAUTIONS TO BE LIFTED ADDITIONAL REMARKS Discuss with ID unit in first instance and alert on-call Microbiology Consultant On advice of IPCT VHF viruses: Notifiable organisms VHF’s: Notifiable disease See Appendix 1 Viral hepatitis Whooping cough (Pertussis) 7-20days Droplet Single room source isolation After 7 days erythromycin See VHF Policy Notifiable Organism/ Disease. See Hepatitis Bordetella pertussis: Notifiable organism. Pertussis: Notifiable disease See Appendix 1 Infectious for 3 weeks after onset if no antibiotics IPCT001/02 Issue Date: December 2010 24 UNCONTROLLED WHEN PRINTED Review Date: December 2013 DISEASE, CLINICAL CONDITION OR INFECTING AGENT Worms Threadworms Yellow fever INCUBATION PERIOD PRECAUTIONS REQUIRED Standard Precautions 3-6days IPCT001/02 Issue Date: December 2010 Standard Precautions ACCOMMODATION PRECAUTIONS TO BE LIFTED On advice of IPCT Until treated Open Ward Until 2 negative stools cultures commencing 1 and 2 weeks post treatment Not applicable ADDITIONAL REMARKS Yellow fever virus: Notifiable organism Yellow Fever: Notifiable disease See Appendix 1 25 UNCONTROLLED WHEN PRINTED Review Date: December 2013 Infections which should be referred to a specialist Infectious Disease Unit Although many infections can be dealt with adequately in a general hospital, there are some diseases which require very strict source isolation. Such patients should ideally never be admitted but sent to a specialist Infectious Diseases Unit. If a patient is suspected to have one of the following, please contact the Infection Prevention Control Team immediately • • • • • • • • Anthrax Diphtheria Plague Viral Haemorrhagic Fever, e.g. Lassa, Marburg, Ebola. Rabies Smallpox Tuberculosis (suspected / known Multi Drug Resistant, MDR) SARS Notification of infectious disease Implementation commenced on 1st Jan 2010 of part 2 Public Health etc. (Scotland) Act 2008: notifiable diseases, organisms and health risk states. A duty is placed on a registered medical practitioner, who has reasonable grounds to suspect (i.e. not await laboratory confirmation), that a patient they are attending to has a notifiable disease to: Notify in writing to Public Health using the specified ‘Notification Form’ (available from Public Health or the ‘Health Protection’ Intranet microsite) within 3 days of forming that suspicion Make an urgent telephone notification as soon as reasonably practicable if significant concern exists regarding the nature of the disease, the ease of transmission of that disease, the patient’s circumstances and any guidance issued by Scottish Ministers. All urgent oral notifications must be followed up, with the completed ‘Notification Form’, within 3 days of suspicion. IPCT001/02 Issue Date: December 2010 26 Review Date: December 2013 UNCONTROLLED WHEN PRINTED Appendix 1 SCHEDULE 1 [Public Health etc. (Scotland) Act 2008] LISTS OF NOTIFIABLE DISEASES AND NOTIFIABLE ORGANISMS Part 1 Notifiable Diseases • • • • • • • • • • • • • • • • • • • • • • • • • • • Anthrax Botulism Brucellosis Cholera Clinical syndrome due to E.coli O157 infection (see Note 1) Diphtheria Haemolytic Uraemic Syndrome (HUS) Haemophilus influenzae type b (Hib) Measles Meningococcal disease Mumps Necrotizing fasciitis Paratyphoid Pertussis Plague Poliomyelitis Rabies Rubella Severe Acute Respiratory Syndrome (SARS) Smallpox Tetanus Tuberculosis (respiratory or non-respiratory) (see Note 2) Tularemia Typhoid Viral haemorrhagic fevers West Nile fever Yellow Fever *It is recommended that those diseases above marked with an * require urgent notification, i.e. within the same working day. Note 1: E.coli O157 Clinical suspicion should be aroused by (i) likely infectious bloody diarrhoea or (ii) acute onset non-bloody diarrhoea with a biologically plausible exposure and no alternative explanation. Examples of biologically plausible exposures include: IPCT001/02 Issue Date: December 2010 27 Review Date: December 2013 UNCONTROLLED WHEN PRINTED • contact with farm animals, their faeces or environment • drinking privately supplied or raw water • eating foods such as undercooked burgers or unpasteurised dairy products • contact with a confirmed or suspected case of VTEC infection. Cases notified as HUS (Haemolytic Uraemic Syndrome) should NOT be notified as “Clinical syndrome due to E.coli O157 infection” as well. Note 2: Tuberculosis Pulmonary TB is tuberculosis of the lung parenchyma and/or the tracheobronchial tree. Non-pulmonary TB is tuberculosis of any other site. Where tuberculosis is clinically diagnosed in both pulmonary and nonpulmonary sites, this should be treated as pulmonary TB. If you are in any doubt about the diagnosis of suspected cases, you should contact the Health Protection Team for advice on 01896 825560 Part 2 Notifiable Organisms: Bacillus anthracis Bacillus cereus Bordetella pertussis Borrelia burgdorferi Brucella genus Campylobacter genus Chlamydia psittaci Clostridium botulinum Clostridium difficile Clostridium perfringens Clostridium tetani Corynebacterium diphtheriae (toxigenic strains) Corynebacterium ulcerans Coxiella burnetii Crimean-Congo haemorrhagic fever virus Cryptosporidium IPCT001/02 Issue Date: December 2010 28 Review Date: December 2013 UNCONTROLLED WHEN PRINTED Dengue virus Ebola virus Echinococcus genus Verocytotoxin-producing E.coli (VTEC) Francisella tularensis Giardia lamblia Guanarito virus Haemophilus influenzae type b (from blood, cerebrospinal fluid or other normally sterile site) Hantavirus Hepatitis A virus Hepatitis B virus Hepatitis C virus Hepatitis E virus Influenza virus (all types, including those caused by a new sub-type) Junín virus Kyasanur Forest disease virus Lassa virus Legionella genus Leptospira genus Listeria monocytogenes Machupo virus Marburg virus Measles virus Mumps virus Mycobacterium bovis Mycobacterium tuberculosis complex Neisseria meningitidis Norovirus Omsk haemorrhagic fever virus Plasmodium falciparum, vivax, ovale and malariae Polio virus Rabies virus Rickettsia prowazekii Rift Valley fever virus Rubella virus Sabia virus Salmonella (all human types) SARS-associated coronavirus Shigella genus Enterotoxigenic Staphylococcus aureus Staphylococcus aureus (all blood isolates) Methicillin-resistant Staphylococcus aureus (MRSA) Streptococcus pyogenes (from blood, cerebrospinal fluid or other normally sterile site) IPCT001/02 Issue Date: December 2010 29 Review Date: December 2013 UNCONTROLLED WHEN PRINTED Streptococcus pneumoniae (from blood, cerebrospinal fluid or other normally sterile site) Toxoplasma gondii Trichinella genus Varicella-zoster virus Variola virus Vibrio cholerae West Nile fever virus Yellow Fever virus Yersinia enterocolitica Yersinia pestis Yersinia pseudotuberculosis Public Health etc. (Scotland) Act 2008 IPCT001/02 Issue Date: December 2010 30 Review Date: December 2013 UNCONTROLLED WHEN PRINTED