* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Document
Survey
Document related concepts
Transcript
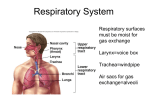
Pamela BL The lower respiratory tract consists of the larynx, trachea, bronchi and lungs. It begins to form during the fourth week(2627 days). The respiratory primordium is first indicated by a median outgrowth(the laryngotracheal groove)from the caudal end of the ventral wall of the primitive pharynx, caudal to the fourth pair of pharyngeal pouches. A.Diagramatic sagittal section of the cranial half of an embryo about 26 days illustrating the floor of the primitive pharynx and the location of laryngotracheal groove. B. Horizontal section at the level shown in A The endoderm lining the laryngotracheal groove gives rise to the epithelium and glands of the larynx, trachea, bronchi, and the pulmonary epithelium. The connective tissue, cartilage and smooth muscle in these structures develop from the splanchnic mesenchyme surrounding the foregut. By the end of the fourth week, the laryngotracheal groove has evaginated to form a pouch like laryngotracheal diverticulum, which is located ventral to the caudal part of the foregut. As this diverticulum elongates, it is invested with splanchnic mesenchyme, and its distal end enlarges to form a globular lung bud. Lateral view of the caudal part of the primitive pharynx illustrating partitioning of the foregut into esophagus and laryngotracheal tube4th-5th week Lateral view of the caudal part of the primitive pharynx illustrating partitioning of the foregut into esophagus and laryngotracheal tube4th-5th week The laryngotracheal diverticulum soon becomes separated from the primitive pharynx. Longitudinal tracheoesophageal folds(ridges) develop, approach each other and fuse to form a partition known as the tracheoesophageal septum. Transverse sections illustrating formation of the tracheoesophageal septum and separation of the foregut into the laryngotracheal tube and esophagus This septum divides the cranial part of the foregut into a ventral portion, the laryngotracheal tube(primordium of the larynx, trachea, bronchi and lungs), and a dorsal portion(primordium of the oropharynx and esophagus). The opening of the laryngotracheal tube into the pharynx becomes the laryngeal aditus(orifice) or inlet of the larynx. Lateral view of the caudal part of the primitive pharynx illustrating partitioning of the foregut into esophagus and laryngotracheal tube4th-5th week The epithelium of the internal lining of the larynx develops from the endoderm of the cranial end of the laryngotracheal tube. The cartilages of the larynx are derived from the cartilages in the 4th and 6th pairs of the branchial or pharyngeal arches. The mesenchyme at the cranial end of the laryngotracheal tube proliferates rapidly producing paired arytenoid swellings. These swellings grow towards the tongue, converting the slit like aperture called the primitive glossitis into a T shaped laryngeal aditus(inlet) and reducing the developing laryngeal lumen to a narrow slit. Drawings illustrating stages in development of the larynx. A.4 weeks, B.5 weeks. The epithelium of the internal lining of the larynx is of endodermal origin. Cartilages and muscles of the larynx arise from mesenchyme in the 4th and 6th pairs of branchial/pharyngeal arches. The laryngeal epithelium proliferates rapidly, resulting in a temporary occlusion of the laryngeal lumen during the 8th week. Recanalization of the larynx usually occurs by the 10th week. The laryngeal ventricles form during this process. These lateral recesses are bounded by folds of mucous membrane that become the vocal folds(cords) and vestibular folds. The epiglottis develops from the caudal part of the hypobranchial eminence, a prominence produced by proliferation of mesenchyme in the ventral ends of the 3rd and 4th branchial/pharyngeal arches. The rostral part of this eminence forms the pharyngeal part of the tongue. C. 6 weeks, D.10 weeks. Note that the laryngeal inlet or aditus changes in shape from slit like opening to a T shaped inlet as the mesenchyme proliferates. Because the laryngeal muscles develop from myoblasts in the 4th and 6th pairs of branchial/pharyngeal arches they are innervated by the laryngeal branches of the vagus nerves that supply these arches. Laryngeal web-uncommon anomaly that results from incomplete recanalization of the larynx during the 10th week. A membranous web forms at the level of the vocal folds(cords) partially obstructing the airway. The endodermal lining of the laryngotracheal tube distal to the larynx differentiates into the epithelium and glands of the trachea and to the pulmonary epithelium. The cartilage, connective tissue and muscles are derived from splanchnic mesenchyme surrounding the laryngotracheal tube. Drawings of transverse sections through the laryngotracheal tube illustrating progressive stages in the development of the trachea. A,4 weeks B,10 weeks C,11 weeks. Tracheosophageal fistula, an abnormal communication or fistula between the trachea and esophagus occurs about once in every 2500 births, most affected infants are males. In more than 85% of cases, a fistula is associated with esophageal atresia(Herbst, 1992). Tracheoesophageal fistula is the most common anomaly of the lower respiratory tract. It results from incomplete division of the cranial part of the foregut into respiratory and