* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Inflammatory processes of the maxillofacial area (periodontitis
Survey
Document related concepts
Transcript
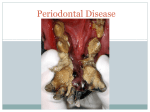
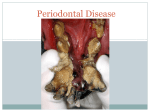
INFLAMMATORY PROCESSES OF THE MAXILLOFACIAL AREA (PERIODONTITIS, OSTEOMYELITIS, LYMPHADENITIS, ODONTOGENIC SINUSITIS, SIALADENITIS. ODONTOGENIC ABSCESSES, PHLEGMONS): ETHIOLOGY, PATOGENESIS, CLINICAL SYMPTOMS, TREATMENT, COMPLICATIONS. Infectious and inflammatory diseases constitute the basic group of the most frequent diseases of the maxillofacial area. Problems of prophylactics, diagnostics, and treatment of infectious and inflammatory diseases are of high importance nowadays. The reasons for this situation are that for the last century the number of people with such diseases has not just decreased, but on the contrary their incidence rates increased at certain periods of time in spite of constant improvement of prophylactic and diagnostic approaches, means and methods of treatment. This is not merely the problem of stomatology, it is a general social problem of our country. The number of people with infectious and inflammatory diseases in the maxillofacial area, the quality of rendered medical care, and so the number and severity of complications caused by these diseases, the terms of incapacity for work are connected with social and economic development of the country, the degree of development of its health care facilities, the level of specialist training and a number of other factors. Medical assistance to people with inflammatory diseases of the maxillofacial area should be rendered by qualified specialists either on an outpatient basis or (in most cases) at hospital at oral and maxillofacial surgery department. More than 90% of patients at first seek medical advice from dentists, otolaryngologist or surgeons at their local hospitals or at other commercial organizations. In this case a doctor should make the accurate diagnosis of the inflammatory disease as far as possible, choose the medical institution where patient can receive oral surgery services provided by skilled dental surgeons and admit the patient to hospital. The probability of possible complications, their severity, the terms of incapacity for work, the disease prognosis and even physical disability depend directly on how promptly and accurately the diagnosis of a respective disease is made as well as whether the treatment is provided in due time. For this reason each doctor regardless of his/her expertise in the area should have sufficient knowledge of ethiology and pathogenesis of inflammatory diseases: he/she should be able to diagnose them, provide necessary medical assistance, know the treatment principles, be able to predict probable course and outcomes of a disease, provide accurate diagnosis and render emergency care when there exists the risk of life-threatening complications of a disease. Ethiology, pathogenesis, classification of infectious and inflammatory diseases of the maxillofacial area. Inflammatory response results from interaction of exogenic (microbs, their toxins, waste and decay products) and endogenic ethiologic factors (factors and mechanisms of non-specific and immune responsiveness). Up to now it has not been possible to determine the overall spectrum of inflammatory processes agents using microbiological diagnostic methods. Thus, clinicians and microbiologists considered aerobes to be the ethiological factor of these diseases, because only this type of bacteria has been detected in the researched material, provided by patients. With improvement of microbiological research methods it has become possible to obtain evidence that anaerobes can be agents of odontogenic infection. In the course of the researches carried out during the last few years it was ascertained that not only staphylococci, but also different representatives of gram1 negative microflora: proteus, colibacillus, Klebsiella and others belong to basic agents of acute odontogenic infection. The great significance in ethiology of inflammatory diseases of the head and the neck has been attached recently to opportunistic microorganisms, asporous obligate anaerobic bacteria. Bacteroides and fusobacteria are the bacteria most frequently found among this type of bacteria. Usually these microorganisms can be found on mucous membranes of oral cavity. When the immune responsiveness of an organism is decreased and hemodynamic in inflammatory tissue is induced, bacteroids, fusobacteria and other opportunistic anaerobic microorganisms can cause pyoinflammatory diseases. The role of microflora is undoubtedly great. However, microorganism-microorganism relations have two-way connection; therefore the peculiarities of the course of the inflammation and development of complications are related not only to the peculiarities of microflora, but also to organism responsiveness, that is the property of an organism to respond to changes in the environment. In other words, responsiveness of an organism reflects the protective and adaptive properties of an organism and is caused by inherent and acquired factors. To a great extent it depends on sex, age, and environment