* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Neurologic
Survey
Document related concepts
Transcript
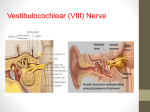
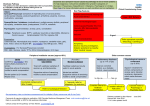
CM 4- Dizziness Dizziness Broad based term to explain how a person feels when our sense of balance is off. • Swimmyheadedness (better term) • True vertigo (feeling of spinning or turning) Multi-system evaluation • Vestibular (peripheral) • CNS (cerebellum) • Cardiac • Pulmonary • Endocrine (thyroid) • Musculoskeletal (C-spine) • Psychogenic (anxiety) Vertigo Diagnosis is made by • History: feel like they are turning • Physical exam: BP, ENT otoscopic, neurologic, cardiac, psych, nystagmus when dizzy • Dix-Hallpike maneuver • Labs: TSH • Audiometry if hearing loss suspected • Imaging if mass suspected (MRI contrast) Peripheral vs Central Vertigo • Peripheral ( Labyrinth or vestibular nerve) – latency 2 - 40 seconds after stimulus – intensity severe – lasts under 1 minute – resolves with continued head position (fatigability) – attenuates with repeated stimulus (habituation) – can have hearing loss &/or tinnitus – no additional neurologic findings • Central (brainstem or cerebellum) – no latency – intensity milder – lasts more than 1 minute – does not fatigue – no habituation – no hearing loss – additional neurologic symptoms found • • • • Nystagmus Feeling of turning in direction of “fast beat” eye movement Nausea (vomiting) Inability to walk due to loss of balance Blurry vision from eye jerking CM 4- Dizziness • • • • • • • • • • • • • Common Causes of Dizziness Benign Positional Vertigo – spells last seconds, results from tiny particles (otoconia) that fall into the wrong part of the semicircular canals, occurs predictably with certain head position, no auditory symptoms, peripheral, 50% vertigo in elderly (20% overall) Ménière’s Disease – spells last hours, believed to be caused by an excess of fluid in the inner ear, tinnitus and low pitch hearing loss, peripheral Vestibular Neuronitis – lasts days, results from viral damage to VIII cranial nerve (no real inflammation), caused by imbalance in neuronal input, no hearing symptoms, peripheral Labyrinthitis – lasts days, results from viral or bacterial infection involving the ears with involvement of the cochlea or semicircular canals (labyrinth), hearing loss and tinnitus occur, peripheral Less Common Causes of Dizziness perilymphatic fistulae from trauma – spells seconds, hearing Sx, peripheral vascular ischemia: TIA, stroke – spells seconds, no hearing Sx, central or peripheral syphilis – spells hours, hearing Sx, peripheral migraine aura – spells hours, no hearing Sx, central anxiety – spells vary, no hearing Sx acoustic neuroma: VIII nerve – spells months, hearing Sx, peripheral cerebellar degeneration, tumor, or damage – spells months, no hearing Sx, central multiple sclerosis – spells months, no hearing Sx, central vestibular ototoxicity: aminoglycosides – spells months, hearing Sx, peripheral Dix-Hallpike Maneuver (diagnose positional vertigo) 1. With the patient sitting on the examination table, facing forward, eyes open, the physician turns the patient's head 45 degrees to the right (A). 2. The physician supports the patient's head as the patient lies back quickly from a sitting to supine position, ending with the head hanging 20 degrees off the end of the examination table. 3. The patient remains in this position for 30 seconds (B). 4. Then the patient returns to the upright position and is observed for 30 seconds. 5. The maneuver is repeated with the patient's head turned to the left. 6. A positive test is indicated if any of these maneuvers produce vertigo with or without nystagmus. • • • • • • • • • Vertigo Treatment Meclizine – antagonist of central and peripheral H1 receptors – antagonizes cholinergic receptors for antiemetic effect. – causes sedation and confusion in the elderly Vestibular rehabilitation exercises: habituation Benign Positional Vertigo - canalith repositioning: Epley Maneuver Vestibular neuronitis and Labyrinthitis - meds and vestibular exercises: self limited in 6 weeks Ménière’s - diuretics, surgery Vascular Ischemia - treat hypertension, platelet inhibition (baby aspirin) Migraine - meds, vestibular rehab Psychiatric - treat underlying disorder Physiologic (motion sickness) - scopolamine CM 4- Dizziness • • Epley Maneuver (for Benign Positional Vertigo) Patient in an upright sitting posture, legs fully extended, and head rotated 45° towards the affected side. The patient is then quickly and passively forced down backwards by the clinician to a supine position with the head held in a 20° - 30° neck extension (Dix-Hallpike position) where the affected ear faces the ground. The patient remains in this position for approximately 1 - 2 minutes and watched for nystagmus. The head is then turned 90° to the opposite direction so that the unaffected ear faces the ground, all while maintaining the 30° neck extension. The patient remains in this position for approximately 1 - 2 minutes. Keeping the head and neck in a fixed position relative to the body, the individual rolls onto their shoulder, rotating the head another 90° in the direction that they are facing. The patient is now looking downwards at a 45° angle. The patient remains in this position for approximately 1–2 minutes and is watched for nystagmus. Finally, the patient is slowly brought up to an upright