digestive portions during the 4th week. Incomplete fusion of the tracheoesophageal folds produces a defective tracheoesophageal septum and abnormal communication between the trachea and esophagus. Four varieties of tracheoesophageal fistula may develop. The most common abnormality is for the superior portion of the esophagus to end blindly(esophageal atresia) and for the inferior portion to join the trachea near its bifurcation. Infants with the common type of esophageal atresia and tracheoesophageal fistula cough and choke on swallowing due to accumulation of excessive amount of saliva in the mouth and upper respiratory tract. When the infant swallows, it rapidly fills the esophageal pouch and is regurgitated. Gastric contents may also reflux from the stomach through the fistula into the trachea and lungs. This causes choking and may result in pneumonia or pneumonitis(inflammation of the lungs). An excess of amniotic fluid(polyhydramnions)is often associated with esophageal atresia and tracheoesophageal fistula. This condition develops because amniotic fluid cannot pass to the stomach and intestines for absorption and subsequent transfer via the placenta to the mother’s blood for disposal. Tracheal stenosis and atresianarrowing(stenosis) and obstruction(atresia) of the trachea are uncommon anomalies that are usually associated with one of the varieties of the tracheoesophageal fistula. Stenoses and atresias probably result from unequal partitioning of the foregut into the esophagus and the trachea. Sometimes there is a web of tissue obstructing airflow(incomplete tracheal atresia). The bulb shaped lung that develops at the caudal end of the laryngotracheal tube during the 4th week divides into 2 knob like buds. These endodermal buds grow laterally into the pericardioperitoneal canals, the primordia of the pleural cavities. Together with the surrounding splanchnic mesenchyme, the bronchial buds differentiate into the bronchi and their ramifications in the lungs. Development of the lungs at four weeks Growth of developing lungs into the adjacent splanchnic mesenchyme of the medial walls of the pericardioperitoneal canals, five weeks. Early in the 5th week each bronchial bud enlarges to form the primordium of a main/primary bronchus. The embryonic right bronchus is slightly larger than the left one and is oriented more vertically, this embryonic relationship persists after birth. Consequently, a foreign body is more liable to enter the right main bronchus than the left one(Moore,1992). Development of the bronchi at five weeks The main/primary bronchi subdivide into secondary bronchi. On the right, the superior secondary bronchus will supply the superior lobe of the lung whereas the inferior secondary bronchus subdivides into two bronchi, one to the middle lobe of the right lung and the other to the inferior lobe. On the left, the two secondary bronchi supply the superior and inferior lobes of the lung. Development of the bronchi, six weeks Each secondary bronchus subsequently undergoes progressive branching. Tertiary or segmental bronchi, ten in the right lung and eight/nine in left lung, begin to form by the 7th week. As this occurs, the surrounding mesenchymal tissue also divides. Development of segmental/tertiary bronchi at eight weeks Each segmental bronchus with its surrounding mass of mesenchyme, is the primordium of a bronchopulmonary segment. By 24 weeks, about 17 orders of branches have developed. An additional seven orders of airways develop after birth. As the bronchi develop, cartilaginous plates develop from the surrounding splanchnic mesenchyme. The bronchial smooth musculature and connective tissue, pulmonary connective tissue and capillaries are also derived from this mesenchyme. As the lungs develop they acquire a layer of visceral pleura from the splanchnic mesenchyme. Development of the layers of the pleura, six weeks. With expansion, the lungs and the pleural cavities grow caudally into the mesenchyme of the body wall and soon lie close to the heart. The thoracic body wall becomes lined by a layer of parietal pleura derived from somatic mesoderm. Lung development can be divided into four stages: 1. Pseudoglandular period 2. Canalicular period 3. Terminal sac period 4. Alveolar period The pseudoglandular period(5-17 weeks); the developing lung somewhat resembles an exocrine gland during this period. By 17 wweeks all major elements of the lung have formed except those involved with gas exchange. Respiration is not possible, hence fetuses born during this period cannot survive. The canalicular period(16-25 weeks); this period overlaps the pseudoglandular period because cranial segments of the lungs mature faster than caudal ones. During the canalicular period, the Lumina of the bronchi and terminal bronchioles become larger and the lung tissue becomes highly vascular. By 24 weeks, each terminal bronchiole has divided to form two or more respiratory bronchiole. Each of these then divides into 3-6 tubular passages called alveolar ducts. Diagrammatic sketch of histological section illustrating late canalicular period , about 24 weeks. Respiration is possible toward the end of canalicular period because some thin walled terminal sacs(primitive alveoli) have developed at the ends of the respiratory bronchioles, and these regions are well vascular zed. Although a fetus born toward the end of this period may