conditions etc. Considering the problem of the pathogenesis of acute odontogenic inflammatory diseases, great attention is paid to sensitization of organism, producing of specific antibodies in response to coming of the antigens into tissues. The coming of the antigens first occurs owing to their ability to penetrate deep into tissues through tissue barriers. As a result of forming and continuous existence of the chronic infection nidus the number of penetrating antigens increases and the level of sensitization rises. In response to this organism is constantly producing specific antibodies, which support antibacterial immunity. The inflammatory process is likely to increase at the disturbance of the dynamic balance between micro- and macroorganism. It may be either the increase in the total effect, which damages from the direction of bacteria, or weakening or increase of reactivity. One of the major factors which contribute to the beginning of inflammatory process is rise in summary effect, which damages virulence of microflora, as a result of increase in the number of microbes/microorganisms. Another significant factor is injury of the demarcation zone (connective tissue capsula or leukocytic bank), which occurs at the injury or operative treatment. Development of acute suppurative inflammation against the background of the existing nidus of chronic infection arises as a rule after the physical or emotional overstrain, supercooling, overheating, and also after certain diseases (especially infectious diseases). The inflammatory processes of jaw are remarkable for greater variety of their clinical course, what gives the basis for their various classifications. One of them was suggested by A.G. Shargorodskyi and L. M. Tsepov (1979) 2 Classification of the odontogenic inflammatory processes by A.G.Shargorodskyi and L.M.Tsepov: А. Periodontitis: 1. Acute periodontitis (serous and purulent periodontitis); 2. Chronic periodontitis in the stage of exacerbation; 3. Chronic (granulating, granulomatous and fibrous periodontitis); B. Jaw periostitis: 1. Acute periostitis (serous and purulent); 2. Chronic periostitis; C. Jaw osteomyelitis: 1. By clinical course: а) acute; b) subacute; c) chronic; d) aggravated chronic. 2. By character of the spread: а) limited; b) diffusion; D. Abscesses and phlegmons: 1) face; 2) perimaxillary; 3) floor of oral cavity; 4) peripharyngeal; 5) tongue; 6) neck. E. Lymphadenitis of face and neck. PERIODONTITIS. Periodontitis - inflammatory process which affects the tissue of the periodontium and bones that support the teeth. The main cause of periodontitis is complicated caries. Distinct types of periodontitis: 1. Acute periodontitis: а) serous periodontitis (limited and generalised), b) purulent periodontitis (limited and generalised). 2. Chronic periodontitis: а) granulating periodontitis, b) granulomatous periodontitis, c) fibrous periodontitis. 3. Chronic periodontitis at the stage of exacerbation. 3 Clinical picture of acute periodontitis. The initial symptom of acute serous periodontitis is toothache, which becomes stronger when biting. This pain doesn’t usually irradiate, so it’s easy for the patient to determine the affected tooth. Another characteristic of periodontitis is softtissue swelling, minor regional lymphadenopathy, slightly painful lymph nodes. The affected tooth is a little loose and vertical percussion of the tooth is positive. At the same time there dental X-ray film shows no change. With the progression of the serous inflammatory process into purulent form of periodontitis the intensity of pain is growing. The pain becomes acute, throbbing and irradiates along the trigeminal nerve. There is acute pain every time one touches the tooth, which becomes loose. The patient notes, that the tooth seems to be growing. The mouth of the patient is half-open, mucous membrane of the alveolar process is hyperemic, edematous and painful within the borders of the injured tooth. Regional lymph nodes are enlarged and painful. Edema of the soft tissue is characteristic at this stage as well. There is deterioration of the general condition of the patient. The treatment of the acute periodontitis consists in creating of exudate outflow from the periapical region. The symptomatic and physical therapy is instituted. Granulating periodontitis is marked by painful sensation, which occasionally appears in the region of the affected tooth. The may be also no pain. It is clear from the anamnesis that tooth disturbs the patient for a long time. Examining the tooth, it is easy to determine whether there is any filling or cavity, which can be sounded indolently. Percussion of the tooth is usually painless. X-ray examination is of considerable importance in differential diagnostics of chronic periodontitis: fibrous periodontitis is marked by irregular enlargement of periodontal fissure; the characteristic feature of the granulomatous periodontitis is sharply delineated destruction zone of different shapes and size in periapical region, the granulating periodontitis is marked by destruction of the alveolar socket and destructive changes in spongy substance without anyand distinguished boundary between Fibrous, granulomatous granulating periodontitis pathologic zone and unaffected tissues. Treatment: 1. Extraction of the tooth; 2. Resection of the top of tooth root; 3. Dental reimplantation; 4. Hemisection of the tooth; 5. Ablation; 6. Coronary and radicular separation. 