sitting posture on the edge of the table they are facing, while maintaining the 45° rotation of the head. The patient sits in this position for up to 30 seconds. The procedure may be repeated on either side until the patient experiences relief of symptoms. • • • • Tinnitus Auditory perception – a ringing, hissing, buzzing, roaring, clicking in one or both ears Affects 10% of US population Prevalent in 40-70 year olds Usually benign • • • • • • • • In general pulsatile tinnitus, unilateral tinnitus, and tinnitus associated with other otologic symptoms represent potentially more serious underlying disease than bilateral tinnitus. Consider an MRI if tumor or serious vascular lesion is suspected in the CNS. CM 4- Dizziness • Otologic disorders are the most common cause of tinnitus and are associated with hearing loss • Hearing loss Conductive – inhibition of sound transmission to inner ear: cerumen, middle ear fluid, otosclerosis, swelling of external canal, TM perforation Sensorineural - abnormality of inner ear or cochlear portion of eight cranial nerve: noise induced hearing loss, presbycusis (advancing age) Tinnitus with Meniere’s • An excessive accumulation of endolymph in the membranous labyrinth is a diagnosis of exclusion. • Characterized by one or more symptoms of recurrent vertigo, unilateral aural fullness, tinnitus and hearing loss Ototoxic Drugs • risks are advanced age or very young, renal and hepatic impairment, pregnancy Medications • Analgesics - ASA, NSAIDS • Antibiotics - aminoglycosides, erythromycin, tetracycline • Chemotherapeutics – bleomycin, cisplatin • Loop diuretics – edecrin, furosemide, bumetanide Medical History and Tinnitus • Onset – progressive with advancing (presbycusis); precipitous onset, linked with loud noise and/or head trauma • Location – unilateral (cerumen impaction, otitis externa or media) tinnitus and unilateral hearing loss suggest acoustic neuroma • Pattern – continuous - hearing loss episodic - Ménière’s pulsatile - vascular origin (aneurysms, AV fistulae) • Pitch - low (Ménière’s) high (sensorineural hearing loss) • Ototoxic exposure • Alleviating - patulous eustachian tube alleviated by lying down Physical Exam • • • • • External canal and TM Cranial nerves Auscultation of neck, periauricular, orbits, mastoid Weber • sound lateralizes to same side with conductive hearing loss and opposite side with sensorineural loss, • sound at same level in both ears is normal hearing or equal bilateral hearing loss Rinne test • bone conduction > air :conductive loss ; • air conduction > bone : normal or sensorineural loss CM 4- Dizziness Case Chief Complaint: Dizziness Mrs. White is a 67 yo retired psychologist who complains of a sensation of room spinning for the past 4-5 days. She denies any trauma, head injury, syncopal episode, chest pain, or new medications. She states the episodes last approximately 30 seconds to two minutes in duration during which time she feels nauseated. What is your working differential diagnosis at this time? List all potential causes. Peripheral Causes • Acute labyrinthitis Infection of the labyrinth, viral or bacterial • Acute vestibular neuronitis Infection of the vestibular nerve, viral • Benign positional vertigo Transient episodes of vertigo caused by stimulation of vestibular sense organs by canaliths; affects older patients and women more • Cholesteatoma Lesion filled with keratin debris, involving the middle ear and mastoid • Herpes zoster oticus Vesicular eruption affecting the ear; caused by reactivation of the Varicella zoster virus, shingles • Ménière’s disease (endolymphatic hydrops) Recurrent episodes of vertigo, hearing loss, tinnitus, or aural fullness caused by increased volume of endolymph in the semicircular canals • Otosclerosis Hardening or thickening of the tympanic membrane from age or recurrent infection • Perilymphatic fistula Breach between middle and inner ear often caused by trauma or excessive straining Central Causes • Cerebellopontine angle tumor Vestibular schwannoma or acoustic neuroma, also infratentorial ependymoma, brainstem glioma, medulloblastoma, or neurofibromatosis • Cerebrovascular disease Transient ischemic attacks or stroke. Arterial occlusion causing cerebral ischemia or infarction, especially affecting the vertebrobasilar system • Migraine Episodic headaches Usually unilateral, with throbbing accompanied by other symptoms such as nausea, vomiting, photophobia, or phonophobia; vertigo part of the aura • Multiple sclerosis Demyelinization of white matter in the central nervous system Other causes • Cervical vertigo Vertigo triggered by somatosensory input from head and neck movements, questionable diagnosis • Drug-induced vertigo Adverse reaction to medications, psychiatric conditions, anxiety, or somatization DDx: Peripheral Vs Central Inner ear disease (peripheral): • Sudden onset of vertigo episodes • Hearing loss, ear pressure, or tinnitus • Lasts for seconds and is associated with position changes (suggests benign positional vertigo) • Vertigo that lasts for hours or days is probably caused by Ménière’s disease or vestibular neuronitis • Prior viral illness, cold sores, or sensory changes in the cervical C2-C3 or trigeminal distributions usually indicate vestibular neuronitis or recurrent episodes of Ménière’s disease. • Patients with peripheral vertigo are usually able to ambulate during attacks and are