* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Marfan Syndrome Guide
Coronary artery disease wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Myocardial infarction wikipedia , lookup
Cardiothoracic surgery wikipedia , lookup
Williams syndrome wikipedia , lookup
DiGeorge syndrome wikipedia , lookup
Artificial heart valve wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Down syndrome wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
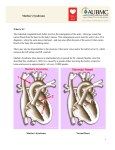
Marfan Syndrome Guide MARFAN SYNDROME guide What is Marfan syndrome? Marfan syndrome (also called Marfan’s syndrome or Marfans syndrome) is a condition that affects the connective tissue. Connective tissue holds the body together and provides support to many structures throughout the body. In Marfan syndrome, the connective tissue isn’t normal. As a result, many body systems are affected, including the heart, blood vessels, bones, tendons, cartilage, eyes, nervous system, skin and lungs. What causes Marfan syndrome? Marfan syndrome is caused by a defect in the gene that encodes the structure of fibrillin and the elastic fibers, a major component of connective tissue. This gene is called fibrillin-1 or FBN1. In most cases, Marfan syndrome is inherited. The pattern is called “autosomal dominant,” meaning it occurs equally in men and women and can be inherited from just one parent with Marfan syndrome. People who have Marfan syndrome have a 50 percent chance of passing along the disorder to each of their children. In 25 percent of cases, a new gene defect occurs due to an unknown cause. Marfan syndrome is also referred to as a “variable expression” genetic disorder, because not everyone with Marfan syndrome has the same symptoms to the same degree. Marfan syndrome is present at birth. However, it may not be diagnosed until adolescence or young adulthood. Who is affected by Marfan syndrome? Marfan syndrome is fairly common, affecting 1 in 10,000 to 20,000 people. It has been found in people of all races and ethnic backgrounds. What are the signs of Marfan syndrome? Sometimes Marfan syndrome is so mild, few if any, symptoms occur. In most cases, the disease progresses with age and symptoms of Marfan syndrome become noticeable as changes occur in connective tissue. hysical Appearance: People with Marfan syndrome are often very tall and thin. Their arms, legs, fingers P and toes may seem out of proportion, too long for the rest of their body. Their spine may be curved and their breastbone (sternum) may either stick out or be indented. Their joints may be weak and easily become dislocated. Often, people with Marfan syndrome have a long, narrow face and the roof of the mouth may be higher than normal, causing the teeth to be crowded. Marfan syndrome causes many changes to occur within the body structures, including dental and skeletal (bone) problems. ental and bone problems: Patients with Marfan syndrome may have a dental history of tooth extractions or D palate expanders for a narrow palate. In addition, patients may have a history of bone problems such as flat feet, hernias and bone dislocations. sydell and arnold Miller family heart & vascular institute www.clevelandclinic.org/marfan For information: 866.289.6911 © 2000-2009 Cleveland Clinic. All rights reserved. Rev. 3/09 Signs of Marfan syndrome (continued) Other changes that occur with Marfan syndrome due to the abnormal connective tissue include changes in the eyes, heart and blood vessels, lungs and skin. Eye problems More than half of all people with Marfan syndrome have eye problems including nearsightedness (blurring of objects far away), lens subluxation (lens of the eye moves away from its typical position) or having a difference in the shape of the eye. dilated aorta Changes in the heart and blood vessels About 90 percent of people with Marfan syndrome develop changes in their heart and blood vessels. lood vessel changes: With Marfan syndrome, the walls of the B blood vessels become weak and dilate (stretch). These blood vessel changes often affect the aorta, the major artery that carries blood from the heart to the rest of the body. When the walls of the aorta weaken or stretch, there is an increased risk of aortic aneurysm, aortic dissection or rupture (bursting). All portions of the aorta can dilate or dissect. These conditions can result in a medical emergency and in some cases are life-threatening. (See next page for more information about these conditions). Normal mitral valve