7. Replantation. PERIOSTITIS OF THE JAW. That is a disease, which is characterized by the spread of the inflammatory process on the periosteum of dental process and jaw from odontogenic or nonodontogenic focus. ACUTE PERIOSTITIS. Patient complains of pain and tissue swelling in the certain region of the jaw. Clinical picture. Acute periostitis is marked by overall intoxication, painful food intake. The face of the patient is skew owing to the soft-tissue edema in the affected zone of the jaw. One side of the alveolar process of maxilla (where subperiostomal abscess was formed) is deformed. The transition fold in this zone is smoothed out, the mucous is hyperemic and hydrotic. Treatment. 1. Extraction or treatment of the affected tooth (exudate outflow through root canal of the tooth). 2. Periosteotomy and draining of the subperiostomal abscess with the following draining of the wound. 3. General medical therapy (sulfonamides or antibiotics). CHRONIC PERIOSTITIS. Patients complain of the deformation of the jaw and slight pain in it. In anamnesis – pain in the affected tooth and its treatment. 4 Clinical picture. Chronic periostitis is marked by deformation of the face owing to the enlarged alveolar process of maxilla or mandible, which is slightly painful when doctor touches it. Other distinctive characteristics are a little smoothed out transition fold and cyanotic mucous tunic. No intoxication is observed and the general condition is almost not affected. Treatment. 1. Extraction or treatment of the affected tooth. 2. Periosteotomy in the region of the infiltration with the following draining of the wound, removing of the bone structure deformity. 3. Physical treatment modes appropriate for drained wound. OSTEOMYELITIS OF THE JAW. That is infectious, allergic and necrotic suppurative process, which develops in the bone structure due to some external and internal factors. ACUTE ODONTOGENIC OSTEOMYELITIS OF THE JAW. Patient complains of intensive pain in the jaw and group of teeth including the affected one, as well as deformation of the face. Clinical picture. The major symptoms of acute ontodogenic osteomyelitis are general condition disorder, high body temperature, intoxication, sleep and appetite disturbances. Other characteristics are distinct alteration of the hemogram, high ESR, protein in the urine. Face is skew owing to the existence of the soft-tissue edema; there is also presence of infiltration. Lymph nodes are enlarged and painful, with distinctive limited mobility. It may be difficult for the patient to open the mouth when the process is localised on the lower jaw in the molar teeth zone. The alveolar process of the maxilla or mandible is deformed from both sides (in the form of a cuff), the transition fold is smoothed out, the mucous tunic in this region is hydropic and hyperemic. Examining shows 3-4 loose teeth, destroyed or filled affected tooth and suppuration from the pockets near the proximate teeth. The disease is accompanied by formation of perimaxillary abscesses and phlegmons. The generalised inflammatory process in the lower jaw can cause Weinsan's symptom – paresthesia (lower lip numbness). X-ray investigation. No changes in the bone structure, only some characteristics of the chronic periodontitis in the affected tooth, can be shown by roentgenogram. Treatment. 1. Extraction of the affected tooth. 2. Periosteotomy of the alveolar process from two sides (vestibular and glossal, buccal and palatine) with draining of the wounds. 3. Perforation of bone in the region of affected tooth. 4. Draining of the abscesses, phlegmons and draining of the wounds. 5. Active general medical therapy (antibiotics, sulfonamides). CHRONIC ONTODOGENOUS OSTEOMYELITIS OF THE JAW. Patient complains of intermittent pain in the jaw and its deformation, presence of one or several continued draining sinus, some purulent fistulas. The anamnesis shows treated or destroyed affected tooth, periods of the exacerbation of the periodontitis, acute onset of the disease. Clinical picture. There is no general state disturbance as a rule, the symptoms of intoxication are characteristic only of the exacerbation stage. There can be distinguished destructive, productive and destructive-productive forms of osteomyelitis of the jaw. Destructive osteomyelitis is marked by deformed alveolar process of maxillary, ulterior fold of mucous tunic, and mucous tunic with some congestion. In the nidus of inflammatory process the teeth are loose, and the affected tooth is, as a rule, extracted. There are one or some purulent fistulas, and in case of sequestrum - granulations flow from it. 5 X-ray investigation. The roentgenogram shows irregular destruction of the bone tissue and sequestra. Sequestra on the upper jaw are formed during 3-4 weeks, while the sequestra on the lower jaw – during 5-6 weeks since the onset of the disease. Productive form of the osteomyelitis is marked by the deformity of face owing to the intumescence/ thickening of the alveolar process of the maxillary from two sides; mucous tunic is cyanotic in this zone. Fistulas usually don’t form. The roentgenogram shows thickening of the jaw due to the periosteal apposition and bone tissue induration (uniform or mediate). Destructive-productive form of the chronic osteomyelitis combines the characteristics of the above Scheme of sequester formation mentioned two forms. at different areas of mandible Treatment. 