* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download A multiparameter test of clot formation and fibrinolysis for in
Neuropharmacology wikipedia , lookup
Discovery and development of cyclooxygenase 2 inhibitors wikipedia , lookup
Drug design wikipedia , lookup
Theralizumab wikipedia , lookup
Plateau principle wikipedia , lookup
Drug interaction wikipedia , lookup
Drug discovery wikipedia , lookup
Discovery and development of direct Xa inhibitors wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Discovery and development of direct thrombin inhibitors wikipedia , lookup
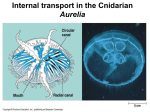
Original article 611 A multiparameter test of clot formation and fibrinolysis for in-vitro drug screening Barbara Kostkaa, Jadwiga Paraa and Joanna Sikorab A large spectrum of methods has been used in both routine and scientific studies of the hemostatic system. The particular interest of the investigators has been focused on methods simultaneously evaluating clotting and fibrinolysis processes. The aim of the present study was to develop an optical method for overall evaluation of clot formation and lysis (CL-test) that could be used in drug screening. The CL-test was performed in citrate plasma diluted with Tris-buffered saline. Thrombin was applied for plasma clotting (0.5 IU/ml), while tissue plasminogen activator (60 ng/ml) was used for fibrinolysis activation. Clot formation and lysis were monitored in thermostatic conditions (37-C) as a continuous record of transmittance change. By means of own computer program, kinetic parameters of the processes studied and plasma overall clot formation and fibrinolysis potential, expressed as the area under the clotgeneration and fibrinolysis curves, were calculated. The CL-test was developed and checked by evaluation of the effect, on clot formation and lysis, of various Introduction Fibrin formation and degradation are the final steps in blood coagulation and they involve sequential activation of multiple proenzymes circulating in the blood. The hemostatic balance between these processes is regulated by numerous mechanisms that control fibrin formation (most important factors are antithrombin, the protein C/protein S system, and tissue factor pathway inhibitor) and its degradation (the activities of plasmin and plasminogen activators are regulated by serpins and a2-macroglobulin). Defects in the mechanisms responsible for fibrin turnover might lead to thrombosis or bleeding. Many studies have shown that the hemostatic balance depends on physical, biochemical, and genetic factors. Numerous chemical compounds and drugs also have a profound influence on fibrin structure and clot formation and lysis [1]. A large spectrum of laboratory tests exists to identify this imbalance in the hemostatic system. In recent years, growing interest in a global assay of coagulation and fibrinolysis that uses optical measurements of clot formation and lysis has been observed [2]. As early as in 1975, Glover and Warner [3] used an aggregometer for turbidimetric measure of clot formation and fibrinolysis dynamics. They determined that curve segments, such as clotting time, maximum optical density and lysis time, correlated respectively with the activated concentrations of acetylsalicylic acid (a drug that affects hemostasis), aprotinin (fibrinolysis activator) and venoruton (fibrinolysis inhibitor). The obtained results confirmed that the test we propose for monitoring clot formation, stabilization and lysis is sensitive and enables precise estimation of the processes studied. In our opinion, it can be a useful tool in drug screening investigations. Blood Coagul Fibrinolysis 18:611–618 ß 2007 Lippincott Williams & Wilkins. Blood Coagulation and Fibrinolysis 2007, 18:611–618 Keywords: acetylsalicylic acid, clot formation, fibrinolysis, in-vitro method a Department of Pharmaceutical Biochemistry and bDepartment of Pharmaceutical Chemistry and Drug Analysis, Medical University of Lodz, Lodz, Poland Correspondence to Dr Joanna Sikora, Department of Pharmaceutical Chemistry and Drug Analysis, Muszynskiego 1, 90-151 Lodz, Poland Tel: +48 42 677 92 95; fax: +48 42 677 92 50; e-mail: [email protected] Received 25 January 2007 Revised 10 May 2007 Accepted 10 May 2007 partial thromboplastin time, fibrinogen concentration and plasminogen level [3]. He et al. [4,5] also applied optical measurements of clotting and fibrinolysis in their studies. They introduced a new parameter that allows for an overall evaluation of the processes studied, and