Leaflets close tightly to prevent backflow of blood when the ventricle contracts atients also may have a history of intracranial bleeding P or brain aneurysms, referred to as Berry aneurysms. eart valve problems: The heart’s valves, especially H the mitral valve, can be affected by Marfan syndrome. The valve leaflets become floppy and do not close tightly, allowing blood to leak backwards across the valve (mitral valve prolapse, also called MVP). When MVP progresses, the condition is called mitral valve regurgitation. itral valve prolapse and regurgitation are associated M with varying degrees of valve leakage. Mild valve leaks do not create extra work on the heart, but require routine follow-up. More significant valve leakages, as determined by your doctor, increase the workload on the heart and may cause symptoms of shortness of breath, feeling over-tired, or palpitations (fluttering in the chest). The abnormal flow may cause a heart murmur, which can be heard with a stethoscope. Over time, the heart may enlarge and heart failure may occur. 4 sydell and arnold Miller family heart & vascular institute www.clevelandclinic.org/marfan Mitral valve prolapse M itral valve leaflets are stretched and do not close tightly T he leaflets bow or flop back into the left atrium with each heartbeat T he valve may leak For information: 866.289.6911 © 2000-2009 The Cleveland Clinic Foundation. All rights reserved. Rev. 3/09 Changes in the heart and blood vessels (continued) ardiomyopathy: With Marfan syndrome, the C heart muscle may enlarge and weaken over time, causing cardiomyopathy. The condition may progress to heart failure. Aortic root dilation: The aortic root is the area where the aorta meets the aortic valve. With Marfan syndrome, the aortic root may dilate or widen. This can cause the aortic valve to become stretched and leak. rrhythmia (abnormal heart rhythm): May A occur in some patients with Marfan syndrome. Arrhythmia is often related to MVP. Other signs of Marfan syndrome ung changes: The changes in lung tissue that L occur with Marfan syndrome increase the risk of asthma, emphysema, bronchitis, pneumonia and collapsed lung. kin changes: Decreased elasticity of the skin S cause stretch marks to occur even without changes in weight. How is Marfan syndrome diagnosed? Marfan syndrome is based on a clinical diagnosis. A multidisciplinary approach is necessary to make the diagnosis because multiple organ systems must be assessed. Members of the team will assess the patient’s family history, eyes, heart and blood vessels, spine and skeletal system. A thorough history of symptoms and information about family members that may have had related problems are also necessary. Other tests, such as an echocardiogram (an imaging procedure that uses high frequency sound waves to produce a moving picture of the heart’s valves and chambers) will be used to evaluate changes in the heart and blood vessels, and to detect heart rhythm problems. If sections of the aorta can not be visualized through echocardiogram, or if a dissection is already suspected, a transesophageal echo (TEE), magnetic resonance imaging (MRI), or computed tomography (CT) scan may be needed. sydell and arnold Miller family heart & vascular institute www.clevelandclinic.org/marfan Often a CT or MRI may also be needed to evaluate for a condition called dural ectasia, a bulging of the lining of the spinal column. It often does not cause any symptoms but it can be associated with back pain in some patients. Dural ectasia is a feature that helps to support the diagnosis of Marfan syndrome but it can also occur with other connective tissue disorders. In some situations, a specific blood test can be used to help diagnose Marfan syndrome. This blood test is highly specialized and is used to detect changes in FBN1, the gene that is responsible for most cases of Marfan syndrome. Genetic counseling should accompany genetic testing because FBN1 testing is not always straightforward. Blood tests also can be used to help in the diagnosis of other genetic mutations, such as Loeys-Dietz syndrome, that cause physical findings similar to Marfan syndrome. Genetic Testing What is genetic testing? Genetic testing is a specialized laboratory test that looks for changes (also called mutations) in a person’s genetic material (DNA, genes or chromosomes) or in the products that the genes make. A gene contains instructions for our bodies. Genes are made up of chemical bases represented by the letters A, T, C