consciously aware of their environment. CM 4- Dizziness Central “CNS” Disease: • Gradual and ill-defined symptoms are more common in CNS, cardiac, and systemic diseases. • Vertigo of sudden onset that lasts for minutes can be due to vascular disease • Central vertigo secondary to brainstem ischemia is often associated with other brainstem characteristics, including diplopia, autonomic symptoms, nausea, dysarthria, dysphagia, or focal weakness • Dysdiadochokinesis and gait ataxia during episodes are more likely due to cerebellar diseases • Sensory and motor symptoms and signs are usually associated with CNS diseases • Common causes of central dizziness are migraine syndromes. Other central causes include demyelination, acoustic tumors, or cerebellar lesions. Mrs. White states she has had no headaches, vision changes, hearing loss, or tinnitus. She denies any recent illness but now seems to think the episodes occur with changes in head position. She has had no spontaneous episodes. Medical History: • PMHX She has no hx of Diabetes, hypertension, or CAD., menopause at age 52 • PSHX cholecystectomy age 47 • FAMHX There is no family hx of migraines or head and neck cancer. She is a retired psychologist. • Father deceased at age 84 of MI • Mother decease at age 82 pneumonia • Brother alive age 64 - hyptn • Sister alive age 65 - obese • MEDS She again states she takes no medications other than OTC vitamin D and calcium. • SOCHX married , social ETOH < 2x/month, non smoker, • WORKHX psychologist, retired Physical Examination • Ht 62" wt 140 lbs BP 124/81 P 76 reg R 16 • HEENT atraumatic, normocephalic, TM’s clear without effusion or exudate, external ear canal clear • PERRLA, EOMI, no nystagmus fundoscopic exam reveals sharp disc margins and no vessel nicking • Carotid pulses are strong, equal and no bruits • Cranial Nerves no palsies, weakness or sensorineural hearing loss is noted • Cardiac regular rate and rhythm without rubs , clicks or murmurs. • Gait is normal, mental status appears normal • You perform a Dix-Hallpike maneuver and note the patient develops torsional upbeat and horizontal nystagmus. Could you refine your diagnosis at this time? List your most probable cause. Benign Positional Vertigo • • • • • • • • Diagnosing Vertigo Patient complains of dizziness. Is it true vertigo? If No, work-up for lightheadedness, presyncope, or dysequilibrium. If Yes, consider medication side effects first. Stop any causing dizziness. Obtain history: timing and duration, provoking and aggravating factors, associated symptoms, and risk factors for cerebrovascular disease. Perform physical examination with special attention to head and neck, cardiovascular, neurologic systems, and provocative diagnostic tests such as Dix-Hallpike Refine differential diagnosis. Which conditions are consistent with physical examination findings? Consider brain MRI in patients with focal neurologic findings, risk factors for cerebrovascular disease, or other findings of a central cause of vertigo. Consider other laboratory and radiologic studies as indicated (e.g., cervical spine series in patients with findings suggesting cervical vertigo). CM 4- Dizziness • You decide to treat the patient with physical therapy (Epley maneuver) and modified home Epley maneuver. This patient does not have: severe carotid stenosis, unstable heart disease, cervical spondylosis, or advanced rheumatoid arthritis which are contraindications to treatment. • Older patients are at risk for sedation, falls, and urinary retention with use of drugs like meclizine. Now that you have made your diagnosis what signs and symptoms would prompt you to order laboratory or imaging studies? With the current diagnosis no labs or imaging studies are needed. Consider labs if a an underlying illness is suspected. Consider imaging if • neurologic symptoms and signs are present, • the patient has risks for CVA, • there is progressive unilateral hearing loss. Associated progressive hearing loss is not present in this case but can help refine your diagnosis. Name causes of vertigo associated with hearing loss. • Ménière’s disease • perilymphatic fistula • acoustic neuroma • cholesteatoma • otosclerosis • TIA or stroke involving anterior inferior cerebellar artery • herpes zoster oticus Your patient returns three weeks later and has noticed improvement of symptoms with physical therapy. She denies any headaches, hearing loss, or tinnitus. What are the characteristics of peripheral vs central vertigo ? Peripheral vs. Central vertigo Nystagmus • Peripheral - Combined horizontal and torsional; inhibited by fixation of eyes onto object; fades after a few days; does not change direction with gaze to either side • Central - Purely vertical, horizontal, or torsional; not inhibited by fixation of eyes onto object; lasts weeks to months; may change direction with gaze in fast beat direction Imbalance Peripheral- Mild to moderate; able to walk Central-Severe; unable to stand still or walk Nausea Peripheral - vomiting May be severe Central – Varies Hearing loss, tinnitus Peripheral – Common Central - Rare Nonauditory neurologic symptoms Peripheral – rare Central - common Latency after provocative diagnostic test Peripheral - Longer (up to 20 sec) Central - Shorter (up to 5 sec) Specialty referral when diagnosis is unclear, if diagnosis is in doubt or indicated by findings. Medical diagnosis may require specialty input.