calculated the area under coagulation and fibrinolysis curves to determine overall hemostasis potential. This method with some modifications was used in both routine and research studies [2,6–9]. Although 100 years have passed since the invention of acetylsalicylic acid (ASA), research assessing its properties and therapeutic action is still conducted. Emphasis has been recently placed on ASA application in cardiovascular prophylaxis [10]. On the other hand, the amount of alarming reports on ASA resistance has increased and this phenomenon may independently correlate with the increase in cardiovascular events risk [11]. Moreover, numerous studies confirm that ASA, apart from antiplatelet action, also affects clot formation and lysis [12,13]. ASA causes lysine residue acetylation of various proteins of procoagulative (fibrinogen and prothrombin) as well as anticoagulative action (antithrombin). Acetylation of lysine residues in fibrinogen influences the clot structure and stabilization through factor XIII-mediated formation of cross-link bonds between fibrin fibers [14]. The results 0957-5235 ß 2007 Lippincott Williams & Wilkins Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited. 612 Blood Coagulation and Fibrinolysis 2007, Vol 18 No 7 of the studies evaluating the ASA effect on fibrinolysis, however, are ambiguous. The impact of ASA activity is thought to be dependent on the initial plasma fibrinolytic activity, the dose, and the time of its administration [6]. Despite the fact that all the mechanisms by which ASA affects hemostasis are not clear, it is well established that this drug influences both coagulation and fibrinolysis [6,10–14]. In the present study, our aim was to develop a simple, routine and accurate test for overall evaluation of clot formation and lysis (CL-test) that allows for continuous registration and for precise estimation of the processes studied, and can be used in in-vitro drug screening. ASA was used as a model drug to check the usefulness of our CL-test. Materials and methods Sample preparation Venous blood was obtained from healthy human volunteers, who had abstained from aspirin and other drugs for at least 2 weeks. Platelet-poor plasma was obtained by centrifugation (1500 g, 20 min, 48C) of platelet-rich plasma. The platelet-rich plasma was obtained by centrifugation (200 g, 10 min, room temperature) of anticoagulated blood (3.2% buffered sodium citrate used in a 1 : 9 volume ratio, Vacuette Coagulation Tubes; Greiner Bio-One, Kremsmünster, Austria). The study protocol complies with the Declarations of Helsinki and Tokyo. Reagents Reagents used for the study were freshly prepared from the stock solutions. Thrombin (400 IU) (Biomed, Lublin, Poland) was dissolved in 0.15 mol/l NaCl, giving a concentration of 400 IU/ml. Stock solution was stored in small portions (20 ml) for up to 1 month at 208C. Then 20 mg actilyse recombinant tissue plasminogen activator (t-PA) (Boehringer, Ingelheim, Germany) was dissolved in 20 ml manufacturer’s solvent, giving a concentration of 1 mg/ml, and was stored in small aliquots at 708C until further use. Fresh reactant solutions of thrombin and t-PA were maintained during the assay in an ice-water bath for no longer than 1 h. Tris-buffered saline (TBS) was prepared by adding 90 ml of 0.15 mol/l NaCl into 10 ml of 0.15 mol/l buffer Tris–HCl, pH 7.4, at 378C (adjusted with HCl). Sodium chloride, Tris, and HCl were obtained from Polish Chemical Reagents (Gliwice, Poland). TBS was stored for up to 1 month at 48C. Aprotinin (Traskolan) was obtained from Jelfa S.A. (Jelenia Góra, Poland), venoruton from Zyma SA (Nyon, Switzerland), ASA from Serva (Heidelberg, Germany), and D,L-lysin-mono-(acetylsalicylate) (Aspisol) from Bayer AG (Leverkusen, Germany). ASA solution was prepared before the assay commenced: 9.01 mg ASA was dissolved in 10 ml deionized water, giving a concentration of 5 mmol/l. A Cecil CE 1011 spectrophotometer (Cecil, London, UK) (378C, with stirring) was computerized with the authors’ own program, which enables not only continuous registration but also quick and easy estimation of the investigated processes. Technical procedure The CL-test with our own computer program, which evaluates the kinetic parameters of the examined process, was used in in-vitro screening studies. The test was based on the assumption of the global assay of coagulation and fibrinolysis with the use of optical measurements [2–5]. To obtain a clotting and lysis curve, 167 ml platelet-poor plasma was diluted in a disposable