and G. Every gene contains thousands of letters. Most times genetic testing is done by taking a blood sample, but sometimes other body samples (like cheek cells or skin) are needed. FBN1 testing is expensive (approximately $2,000). For information: 866.289.6911 © 2000-2009 The Cleveland Clinic Foundation. All rights reserved. Rev. 3/09 5 Genetic testing (continued) It is often covered by insurance, but this varies depending on individual insurance policies. We recommend that you check with your insurance company about coverage prior to having testing. FBN1 is a large gene and mutations can be found throughout the gene. Over 1,000 different mutations have been identified in FBN1; most mutations are unique to an individual family. Once a mutation is found in one family member, we expect that same mutation to be present in affected family members. In some cases, a change in the genetic code is found that the lab is not able to determine if it actually causes Marfan syndrome. These types of mutations are called variants. When variants are identified, sometimes it is necessary to test other family members (often parents) to try to determine its significance. The lab may also identify changes in the gene called polymorphisms. Polymorphisms are gene changes that are relatively common and are not likely to cause Marfan syndrome. Someone in whom a diagnosis is suspected but clinical evaluation did not establish the diagnosis. Someone in whom Marfan syndrome is one of several diagnoses that are being considered. Family members of someone with an identified mutation. Who should have genetic testing? How is Marfan syndrome treated? There are numerous reasons that someone should consider genetic testing for Marfan syndrome. People who should consider genetic testing include: Marfan syndrome requires a treatment plan that is individualized to the patient’s needs. Some people may not require any treatment, just regular follow-up appointments with their doctor. Others may need medications or surgery. The approach depends on the structures affected and the severity of the condition. 6 Someone with a clinical diagnosis who is interested in genetic testing so that other family members can get tested. Genetic testing should be initiated in someone with Marfan syndrome first and once a mutation is identified other family members can have testing for that mutation at a reduced cost. Someone with a clinical diagnosis who would like to confirm the diagnosis. (It should be noted that not all cases of Marfan syndrome can be confirmed through genetic testing. Therefore, when a person with a diagnosis of Marfan syndrome does not have a mutation in FBN1 it does not mean that he/she does not have Marfan syndrome. It just means that it was not possible to find the genetic reason with current technology. sydell and arnold Miller family heart & vascular institute www.clevelandclinic.org/marfan Lifestyle considerations Follow-up: Routine follow-up including cardiovascular, eye, and skeletal exams, especially during the growing years. Your doctors will discuss the frequency of follow-up with you. Activity: Activity guidelines vary, depending on the extent of the disease and symptoms. Most people with Marfan syndrome can participate in some type of physical and/or recreational activities. Those with dilation of the aorta will be asked to avoid high-intensity team sports, contact sports, and isometric exercises (such as weight lifting). Ask your cardiologist about activity guidelines for you. For information: 866.289.6911 © 2000-2009 The Cleveland Clinic Foundation. All rights reserved. Rev. 3/09 Lifestyle considerations (continued) Pregnancy: Genetic counseling should be performed prior to pregnancy as Marfan syndrome is an inherited condition. Pregnant women with Marfan syndrome are considered high risk cases. If the aorta is normal size, the risk for dissection is lower, but not absent. Those with even slight enlargement are at higher risk and the stress of pregnancy may cause more rapid dilation. Careful followup, with frequent blood pressure checks and monthly echocardiograms is required during pregnancy. If there is rapid enlargement or aortic regurgitation, bed rest or surgery may be required. Your doctor will discuss with you the best method of delivery with you. Endocarditis prevention: People with Marfan syndrome who have also had valve surgery have an increased risk for bacterial endocarditis. This is an infection of the heart valves or tissue which occurs