* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Cardiovascular System
Quantium Medical Cardiac Output wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Coronary artery disease wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Cardiac surgery wikipedia , lookup
Myocardial infarction wikipedia , lookup
Jatene procedure wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
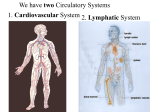
Circulation: The Cardiovascular and Lymphatic Systems 1 Cardiovascular System Cardiovascular system Consists of heart and blood vessels Encompasses blood circulation Delivers oxygen and nutrients to cells Carries away waste products Lymphatic system Drains fluid and proteins from tissues, returns them to bloodstream 2 Cardiovascular System 3 The Heart Located between lungs Myocardium = thick muscle layer Endocardium = inside lining Epicardium = Outside lining Pericardium = surrounding fibrous sac 4 Location of Heart The heart is encased in and separated from the walls of the pericardial cavity by three linings: the epicardium, which forms the outer part of the heart; the pericardial sac and the pericardium The heart fits tightly inside the pericardial cavity, a subcavity of the thoracic cavity. The pericardial cavity is lined with a serous ( thin) membrane called the pericardium, and the heart is within yet a second lining called the pericardial sac. This sac contains about half an ounce of fluid, which lies between it and the heart’s outer lining 5 The structure of the heart The membrane forming the outer lining of the heart is called the epicardium Immediately beneath the epicardium is the myocardium, comprising the muscles, blood vessels and nerve tissue that make up the bulk of the heart The heart’s inner surface is called the endocardium 6 Heart (cont’d) Atrium Upper receiving chambers Atria are separated by interatrial septum (plural septa) Ventricle Lower pumping chambers Pulmonary circuit (right side to lungs) Systemic circuit (left side to rest of body) Ventricles are separated by interventricular septum Also, each atrium is divided from each ventricle by an atrioventricular septum, which contains various valves 7 Illustrated Heart 8 Heart valves The right atrioventricular valve, also sometimes called the tricuspid valve, leads from the right atrium into the right ventricle The pulmonary semilunar valve connects the right ventricle to the lungs, which also connect to the left ventricle through the left atrium by way of the left atrioventricular valve, also sometimes called the bicuspid ot mitral valve The aortic semilunar valve leads out of the left ventricle 9 Blood Flow Through the Heart When blood comes back to the heart after having delivered oxygen and other nutrients to the body’s cells, it needs to be replenished before going out again. It re-enters the heart at the atrium Right atrium receives blood from body Enters right ventricle and is pumped to lungs Oxygenated blood returns to left atrium Enters left ventricle and is pumped to rest of body One-way valves force blood flow forward Heart sounds produced when valves close 10 The Heartbeat Systole = contraction (emptying the heart) Diastole = relaxation ( refilling chambers) Heart beats start with both atria contracting Immediately thereafter both Ventricles contract Wave of increased pressure in the vessels following ventricular contraction is pulse Contractions are stimulated by electrical impulse Blood Pressure Force of blood exerted against wall of blood vessel Measured by sphygmomanometer Measured as both systolic and diastolic, such as 120/80 11 Pacemaker and conduction system of the heart Contractions are stimulated by a built-in system that regularly transmits electrical impulses through the heart They include the sinoatrial (SA) node, called the pacemaker because it sets the rate of the heart beat The atriopventricular (AV) node, the AV bundle (bundle of His) the left and right bundle branches and Purkinje fibers 12 Conduction System of the Heart 13 Clinical Aspects of the Circulatory System Atherosclerosis Accumulation of fatty deposits within artery Risk factors: High levels of lipoproteins (especially LDL’s) Smoking High blood pressure Poor diet Inactivity Stress Family history 14 Thrombosis and Embolism Definitions: Thrombosis = formation of blood clot Thrombus = blood clot Embolism = blockage of blood vessel Embolus = blockage mass Blockage is usually blood clot Blockage can also be air, fat, bacteria, or other solid materials Stroke = blockage in a cerebral vessel 15 Aneurysm Weakened arterial wall ballooning out Caused by: Atherosclerosis Malformation Injury 16 Heart Diseases Coronary artery disease Results from atherosclerosis Early sign is angina pectoris (chest pain) Diagnosed by: ECG Stress tests Coronary angiography Echocardiography Treatments: Control of exercise, administration of nitroglycerin Angioplasty (PTCA) 17 Bypass (CABG) Heart Diseases (con’t) Myocardial infarction = heart attack Symptoms: Epigastric pain Pain extending to jaw, arms Pallor (turns pale) Diaphoresis Nausea Dyspnea (difficulty breathing) May also be burning sensation similar to heartburn 18 Heart Diseases (cont’d) Arrhythmia Irregularity of heart rhythm Bradycardia = slower than average Tachycardia = faster than average Fibrillation = extremely rapid, ineffective Controlled on Long term with pacemaker 19 Heart Diseases (cont’d) Heart failure Heart fails to empty effectively, leading to edema Congenital heart disease Birth defects Most can be corrected surgically Rheumatic heart disease Streptococcus infection damaging heart valves 20 21 22 23 24 The Vascular System Arteries and arterioles Carry blood away from heart Vasoconstriction and vasodilatation Become smaller as they go away from the heart? Capillaries Smallest vessels Where exchange between blood and tissues happens Veins and venules Carry blood back to heart 25 26 Conducting arteries Sometimes called elastic arteries and can have an inside diameter as great as an inch The aorta is an example of a conducting artery The pulmonary artery and aortic trunk are examples of conducting arteries which move blood away from the heart Three major conducting arteries branch from aortic arch. They are the brachiocephalic trunk, the left common carotid artery and the left subclavian artery Both the right subclavian artery and the right common carotid artery attach to the brachiocephalic trunk 27 28 Medium size arteries, ( also called muscular arteries because they contain a lot of muscle tissue) typically have an inside diameter of about a sixth of an inch (eg external carotid artery) Arterioles are the smallest arteries, with an average inside diameter of 0.0018 of an inch or about 1/100 the size of a medium size artery Arteries and arterioles connect to the capillaries which can be as tiny as one blood cell ( or about ¼ the size of an arteriole in diameter) 29 Principal Arteries 30 Veins Veins carry blood back to the heart. They follow the same path as the arteries ( with blood flowing in the reverse direction) Also, like arteries, they vary in diameter, becoming larger as they approach the heart because of the increasing volumes of blood they must carry The vein counterparts of the conducting arteries are the superior vena cava and the inferior vena cava. Together they are known as the venae cavae Medium veins and venules are the counterparts of the muscular arteries and arterioles Superior vena cava drains blood from upper body, including head neck shoulders and arms Inferior vena cava receives blood from the lower body, the dividing line being the diaphragm 31 Principal Veins 32 33 Disorders of the Veins Varicose veins Breakdown in valves with chronic dilatation Contributing factors: Heredity Obesity Prolonged standing Pregnancy 34 Disorders of the Veins (con’t) Phlebitis = inflammation of veins Causes: Infection Injury Poor circulation Valve damage Can result in thrombophlebitis (blood clot) Most damaging if occurring deep 35 Hypertension Commonly known as high blood pressure Contributing factor in many conditions Defined as systolic > 140, diastolic > 90 Causes left ventricle to enlarge First defense: diet and life habits 36 Blood and Immunity 37 Blood Plasma 90% water Rest contains: Nutrients Electrolytes (dissolved salts) Gases Albumin (protein) Clotting factors Antibodies Wastes Enzymes Hormones Relative acidity (pH) steady at 7.4 38 Blood Cells Produced in red bone marrow Three kinds: Red = erythrocytes White = leukocytes Platelets = thrombocytes 39 Erythrocytes Main function: carry oxygen to cells Most numerous of blood cells Short lifespan (120 days) requires constant replacement Production regulated by erythropoietin (hormone made in kidneys) Leukocytes Protect against foreign substances Five different types: Neutrophils Eosinophils Basophils Lymphocytes Monocytes 40 Leukocytes Phagocytes are often the first immune system cells on the scene when injury occurs. They prevent infection by cleaning away pathogens and debris Phagocytes are two types: microphages and macrophages The average human body contains one trillion lymphocytes which include NK cells, T cells and B cells T cells make up about 80% of the total number of lymphocytes T lymphocytes depend on the thymus for their activation T lymphocytes are prompted by a specific antigen; a substance 41 that induces sensitivity Leukocytes Antigens also stimulate the immune system to generate antibodies, which can produce immunity from future attacks by the same type of antigen Unlike NK cells which roam the body looking for intruders, T cells attack only when they recognize a specific antigen, and then only after receiving instructions from special T cells that distinguish between good and bad antigens B lymphocytes are derived from bone marrow. Like NK cells, they roam the body looking for intruders But unlike NK cells, they stop