survive if given intensive care, it often dies because its respiratory and other systems are still relatively immature. The terminal sac period(24 weeks –birth); during this period many more terminal sacs develop and their epithelium becomes very thin. Capillaries begin to bulge into these primitive alveoli. By 24 weeks, the terminal sacs are lined mainly by squamous epithelial cells of endodermal origin known as type I alveolar cells/pneumocytes. The capillary network proliferates rapidly in the mesenchyme around the developing alveoli, and there is concurrent active development of lymphatic capillaries. Scattered among the squamous epithelial cells are rounded, secretory, epithelial cells called type II alveolar cells/pneumocytes. Diagrammatic sketch of histological section illustrating terminal sac period about 26 weeks These cells secrete pulmonary surfactant, a complex mixture of phospholipids which forms as a monomolecular film over the internal walls of the terminal sacs. It is recognized that the maturation of alveolar type II cells and surfactant production varies widely in fetuses of different gestational ages(Chernick and Kryger,1990). The production of surfactant increases during the terminal stages of pregnancy, particularly during the last two weeks before a full term birth. Surfactant counteracts surface tension forces and facilitates expansion of the terminal sacs(primitive alveoli). Consequently, fetuses born prematurely at 24-26 weeks may survive if given intensive care but they suffer respiratory distress due to surfactant defiency. Surfactant production begins by 20 weeks but it is present in very small amounts in premature infants, it does not reach adequate levels until the late fetal period(Ballard, 1989). By 26-28 weeks after fertilization, the fetus usually weighs about 1000gms and sufficient terminal sacs and surfactant are present to permit survival of a prematurely born infant. Before this, the lungs are usually incapable of providing adequate gas exchange, partly because the alveolar surface area is insufficient and the vascularity underdeveloped. It is not the presence of thin terminal sacs or primitive alveolar epithelium so much as the development of an adequate pulmonary vasculature and sufficient surfactant that are critical to the survival of premature infants. The alveolar period(late fetal period – childhood); the epithelial lining of the terminal sacs attentuates to an extremely thin squamous epithelial layer. The type I alveolar cells become so thin that the adjacent capillaries bulge into the terminal sacs. Diagrammatic sketch of histological section illustrating alveolar period in new born infant. By the late fetal period, the lungs are capable of respiration because the alveolocapillary membrane(respiratory membrane) is sufficiently thin to allow gas exchange. Although the lungs do not begin to perform this vital function until birth, they must be well developed so that they are capable of functioning as soon as the baby is born. At the beginning of the alveolar period, each respiratory bronchiole terminates in a cluster of thin walled terminal sacs separated from one another by loose connective tissue. These terminal sacs represent future alveolar ducts. Characteristic mature alveoli do not form until after birth. Before birth the immature alveoli appear as small bulges on the walls of respiratory bronchioles and terminal sacs(future alveolar ducts). After birth the primitive alveoli enlarge as the lungs expand, but most increase in the size of the lungs results from an increase in number of respiratory bronchioles and primitive alveoli rather than from an increase in the size of the alveoli(Crelin, 1975). From the 3rd-8th year or so, the number of immature alveoli continues to increase(Thurlbeck, 1991). Unlike mature alveoli immature alveoli have the potential for forming additional primitive alveoli. As primitive alveoli increase in size, they become mature alveoli. Breathing movements occur before birth, exerting sufficient force to cause aspiration of amniotic fluid into the lungs. These prenatal breathing movements, which can be detected by real time ultrasonography, are not continuous but they are essential for normal fetal lung development. The pattern of fetal breathing movements is widely used in the diagnosis of labor and as a predictor of fetal outcome in preterm delivery. Fetal breathing movements, which increase as the time of delivery approaches, probably condition the respiratory muscles. In addition, these movements stimulate lung development, possibly by creating a pressure gradient between the lungs and the amniotic fluid(Behrman, 1992). At birth the lungs are about half filled with fluid derived from the amniotic cavity, lungs and tracheal glands. Aeration of the lungs at birth is not so much the inflation of empty collapsed organs but rather the rapid replacement of intra alveolar fluid by air. The fluid in the lungs is cleared at birth by three routes: Through the mouth and nose by pressure on the thorax during delivery Into the pulmonary capillaries and into the lymphatics and pulmonary arteries and veins. Respiratory distress syndrome, infants born prematurely are susceptible to RDS(Chernick and Kryger, 1990). These infants develop rapid, labored breathing shortly after birth. Hyaline membrane disease is a major cause of RDS in newborn infants(Behrman, 1992).