when bacteria enters the blood stream. To reduce the risk of endocarditis, antibiotics should be given prior to dental or surgical procedures in patients with Marfan syndrome who have had valve surgery. Check with your doctor about the type and amount of antibiotics you should take. A wallet card may be obtained from the American Heart Association with specific antibiotic guidelines. Medications Medications are not used to treat Marfan syndrome, however they may be used to prevent or control complications. Medications may include: beta-blocker improves the heart’s ability A to relax, decreases the forcefulness of the heartbeat and the pressure within the arteries, thereby preventing or slowing the enlargement of the aorta. Beta-blocker therapy should begin at an early age. sydell and arnold Miller family heart & vascular institute www.clevelandclinic.org/marfan In people who are unable to take beta-blockers due to asthma or sideeffects, a calcium channel blocker, such as verapamil, is recommended. angiotensin An receptor blocker (ARB) is a type of medication that acts on a chemical pathway in the body. These agents are often used in treatment of high blood pressure as well as heart failure. Clinical trials are currently being conducted to evaluate how these medications may prevent aortic enlargement. Surgery Surgery for Marfan syndrome is aimed at preventing aortic dissection or rupture and treating valve problems. When the aorta diameter is more than 4.7 cm (centimeters) to 5.0 cm (depending on your height), or if the aorta is enlarging at a rapid pace, surgery is recommended. Your cardiologist may also calculate your aortic root diameter to height ratio, since this may also influence whether you should have surgery. The recommendation for surgery is based on size of the aorta, expected normal size of the aorta, rate of aortic growth, age, height, gender and family history of aortic dissection. Surgery involves a replacement of the dilated portion of the aorta with a graft. Valve repair or replacement surgery may be needed when Marfan syndrome causes a leaky aortic or mitral valve (regurgitation) that leads to changes in the left ventricle (left lower chamber of the heart) or heart failure. For information: 866.289.6911 © 2000-2009 The Cleveland Clinic Foundation. All rights reserved. Rev. 3/09 7 Surgical Treatment for Marfan Syndrome Surgery for Marfan syndrome is aimed at preventing aortic dissection or rupture (see next page for more information about these conditions) and treating valve problems. It is recommended that people with Marfan syndrome undergo surgery by surgeons who are experienced in this type of surgery. A better understanding of Marfan syndrome combined with earlier detection, careful follow-up and safer surgical techniques have resulted in better outcomes for patients. At the Cleveland Clinic, patients who had surgery for Marfan syndrome or related connective tissue disorders had a 99 percent survival rate and excellent normal expected late survival of 82 percent at 10 years. Aorta Surgery for Marfan Syndrome Surgery involves a replacement of the dilated portion of the aorta with a graft. The two surgical techniques include: raditional method: Replace the aorta T with a graft and the aortic valve with a mechanical valve. alve-sparing method: Replace the V aorta with a tube graft and re-implant the native aortic valve. The valvesparing method is the recommended surgery and is the standard of care. Your surgeon should be experienced in performing this complex procedure. Aortic aneurysm Repair of aortic aneurysm with graft Traditional aorta surgery method During surgery, the heart surgeon removes the area of dissection or aneurysm. Due to the connective tissue disorder, the aorta is prone to tearing, so the heart surgeon must use great care. A mechanical valve, attached to the end of the aortic graft, is sewn to the annulus (opening) of the aortic valve. The coronary arteries are reattached to the aortic graft through small button holes cut into the graft. Then, the other end of the Dacron graft is sewn to the tissue of the aorta. Mechanical Heart Valves Mechanical heart valves are made of metal or carbon and are designed to perform the functions of the patient’s native heart valve. A mechanical valve is Open very durable, well-tolerated by the body and is designed to last a lifetime. Closed The bi-leaflet valve is the most common type of mechanical valve and consists of two carbon leaflets in a ring covered with polyester knit fabric. Most patients who receive a mechanical valve replacement need to take anticoagulant medications for the rest of their lives. 