plastic cuvette with 313 ml (control) or 288 –308 ml TBS, 5–30 ml examined drug and 5 ml t-PA (final concentration, 60 ng/ml). It is also possible to obtain only a fibrin clot formation curve. In this case, 5 ml TBS was used instead of t-PA. Transmittance changes were measured continuously by a spectrophotometer at 405 nm and were registered in the computer program. The instrument was set for 100% transmission with platelet-poor plasma diluted with TBS prior to each reading. The examined sample was preincubated at 378C for 3 min. Then (when baseline stabilized) 10 ml thrombin (final concentration, 0.5 IU/ml) was added to start the process. The sample was stirred at 800 rpm for 10–15 s during thrombin addition. As shown in Fig. 1, the curve is generated over the course of the assay reactions and has a baseline transmittance with a peak at the moment of thrombin addition (indicator 0), and three consequent phases. Phase 1 (Fig. 1, light gray) corresponds to plasma fibrin generation triggered by exogenous thrombin and is reflected by a progressive decrease in transmittance to a point of minimum. Phase 2 (Fig. 1, gray) stands for the plateau of maximal decrease in transmittance and is the moment of stable clot formation. A final increase in transmittance (phase 3; Fig. 1, white) indicates the fibrinolytic potential in response to exogenous t-PA. Curves were recorded continuously and evaluated by the computer program. The calculated parameters of clotting and fibrinolysis are shown in Fig. 1. Introduction of 10 marks (To, R, 0–7), automatically placed in the appropriate points of study curves, enables calculation of 15 kinetic parameters of clot formation and lysis. There is also the possibility of manual change in the position of marks, in case of nontypical curves. The computer program can also be used to record platelet shape change, aggregation [15,16], and clot formation and fibrinolysis curves with the use of different activators (such as calcium ions, thrombin, t-PA, streptokinase, urokinase). Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited. Test of clot formation and fibrinolysis Kostka et al. 613 Fig. 1 that examines clot solubility in 5 mol/l urea solution [17] – that the amount of calcium ions present in citrate plasma was sufficient for activation of factor XIII and stabilization of fibrin structure. 0 Light transmission (%) 20 Thrombin Tt Tf Ti Tc The experimental conditions we proposed enable observation of a possible drug influence on all three phases of this process at a time that does not exceed 30 min. 40 60 Sr Sc Sf Lv ° 80 To provide an optimal condition similar to the physiological environment, thermostating (378C) and buffer (pH 7.4 at 378C) were used. Fmax Lmax Fv ° 100 0 To R12 5 3 4 10 5 6 7 15 20 Typical curve of clotting and fibrinolysis with parameters evaluated in the CL-test demonstrated. Phase I – clot formation (light gray): Tt (s), thrombin time [time elapsed from thrombin addition (indicator 0) to coagulation beginning (indicator R)]; Fmax (%T), maximum clotting [i.e. the transmittance difference between the baseline (indicator To) and minimum transmittance (indicator 4)]; Tf (s), plasma clotting time (from indicator 1 – means 10% of Fmax – to indicator 3 – means 90% of Fmax); Fvo (%T/min), initial plasma clotting velocity corresponds to the site of the quickest transmittance change (indicator 2); Sr (%T x min), area under the clot formation curve. Phase II – forming a stable clot (gray): Tc (s), clot stabilization time (from indicators 3 to 5); Sc (%T x min), area under the curve of a stable clot formation. Phase III – fibrinolysis (white): Lmax (%T), maximum lysis [i.e. the transmittance difference between the minimum transmittance (indicator 4) and the baseline (indicator 7)]; Tl (s), fibrinolysis time (from indicators 5 to 7); Lvo (%T/min), initial clot fibrinolysis velocity corresponds to the site of the quickest transmittance change (indicator 6); Sf (%T x min), area under the fibrinolysis curve; CLAUC (%T x min), overall potential of clot formation and lysis (i.e. the areas under clotting, fibrinolysis and transition curves. CLAUC ¼ Sr þ Sc þ Sf). To, R, 0–7,– indicators used in the CL-test computer program. To check the method, the influence of various concentrations of model drugs has been examined. We have used aprotinin as an in-vitro model of fibrinolysis inhibitor [18] and venoruton [0-(b-hydroxyethyl)-rutoside] as the fibrinolysis activator [19]. In the CL-test, we have confirmed that aprotinin, depending on the