in lymph tissue to seek out foreign antigens However they do not attack until the special T cells instruct them to do so 42 43 44 Platelets Important for hemostasis Most active during coagulation Stick together to plug injury site Interact with clotting factors in plasma to make wound-sealing clot Convert fibrinogen to threads of fibrin Threads of fibrin trap blood cells and plasma to make clot 45 Blood Types Determined by genetically inherited proteins Most familiar groups are ABO and Rh Important to match for blood transfusions Compatible types determined by cross-matching 46 TEST ABBREVIATION DESCRIPTION Differential count Diff Relative % of the different types of leukocytes hematocrit Ht, Hct, crit Relative % of packed red cells in a given volume of blood Packed cell volume PCV hematocrit Mean corpuscular volume MCV Volume of an average red cell Mean corpuscular hemoglobin MCH Average weight of hemoglobin in red cell Mean corpuscular hemoglobin concentration MCHC Average concentration of hemoglobin in red cell Erythrocyte sedimentation rate ESR Rate of setting of erythrocytes per unit of time, used to detect infection or inflammation complete blood count CBC Series of tests including cell counts, hematocrit, hemoglobin, and cell 47 volume measurements The Immune System Launches specific attacks on disease organisms Involves components of lymphatic system and blood Immune system response from T cells or B cells T cells mature in thymus gland B cells mature in lymphoid gland Passive immunity: Transfer of antibodies Naturally (mother’s milk) Artificially (immune serum) Active immunity: Individual’s own response to disease organism Natural contact 48 Vaccine Clinical Aspects: Blood Anemia Decrease in hemoglobin in blood Can result from: Too few red blood cells Cells are too small Too little hemoglobin Key tests involve blood counts Symptoms include fatigue, shortness of breath Aplastic anemia = destruction of bone marrow Nutritional anemia (includes pernicious anemia) = deficiency of vitamin B12 Sideroblastic anemia = body doesn’t use iron properly 49 Hemorrhagic anemia = results from blood loss Types of Anemia (con’t) Thalassemia (includes Cooley anemia) Hereditary disease causing rupture of red cells Affects production of hemoglobin Sickle cell anemia Mutation alters hemoglobin molecule Deformed cells block blood vessels and prevent tissues from receiving oxygen 50 Coagulation Disorders Thrombocytopenia Deficiency in number of platelets Disseminated intravascular coagulation Widespread clotting, obstructing circulation to tissues Hemophilia Hereditary deficiency of specific clotting factor Sex-linked disease: Passed from mother to son 51 Neoplasms Leukemia Rapidly dividing, but incompetent white blood cells Causes unknown, but may include radiation, heredity Treatment includes: Chemotherapy Radiation therapy Bone marrow transplantation 52 Neoplasms (con’t) Hodgkin disease Disease of lymphatic system that may spread Contains Reed-Sternberg cells (giant cells in lymph nodes) Non-hodgkin lymphoma Also malignant enlargement of lymph nodes More common, deadly than Hodgkin disease Multiple myeloma Cancer of blood-forming cells in bone marrow 53 Clinical Aspects: Immunity Hypersensitivity Commonly known as allergy More sensitive to allergens (pollen, dust) Anaphylactic reaction Severe generalized allergic response Must be treated with epinephrine (adrenaline) Delayed hypersensitivity reaction Involves T cells and takes 12 hours for onset (poison ivy) 54 Clinical Aspects: Immunity (con’t) Immunodeficiency Any failure in immune system (AIDS) Starts with HIV infection Leaves individual susceptible to other infections Autoimmune disorder Immune response to own tissues Cause may be: Failure of immune system Body cells altered by mutation or disease 55 The Lymphatic System Role in circulation: return excess fluid and proteins from tissues back to bloodstream Fluid known as lymph Lower part and upper left side of body drains into thoracic duct Upper right side of body drains into right lymphatic duct Other roles: Absorb digested fats Protect body from impurities, microorganisms Assist with immunity 56 Lymphatic Disorders Lymphadenitis = enlargement of lymph nodes Lymphedema = tissue swelling Lymphoma = neoplastic disease affecting white blood cells 57 58 Thymus Located behind the sternum Secretes thymosin, which help T cells develop Spleen It contains phagocytes, removes damaged red blood cells, and recycles and stores reclaimed iron from others Tonsils Any collection of lymph tissue can be called a tonsil include palatine, pharyngeal and lingual tonsils Lymph nodes They are structures of variable size that contain macrophages, filtering out disease-causing antigens and other debris as the lymph flows through them. These antigens are exposed to lymphocytes to start immune response Swollen glands reveal the presence of an infection or injury in the area of swollen gland 59 60