8 sydell and arnold Miller family heart & vascular institute www.clevelandclinic.org/marfan For information: 866.289.6911 © 2000-2009 Cleveland Clinic. All rights reserved. Rev. 3/09 Aortic Dissection Aortic Aneurysm The aorta has many layers. Aortic dissection is a tear that develops in the inner layer of the aorta, causing blood to flow between the layers. The layers then separate, interrupting the blood flow and possibly causing the arterial wall to burst. An aortic aneurysm is an abnormal enlargement or bulging of the wall of the aorta. An aneurysm can occur anywhere in the vascular tree. Once an aneurysm is diagnosed, treatment may be needed, depending on the size of the aneurysm. Ruptured aneurysms require emergency surgery to stop the bleeding. normal aorta aneurysm In patients with Marfan syndrome, aortic dissection is a lifethreatening emergency that requires immediate treatment. Surgical treatment involves repairing or replacing the damaged segment of the aorta. The goal is to perform surgery BEFORE dissection occurs, to reduce the risk of death and to improve the long-term life expectancy. The majority of patients who have surgery prior to dissection do not need future surgeries. However, surgery after aortic dissection increases the need for future surgeries to repair other sections of the aorta. Symptoms of Aortic Dissection Symptoms of Aortic Aneurysm ymptoms of a thoracic aortic aneurysm S (affecting upper part of aorta in chest): Pain in the jaw, neck, upper back or chest; coughing, hoarseness or difficulty breathing ymptoms of an abdominal aortic aneurysm S (affecting lower part of aorta in abdomen): Pulsating enlargement or tender mass felt by a physician when performing a physical examination; pain in the back, abdomen, or groin not relieved with position change or pain medication Early diagnosis of an aneurysm is critical to managing the condition and reducing the risk of rupture. If you have these symptoms, call your doctor right away. ost common symptom: Severe pain in the M chest (front, back or both) Less common symptoms: Pain in the abdomen, numbness or weakness in one or both legs, loss of consciousness, or symptoms of a stroke (sudden weakness, numbness, dizziness or loss of balance; sudden vision changes; sudden confusion, difficulty speaking) If you have these symptoms, call for emergency help (dial 911 in most areas). For information: 866.289.6911 © 2000-2009 Cleveland Clinic. All rights reserved. Rev. 3/09 9 Valve sparing re-implantation aorta surgery There are two methods for replacing the aorta without replacing the aortic valve, including: Valve sparing re-implantation method Valve remodeling method Aortic arch repair surgery with repair and reimplantation of the native aortic valve The surgery involves freeing and repairing the aortic valve and replacing the damaged section of the aorta with a synthetic tube graft. graft Both surgical techniques are used for young people whose aortas are not too enlarged and in whom the aortic valve has not been damaged. After aortic graft surgery, patients usually remain in the hospital 5 to 10 days. After a recovery period of six to eight weeks, return to regular activities is expected. Sutures are placed through the graft and just below the aortic valve, around the left ventricular outflow tract. The valve sparing re-implantation method (illustrated to the right) is the preferred method for people with Marfan syndrome. Valve Repair or Replacement Surgery for Marfan Syndrome Valve repair or replacement surgery may be needed when Marfan syndrome causes a leaky aortic or mitral valve (regurgitation) that leads to changes in the left ventricle (left lower chamber of the heart) or heart failure. Over the past several years, there have been great advances in the surgical treatment of diseased heart valves, including the modified David’s reimplantation procedure. In this procedure, the appropriately sized aorta graft is determined, the left ventricular outflow tract (the passageway out of the left ventricle) is maintained, and surgical outcomes are improved when using the valvesparing method. For more information about this technique, please see our website at www.clevelandclinic.org/marfan. At Cleveland Clinic, valve surgery may be combined with other heart surgeries, such as more than one valve procedure, bypass surgery, aortic aneurysm surgery or surgery to treat atrial fibrillation (an irregular heart beat that is common in patients with valve disease). Your surgeon can provide more information about valve surgery if this treatment option is recommended. 