concentration used, decreases the fibrinolytic capacities of plasma (Table 1) whereas venoruton causes fibrinolysis acceleration (Table 1). The intra-assay coefficients of variation for the CL-test were established for 10 samples of normal plasma. Each plasma sample was analyzed in triplicate or duplicate under the same assay conditions. Intra-assay coefficients of variation for clotting parameters were between 1.1 and 4.4%, for the clot stabilization phase were between 6.7 and 7.9%, and for fibrinolysis parameters were between 0.9 and 9.7%. Effect of acetylsalicylic acid on clot formation (phases I and II) and fibrinolysis (phase III) Data analysis The results are presented as the mean SD. Significance of differences between groups was established by Student’s t-test. A value of P less than 0.05 was considered statistically significant. Results Clotting and lysis test We have performed several experiments to check how the system behaves at different thrombin and t-PA concentrations, with and without calcium ions. The effect of various concentrations of calcium ions alone (3.75–17.5 mmol/l) and with thrombin (0.04-1 IU/ml; data not shown), and of thrombin alone (0.125–1 IU/ml) and with t-PA (30–1400 ng/ml), was investigated by the CL-test (Fig. 2a,b). We have experimentally found that the concentrations of 0.5 IU/ml thrombin and 60 ng/ml t-PA are optimal in in-vitro drug screening. Exogenous calcium ions were not added to the sample, and high thrombin concentration (0.5 IU/ml) was used to directly initiate fibrin formation. This eliminates the effect of thrombin generation on the processes studied [12]. We have experimentally confirmed – by the method In the second part of this study, we performed several experiments with ASA to check whether our proposed invitro model for drug screening can be a useful tool to evaluate changes in plasma clot formation and fibrinolysis. ASA was added to diluted plasma at concentrations of 50, 100, 200 and 300 mmol/l and the parameters of the three phases together were measured (Fig. 3 and Table 2). The range of ASA concentrations used in our study was approximate to the maximal plasma concentrations reached after oral administration [6,10] and approximate to the concentrations (1–1000 mg/ml) used by other authors in in-vitro experiments [6,20]. When only clot formation was examined, there was no significant influence of different ASA concentrations on the evaluated parameters of phases I and II (data not shown). Figure 3 presents the influence of different concentrations of ASA on clotting and fibrinolysis processes induced by thrombin and t-PA (data obtained with the same plasma). Table 2 presents the means SD of the examined CL-test parameters for 50, 100, 200 Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited. 614 Blood Coagulation and Fibrinolysis 2007, Vol 18 No 7 Fig. 2 (a) 0 1 175 ng/ml t-PA 2 300 ng/ml t-PA 3 700 ng/ml t-PA 4 1400 ng/ml t-PA Light transmission (%) 20 40 1 60 80 100 2 3 4 120 0 5 10 15 20 25 Time (min) (b) Light transmission (%) 0 1 0.125 IU/ml thrombin 2 0.250 IU/ml thrombin 3 0.5 IU/ml thrombin 4 1.0 IU/ml thrombin 20 40 60 80 4 100 2 1 3 120 0 5 10 15 20 25 Time (min) Curve Tt (s) Fmax (%T) Tf (s) 20.1 19.5 19.9 20.3 63.7 62.6 60.8 64.1 89.9 86.2 72.9 65.7 (b) Thrombin 1 325.0 2 134.0 3 52.6 4 32.6 17.3 41.3 58.0 60.6 88.5 86.8 79.7 65.0 (a) t-PA 1 2 3 4 Tc (s) Lmax (%T) Tl (s) Lvo (%T/min) CLAUC (Sr þ Sc þ Sf) (%TMmin) 242 258 263 277 772 548 166 62 30.9 56.0 59.3 63.9 774 431 160 79 5.1 13.1 26.4 57.3 1224.5 (73.3 þ 803.2 þ 348.0) 832.5 (69.6 þ 52.8 þ 234.1) 273.5 (56.4 þ 150.6 þ 66.5) 153.0 (55.4 þ 62.0 þ 35.6) 12.8 43.4 132.0 195.0 26 31 166 219 17.2 42.3 59.5 62.0 115 122 133 145 8.2 24.1 27.6 26.2 41.9 (13.7 þ 8.1 þ 20.1) 101.6 (36.4 þ 19.6 þ 45.6) 274.9 (53.8 þ 155.4 þ 65.5) 338.2 (47.4 þ 215.5 þ 75.3) Fvo (%T/min) Effects of various (a) tissue-type plasminogen activator (t-PA) concentrations (175–1400 ng/ml) and (b) thrombin concentrations (0.125–1 IU/ml) on CL-test parameters (data obtained with the same plasma). For definitions, see Fig. 1. Table 1 Effects of various concentrations of aprotinin (fibrinolysis inhibitor) and venoruton (fibrinolysis activator) on CL-test parameters Aprotinin (n ¼ 2) 0 (control) 1 KIU/ml 10 KIU/ml 100 KIU/ml Venoruton (n ¼ 2) 0 (control) 100 mmol/l 200 mmol/l Tt (s) Fmax (%T) Tf (s) Fvo (%T/min) Tc (s) Lmax (%T) Tl (s) Lvo (%T/min) 23.2 26.3 28.8 29.9 54.3 56.0 55.1 59.5 44.0 52.6 68.8 87.7 222 205 197 201 218 242 332 665 61.8 63.5 59.0 142 152 332 38.2 31.6 11.5 M M M 31.8 34.1 33.3 37.1 37.9 38.5 53.5 50.4 44.3 123 126 132 286 259 193 33.7 36.9 39.5 470 415 231 5.6 7.0 17.7 CLAUC (Sr þ Sc þ Sf) (%T min) 277.6 (28.7 þ 191.4 þ 57.5) 316.7 (35.5 þ 219.3 þ 61.8) 473.9 (46.5 þ 295.3 þ 132.0) 1122.1 (65.7 þ 1056.4 þ 0M) 360.4 (23.5 þ 171.7 þ 165.2) 324.5 (23.0 þ 161.0 þ 140.5) 209.2 (19.8 þ 120.0 þ 69.4) See Fig. 1 for definitions. M 100% inhibition. Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited. Test of clot formation and fibrinolysis Kostka et al. 615 Fig. 3 0 1 Control 2 3 50 micromol/l ASA 100 micromol/l ASA 4 200 micromol/l ASA 5 300 micromol/l ASA Light transmission (%) 20 40 60 80 4 100 1 5 3 2 120 0 5 10 20 15 25 Time (min) Curve Tt (s) Fmax (%T) Tf (s) Fvo (%T/min) Tc (s) Lmax (%T) Tl (s) Lvo (%T/min) 1 2 3 4 5 140 140 149 128 132 37.1 36.4 37.8 37.3 38.9 159 145 145 129 144 33.5 32.2 32.0 35.8 36.7 335 270 248 207 280 34.6 35.1 37.8 37.6 38.2 258 209 211 197 226 8.8 10.8 11.6 12.1 10.9 CLAUC (Sr þ Sc þ Sf) (%TMmin) 391.1 305.0 283.5 245.1 325.6 (67.9 þ 205.1 þ 118.1) (58.7 þ 159.4 þ 86.9) (59.8 þ 150.8 þ 72.9) (53.1 þ 125.4 þ 66.6) (62.1 þ 175.7 þ 87.8) Effects of 50, 100, 200 and 300 mmol/l acetylsalicylic acid (ASA) on clotting and fibrinolysis curves. The final concentrations of exogenous thrombin and t-PA were 0.5 IU/ml and 60 ng/ml, respectively (data obtained with the same plasma). For definitions, see Fig. 1. and 300 mmol/l ASA. For 200 mmol/l ASA there were significant differences, in relation to the control, in the areas under the clotting curve (#Sr) and stable clot formation curve (#Sc). Moreover, the overall clot formation and fibrinolysis potential (areas under clotting, fibrinolysis and transition curves, #CLAUC), the time of stable clot formation (#Tc) and the time of clot lysis (#Tl) decreased statistically significantly. When 100 mmol/l ASA was used, we observed a significant decrease only in CLAUC and Sc. In the case of 50 and 300 mmol/l ASA, there was no significant influence on Table 2 the coagulation and fibrinolysis parameters. Owing to weak ASA solubility in water and the possibility of precipitation, however, we performed additional tests with D,L-lysin-mono-(acetylsalicylate) (Aspisol), which is water-soluble and hydrolyzes to ASA. Preliminary results obtained with Aspisol were parallel to those with ASA. Aspisol concentrations of 100 and 200 mmol/l (concentrations converted and expressed as ASA concentrations in the sample) accelerated fibrinolysis, whereas higher concentrations (300–3000 mmol/l) did not cause such (as above) effect (data not shown). In-vitro effects of different acetylsalicylic acid (ASA) concentrations on CL-test parameters Tt (s) Fmax (%T) Tf (s) Fvo (%T/min) Sr (%T x min) Tc (s) Sc (%T x min) Lmax (%T) Tl (s) Lvo (%T/min) Sf (%T x min) CLAUC (%T x min) Control (n ¼ 13) 50 mmol/l ASA (n ¼ 10) 100 mmol/l ASA (n ¼ 7) 200 mmol/l ASA (n ¼ 10) 300 mmol/l ASA (n ¼ 10) 111.2 13.3 47.9 8.2 153.2 12.1 44.1 15.1 80.7 13.5 352.8 65.4 277.6 96.5 46.9 7.9 314.7 23.1 9.9 1.4 148.3 35.32 506.6 142.2 114.0 33.5 44.8 8.6 152.9 23.6 41.8 17.3 75.5 42.0 334.1 7.0 213.8 57.0 42.0 5.7 272.4 61.0 9.9 2.0 128.8 55.5 430.3 97.0 119.1 30.7 44.0 8.5 149.7 24.1 39.1 16.5 71.7 13.5 292.9 78.4 178.5 43.1MM 44.0 8.2 269.9 65.6 10.8 2.4 111.0 44.2 344.3 68.1MM 104.4 29.7 44.3 5.1 141.4 17.8 40.5 9.0 68.4 13.5MM 255.3 27.5MM 182.7 31.8MM 44.3 5.2 251.1 51.5MM 11.5 2.8 103.0 30.8 351.0 72.9MM 100.9 22.8 48.5 10.0 150.0 23,8 44.7 22.9 77.0 20.1 304.7 99.4 249.4 125.3 47.9 9.5 319.2 62.5 9.7 2.1 147.5 54.4 473.9 192.8 See Fig. 1 for definitions. MM P ¼ (0.05–0.001) versus control. Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited. 616 Blood Coagulation and Fibrinolysis 2007, Vol 18 No 7 Discussion In recent years, growing interest in a global assay of coagulation and fibrinolysis that uses optical measurement of clot formation and lysis can be observed [2]. In the present study we have developed an optical method for overall evaluation of clot formation and fibrinolysis (the CL-test) in human plasma, which can be used in in-vitro drug screening. Implementation of continuous registration and our own computer program that calculates 15 kinetic parameters (Fig. 1) allowed for overall, as well as detailed, evaluation of the examined processes. As it is of crucial importance that the test used for drug screening should be sensitive enough to catch even subtle changes induced by studied compounds, we have performed several experiments to choose the most suitable concentrations of thrombin and t-PA, and other