10 sydell and arnold Miller family heart & vascular institute www.clevelandclinic.org/marfan dilator A custom-sized dilator device is placed in the left ventricular outflow tract, through the aortic valve. Sutures are tied around the dilator to shape the bottom portion of the aorta graft, similar to the natural aortic root. The repaired aortic valve is reimplanted and the aortic graft is sewn to the annulus of the repaired valve. The valve is tested to make sure it opens and closes properly. Small holes are made in the graft for the coronary ostia (openings), where the coronary arteries are re-attached. The graft is sewn to the aorta. If the aortic arch needs to be replaced, a separate graft is sewn from the aortic arch to the aortic root graft. For information: 866.289.6911 © 2000-2009 Cleveland Clinic. All rights reserved. Rev. 3/09 Follow-Up Care A better understanding of Marfan syndrome combined with earlier detection, careful follow-up and safer surgical techniques have resulted in better outcomes for patients. Even if you have surgery to treat your condition, it is important to follow up with your doctor regularly, take your medications as prescribed, and make preventive lifestyle changes to reduce the risk of future disease progression. Your health care team can help you achieve your goals. References Svensson LG, Blackstone EH, Feng J, de Oliveira D, Gillinov AM, Thamilarasan M, Grimm RA, Griffin B, Hammer D, Williams T, Gladish DH, Lytle BW. Are Marfan syndrome and marfanoid patients distinguishable on long-term followup? Ann Thorac Surg. 2007 Mar;83(3):1067-74. PMID: 17307461. hudia SK, Troughton R, Lam BK, Rajeswaran J, Mills WR, B Gillinov AM, Griffin BP, Blackstone EH, Lytle BW, Svensson LG. Mitral valve surgery in the adult Marfan syndrome patient. Ann Thorac Surg. 2006 Mar;81(3):843-8. PMID: 16488682. eur M, Costin B, Crowe S, Grimm RA, Moran R, H Svensson LG, Traboulsi EI.The value of keratometry and central corneal thickness measurements in the clinical diagnosis of Marfan syndrome. Am J Ophthalmol. 2008 Jun;145(6):997-1001. Epub 2008 Apr 18. Pearson GD, Devereux R, Loeys B, Maslen C, Milewicz D, Pyeritz R, Ramirez F, Rifkin D, Sakai L, Svensson L, Wessels A, Van Eyk J, Dietz HC; National Heart, Lung, and Blood Institute and National Marfan Foundation Working Group. Report of the National Heart, Lung, and Blood Institute and National Marfan Foundation Working Group on research in Marfan syndrome and related disorders. Circulation. 2008 Aug 12; 118(7):785-91. PMID: 18695204. vensson LG. Aortic valve stenosis and regurgitation: an S overview of management. J Cardiovasc Surg (Torino). 2008 Apr;49(2):297-303. PMID: 18431353. vensson LG, Kouchoukos NT, Miller DC, Bavaria JE, S Coselli JS, Curi MA, Eggebrecht H, Elefteriades JA, Erbel R, Gleason TG, Lytle BW, Mitchell RS, Nienaber CA, Roselli EE, Safi HJ, Shemin RJ, Sicard GA, Sundt TM 3rd, Szeto WY, Wheatley GH 3rd; Society of Thoracic Surgeons Endovascular Surgery Task Force. Expert consensus document on the treatment of descending thoracic aortic disease using endovascular stent-grafts. Ann Thorac Surg. 2008 Jan;85(1 Suppl):S1-41. PMID: 18083364. Svensson LG, Deglurkar I, Ung J, Pettersson G, Gillinov AM, D'Agostino RS, Lytle BW. Aortic valve repair and root preservation by remodeling, reimplantation, and tailoring: sydell and arnold Miller family heart & vascular institute www.clevelandclinic.org/marfan technical aspects and early outcome. J Card Surg. 2007 Nov-Dec;22(6):473-9. PMID: 18039206. Svensson LG. The elephant trunk procedure: uses in complex aortic diseases. Curr Opin Cardiol. 