experimental conditions, and have checked the results using aprotinin, venoruton and ASA, drugs with a known effect on hemostasis. Various environmental factors, such as salt and protein concentrations, ion contents, and so on, exert an influence on fibrin clot formation and its structure [21–23]. While performing measurements, the maintenance of constant pH and temperature levels, due to their impact on protein involved in molecular interactions such as thrombin– fibrinogen binding, are of crucial significance [22]. In our experiments, in order to provide an optimal, similar to physiological environment, thermostating (378C) and buffer (pH 7.4 at 378C) were used. We did not add calcium ions to the sample and applied a high concentration of thrombin (0.5 IU/ml). Addition of small amounts of thrombin (0.05 IU/ml) does not result in coagulation initiation but induces a feedback reaction leading to endogenous thrombin generation, and by that to clot formation [12]. The concentration of thrombin used in our method induces clotting directly, and thus we eliminate the effect of thrombin generation on the processes studied. For the same reason, application of exogenous calcium was ceased. We confirmed that, by means of the method that examines clot solubility in 5 mol/l urea solution [17], the amount of calcium ions in diluted citrate plasma was sufficient to activate factor XIII and to stabilize the fibrin structure. Under such experimental conditions, fibrinogen function should be the main contributor to variations in fibrin structure. in the amounts of thrombin and t-PA used (Fig. 2a,b). In our proposed experimental conditions, the thrombin and t-PA concentrations are constant and ensure that even subtle changes in all three phases of examined processes can be detected, as confirmed with aprotinin and venoruton, which is important in drug screening tests. We used area under the curve for the overall evaluation of clotting, clot stabilization and fibrinolysis phases. Owing to the continuous recording and the computer evaluation of the processes, we introduced our own parameters assessing the overall potential of clotting and fibrinolysis (CLAUC), the overall clotting potential (Sr), the clot stabilization phase (Sc) and the overall fibrinolysis potential (Sf). The computer program also enables one to determine kinetic parameters such as the times and initial velocities of those processes (Fig. 1). In our opinion, such a form of clot formation and fibrinolysis evaluation may find application in drug screening. There are numerous studies substantiating clinical efficacy of ASA as an antithrombotic drug. The majority of these studies’ concerns the impact on platelet reactivity [24], chiefly through irreversible inhibition of platelet cyclooxygenase-1 and also through reduction of expression of adhesive molecule binding monocytes, neutrophils and platelets on the surface of endothelial cells [25]. The mechanism of ASA action on plasma coagulation and fibrinolysis factors, however, has not so far been completely elucidated. We have used ASA, a model drug that influences both coagulation and fibrinolysis, to check whether the CLtest is sensitive enough to catch its induced changes in clot formation, stabilization and lysis. In the system studied, ASA concentrations of 100 and 200 mmol/l appeared to have a statistically significant influence on CLAUC. Shortening of the clot stabilization time (#Tc) and reduction of the area under the stable clot formation curve (#Sc), when the final fibrin organization and stabilization occur, as well as fibrinolysis acceleration (#Tl, #Sf) and reduction of the area under the clotting curve (#Sr) affected the statistically significant decrease in CLAUC at the concentration of 200 mmol/l. In our experimental conditions we have found that the ASA concentration of 200 mmol/l has the strongest action, while higher (300 mmol/l) and lower (50 mmol/l) concentrations have not caused substantial changes in the effect observed. Preliminary results obtained with water-soluble (Aspisol) confirmed dose–response to ASA (data not shown). D,L-lysin-mono-(acetylsalicylate) When assessing sensitivity of the CL-test to the different concentrations of thrombin and t-PA, we observed obvious interdependence that changes in the clot formation and fibrinolysis curves are correlated with changes The results of our experiments are also supported by the study of Bjornsson et al. [26]. They observed fibrinolysis Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited. Test of clot formation and fibrinolysis Kostka et al. 617 acceleration, manifested by shortening of the clot lysis time, after treatment with aspirin. What is more, those authors reported an inverse dependence between the fibrinogen acetylation level and clot lysis time in in-vitro studies [26]. Numerous controversies on ASA’s effect on fibrinolysis [6] exist in the literature. Some of the in-vitro studies provide evidence that low ASA concentrations do not have any influence on fibrinolytic action, whereas high concentrations inhibit this process [6]. In other studies, the application of low aspirin doses has been found to impair thrombin generation and thrombincatalyzed reactions at the moment of blood vessel damage [27,28]. Antovic et al. [8] examined the influence of various ASA doses (37.5, 320 and 960 mg daily) on fibrin gel porosity, and they observed that low doses of ASA induce more favorable changes in the fibrin network than the higher ones. Williams et al. [13] also proved that low-dose ASA ingestion (75 mg daily) results in increased fibrin gel porosity in healthy individuals. Moreover, they found a tendency towards less efficient blockade of thromboxane formation with higher ASA dose (320 mg daily). ASA application may change the clot structure, the velocity of clot formation and fibrinolysis due to lysine acetylation present in the structure of prothrombin, fibrinogen and antithrombin III. Lysine occurring in fibrinogen is essential to form cross-link bonds, mediated by factor XIII, between the fibrin fibers. Its acetylation results in blocking bond formation and decreasing clot stabilization [14]. Acetylation of too many lysine residues, however, may result in a suboptimal change of the fibrinogen molecule [13]. ASA slows down conversion of prothrombin into thrombin, which contributes to formation of thicker fibers and clot structure loosening [12,29]. These changes enable t-PA to penetrate the clot and finally to enhance fibrinolysis, as lysis of clots with loose fibrin conformation made of thick fibers is faster than those with tight fibrin conformation made of thin fibers [23]. He et al. [30] studied the effect of ASA on fibrinous clot formation in vitro using the optical method and pure fibrinogen, thrombin, calcium ions and factor XIII. ASA was shown to reduce maximum absorbance in a dose-dependent manner, and to prolong the coagulation time. Together with the increase in ASA concentration, a decline in the amount of the clot-insoluble proteins affected by the alkaline urea solution was observed. These observations corroborate the inhibitory properties of ASA in relation to factor XIII activity [30]. In conclusion, the CL-test may be applied in drug screening tests evaluating their influence on the process of fibrinous clot formation and lysis (compounds that affect thrombin, fibrinogen and fibrinolysis). This has been confirmed by our studies with ASA, which revealed that the drug decreases overall clot formation and fibrinolysis potential (CLAUC), probably by clot structure changes that lead to fibrinolysis acceleration. The use of the computer program to determine coagulation and fibrinolysis kinetic parameters, as well as the overall evaluation of subsequent phases of the processes through calculation of the area under the recorded curve, provide the possibility of a rapid and simple assessment of the activity of the compound studied. Acknowledgement The present study was supported by grant No. 502-13229 of the Medical University of Łódź, Poland. References 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 Sidelmann JJ, Gram J, Jespersen J, Kluft C. Fibrin clot formation and lysis: basic mechanisms. Semin Thromb Hemost 2000; 26:605–618. Goldenberg NA, Hathaway WE, Jacobson L, Manco-Johnson MJ. A new global assay of coagulation and fibrinolysis. Thromb Res 2005; 116:345– 356. Glover D, Warner ED. The CLUE test – a multiparameter coagulation and fibrinolysis screening test using the platelet aggregometer. Am J Clin Pathol 1975; 63:74–80. He S, Bremme K, Blombäck M. A laboratory method for determination of overall haemostatic potential in plasma. I Method design and preliminary results. Thromb Res 1999; 96:145–156. He S, Antovic A, Blombäck M. A simple and rapid laboratory method for determination of hemostasis potential in plasma. II Modifications for use in routine laboratories and research work. Thromb Res 2001; 103:355–361. Buczko W, Mogielnicki A, Kramkowski K, Chabielska E. Aspirin and the fibrinolytic response. Thromb Res 2003; 110:331–334. Antovic