2005 Nov;20(6):491-5. Review. PMID: 16234619. Svensson LG, Kim KH, Blackstone EH, Alster JM, McCarthy PM, Greenberg RK, Sabik JF, D'Agostino RS, Lytle BW, Cosgrove DM. Elephant trunk procedure: newer indications and uses. Ann Thorac Surg. 2004 Jul;78(1):109-16; discussion 109-16. Review. PMID: 15223413. vensson LG. Sizing for modified David’s reimplantation S procedure. Ann Thorac Surg. 2003 Nov;76(5):1751-3. PMID: 14602338. vensson LG, Kim KH, Lytle BW, Cosgrove DM. Relationship S of aortic cross-sectional area to height ratio and the risk of aortic dissection in patients with bicuspid aortic valves. J Thorac Cardiovasc Surg. 2003 Sep;126(3):892-3. PMID: 14502185. vensson LG. Progress in ascending and aortic arch S surgery: minimally invasive surgery, blood conservation, and neurological deficit prevention. Ann Thorac Surg. 2002 Nov;74(5):S1786-8; Discussion S1792-9. PMID: 12440666. vensson LG, Khitin L. Aortic cross-sectional area/height S ratio timing of aortic surgery in asymptomatic patients with Marfan syndrome. J Thorac Cardiovasc Surg. 2002 Feb;123(2):360-1. PMID: 11828302. vensson LG, Longoria J, Kimmel WA, Nadolny E. S Management of aortic valve disease during aortic surgery. Ann Thorac Surg. 2000 Mar;69(3): 778-83; Discussion 783-4. PMID: 10750761. Svensson LG, Labib SB, Eisenhauer AC, Butterly JR. Intimal tear without hematoma: an important variant of aortic dissection that can elude current imaging techniques. Circulation. 1999 Mar 16;99(10):1331-6. PMID: 10077517. For information: 866.289.6911 © 2000-2009 Cleveland Clinic. All rights reserved. Rev. 3/09 11 Support is Available We understand that learning you have a genetic disorder, such as Marfan syndrome, is concerning. You may be worried about making lifestyle changes, financial concerns, having surgery, needing to have medical follow-up care the rest of your life. Or there may be financial concerns. It may be also concerning to think about risk to future children. It is important to seek medical care from a physician who has experience in treating Marfan syndrome. Get accurate information. It may also help to seek genetic counseling to help understand the disease and your risk for passing it on to your children. In addition to the Marfan syndrome resources at Cleveland Clinic (listed below), these national organizations can help provide you with information and support: National Marfan Foundation www.marfan.org 800.862.7326 National Institute of Arthritis and Musculoskeletal and Skin Disease www.niams.nih.gov 877.226.4267 American Heart Association www.americanheart.org 800.242.8721 Marfan Syndrome and Connective Tissue Disorder Clinic The multi-disciplinary team of experts in the Marfan Syndrome and Connective Tissue Disorder Clinic includes cardiologists, pediatric cardiologists, cardiovascular and vascular surgeons, ophthalmologists, orthopedic surgeons and genetic specialists. The mission of the Marfan Syndrome and Connective Tissue Disorder Clinic is to bring together a knowledgeable and experienced multi-disciplinary team of cardiology and vascular doctors and other cardiology experts to provide: A thorough evaluation of patients using state-of-the art diagnostic testing On-going comprehensive care for those patients with disease of the aorta, connective tissue disorder, and Marfan syndrome Genetic screening for families of those with genetic disorders, such as Marfan syndrome Ongoing research and education to provide patients with high quality and innovative therapies The goal is to help patients live longer and improve their quality of life. For More Information For more information about Marfan syndrome and treatments, please visit our website at www.clevelandclinic.org/marfan or e-mail us using the Contact Us form on the web at www.clevelandclinic.org/heart. To talk with a nurse about Marfan syndrome and available treatment options, please contact the Heart and Vascular Resource Center Nurse toll-free at 866.289.6911. To make an appointment, please call 800.659.7822. About the Sydell and Arnold Miller Family Heart & Vascular Institute The Sydell and Arnold Miller Family Heart & Vascular Institute at Cleveland Clinic is one of the largest cardiovascular specialty groups in the world, providing patients with expert medical management and a full range of therapies. Our cardiac care program has been ranked number one since 1995 by U.S. News & World Report. Our areas of expertise combine research, education and clinical practice to provide innovative and scientificallybased treatments for cardiovascular disease. The commitment of our physicians and scientists to the prevention and cure of cardiovascular disease has led to innovative care, better outcomes and improved quality of life for patients with cardiovascular disease. This information is not intended to replace the medical advice of your doctor or health care provider. Please consult your health care provider for advice about a specific medical condition. 12 sydell and arnold Miller family heart & vascular institute www.clevelandclinic.org/marfan For information: 866.289.6911 © 2000-2009 Cleveland Clinic. All rights reserved. Rev. 3/09