A, Blomback M, Sten-Linder M, Petrini P, Holmstrom M, He S. Identifying hypocoagulable states with a modified global assay of overall haemostasis potential in plasma. Blood Coagul Fibrinolysis 2005; 16:585–596. Antovic A, Blomback M, Bremme K, He S. The assay of overall haemostasis potential used to monitor the low molecular mass (weight) heparin, dalteparin, treatment in pregnant women with previous thromboembolism. Blood Coagul Fibrinolysis 2001; 13:181–186. Curnow JL, Morel-Kopp M-C, Roddie C, Aboud M, Ward CM. Reduced fibrinolysis and increased fibrin generation can be detected in hypercoagulable patients using the overall hemostatic potential assay. J Thromb Haemost 2007; 5:528–534. Cerletti C, Dell’Elba G, Pecce R, Di Castelnuovo A, Scorpiglione N, Feliziani V, de Gaetano G. Pharmakokinetic and pharmacodynamic differences between two low dosages of aspirin may affect therapeutic outcomes. Clin Pharmakokinet 2003; 42:1059–1070. Hankey G, Eikelboom JW. Aspirin resistance. Lancet 2006; 367:606–617. Antovic A, Pernrby C, Jakobsson EG, Wallen HN, Hejemadahl P, Blomback M, He S. Marked increase of fibrin gel permeability with very low dose ASA treatment. Thromb Res 2005; 116:509–517. Williams S, Fatah K, Hjemdahl P, Blomback M. Better increase in fibrin gel porosity by low dose than intermediate dose acetylsalicylic acid. Eur Heart J 1998; 19:1666–1672. Undas A, Sydor WJ, Brummel K, Musiał J, Mann KG, Szczeklik A. Aspirin alters the cardioprotective effects of the factor XIII Val34Leu polymorphism. Circulation 2003; 107:17–20. Kostka B, Sikora J, Para J, Krajewska U, Korzycka L. A New nitrate derivative of piperazine: its influence on platelet activity. Blood Coagul Fibrinolysis 2007; 18:151–156. Kostka B, Sikora J, Aranowska K, Para J, Ochocki J. Effect of cis-platinum(II) amine phosphonate complexes on in vitro platelets reactivity. Acta Toxicol 2005; 13:113–121. Łopaciuk S. Blood coagulation tests. In: Pawelski S, editor. Laboratory diagnostics in haematology [in Polish]. Warsaw: PZWL; 1990. pp. 226– 227. Sodha NR, Boodhwani M, Bianchi C, Ramlavi B, Sellke FW. Aprotinin in cardiac surgery. Expert Rev Cardiovasc Ther 2006; 4:151–160. Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited. 618 Blood Coagulation and Fibrinolysis 2007, Vol 18 No 7 19 20 21 22 23 24 25 26 27 28 29 30 Kostka B, Michalska M, Krajewska U, Wierzbicki R. Blood coagulation changes in rats poisoned with methylmercuric chloride (MeHg). Pol J Pharmacol Pharm 1989; 41:182–189. Kupryś I, Kurowski M, Kuźminska B, Zielińska-Wyderkiewicz E, Górski P, Kuna P. Basophil degranulation test in the diagnosis of nonsteroidal antiinflammatory drug hypersensitivity [in Polish]. Pol Merkuriusz Lek 2005; 18:540–543. Carr ME Jr, Alving BM. Effect of fibrin structure on plasmin-mediated dissolution of plasma clots. Blood Coagul Fibrinolysis 1995; 6:567–573. Weisel JW, Nagasawami C. Computer modeling of fibrin polimeryzation kinetics correlated with electron microscope and turbidity observations: clot structure and assembly are kinetically controlled. Biophys J 1992; 63:111–128. Collet JP, Park D, Lesty C, Soria C, Soria G, Montalescot G, Weisel JW. Influence of fibrin network conformation and fibrin fiber diameter on fibrinolysis speed: dynamic and structural approaches by confocal microscopy. Arterioscler Thromb Vasc Biol 2000; 20:1354– 1361. Patrono C. Aspirin as an antiplatelet drug. N Engl J Med 1994; 330:1287– 1294. Lopez-Ferre A, Caramelo C, Esteban A, Alberola ML, Millas I, Monton N, Casado S. Effects of aspirin on platelet–neutrofil interactions. Circulation 1995; 91:2080–2088. Bjornsson TD, Schneider DE, Berger H Jr. Aspirin acetylates fibrinogen and enhances fibrinolysis. Fibrinolytic effect is independent of changes in plasminogen activator levels [abstract]. J Pharmacol Exp Ther 1989; 250:154–161. Undas A, Brummel K, Musial J, Mann KG, Szczeklik A. Blood coagulation at the site of microvascular injury: effects of low-dose aspirin. Blood 2001; 98:2423–2431. Szczeklik A, Musiał J, Undas A, Swadzba J, Gora PF, Piwowarska W, Duplaga M. Inhibition of thrombin generation by aspirin is blunted in hypercholesterolemia. Arterioscler Thromb Vasc Biol 1996; 16:948–954. Veklich Y, Francis CW, White J, Weisel JW. Structural studies of fibrinolysis by electron microscopy. Blood 1998; 92:4721–4729. He S, Blombäck M, Yoo G. Modified clotting properties of fibrinogen in presence of acetylsalicylic acid in purified system. Ann N Y Acad Sci 2001; 936:531–535. Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.