1. Extraction of the affected tooth, in case, if it hasn’t been extracted at the stage of acute osteomyelitis. 2. Sequestrectomy (in case of destructive form of the osteomyelitis). 3. The productive form of osteomyelitis is treated with levomizol (locally) and in the farther treatment - leveling procedure of the bone is required. 4. General medical treatment (antibiotics, sulfonamides, immune therapy). ACUTE ODONTOGENIC MAXILLARY SINUSITIS. That is acute inflammatory process of maxillary sinus mucous tunic as a result of odontogenic cause (affected tooth). Patient complains of pain in the upper jaw, which becomes more severe when bending the head, sensation of heaviness in one part of the face, and blocking of nose from one side, weakening of olfaction, some discharge from one nostril. Clinical picture. The main symptoms of the disease are general weakness, sleep and appetite disturbance, high body temperature, intoxication. The smoothed out nasolabial fold from one side of the face and minor soft-tissue edema are determined while examining the patient. Pressing on the front part of the maxillary sinus causes painful sensation. The phenomena of periodontitis (mostly 16, 17, 26 and 27 teeth), alveolitis, periostitis, osteomyelitis, as well as the anastomosis of the oral cavity and maxillary sinus, which emerged after extraction of the tooth, the roots of which were situated in the maxillary sinus, can be observed on the maxillary from the side of the inflammation process. The axial section roentgenogram shows covering of the maxillary sinus of different degrees. Upper-medial cupola of the maxillary sinus can be covered less than its other parts as distinct from the rhinogenous maxillary sinusitis. X-ray investigation. The enlargement X-ray film of the upper jaw teeth shows depressioin of the bone tissue around the molar teeth roots, and close position of the tooth roots, with regard to the lower part of the maxillary sinus. Treatment. 1. Treatment or extraction of the affected tooth. 2. Maxillary sinusotomy at the pushing of the tooth root or instrument. 3. Removal of the anastomosis and draining of the maxillary sinus through nasal meatus in case of maxillary sinusitis; in case of the opening of the intact maxillary sinus - prescription of the vasoconstrictive medication. 4. General medical treatment (antibiotics, sulfonamides). CHRONIC ODONTOGENIC MAXILLARY SINUSITIS. 6 Patient complains of the slight headache, purulent discharge from one of the nostrils. There is minor deterioration of the general condition. Clinical picture. Face remains symmetric, mucous tunic of the alveolar process of the maxilla from the side of inflammation is slightly cyanotic. Periodontitis is characteristic of affected tooth; percussing is slightly painful. In case of the proceeding extraction of the tooth the outflow of the inflammatory exudates can be observed there. It is possible to determine the perforation by means of the following actions: it is necessary to open the mouth and close the nose of the patient, and, bringing a piece of the cotton wool to the specified anastomosis, ask the patient to breathe out through the nose. In case of perforation the fibres of the cotton wool will vacillate. In case of the anastomosis obturation and accumulation of the exudate in the maxillary sinus there is a possibility of the inflammation. X-ray investigation. The axial section roentgenogram film may show darkened maxillary sinus; the kinds of shadows may serve as an evidence of the fact, that the maxillary sinus is covered by the thickened mucous tunic, the borders of it are vividly expressed. It is necessary to remember that in case of the odontogenic maxillary sinusitis the X-ray will show the unchanged upper-medial cupola. Treatment. 1. Treatment or extraction of the affected tooth. 2. Maxillary sinusotomy in case of oro-antrel anastomosis and hypertrophically changed mucous tunic of the maxillary sinus. 3. General medical treatment (antibiotics, sulfonamides, immune therapy). ACUTE ODONTOGENIC AND NONODONTOGENIC LYMPHADENITIS. Patient complains of the tumor-like mass, which occurs as a rule in the perimaxillary zone as a result of the affected tooth disease or other inflammatory processes. Clinical picture. The superficial lymphadenitis (submaxillary, mental and others) are marked by the deformity of the corresponding facial region, owing to the enlarged, painful, and sometimes limited in its mobility lymph node. In case of the serous lymphadenitis the colour of the skin over the affected lymph node is not changed. Purulent lymphadenitis is marked by hyperemic skin, the tissues around are infiltrated. Deep lymphadenitis (of parotid-masticatory, buccal region or neck) is marked by the minor soft-tissue deformity, pain syndrome and impaired function prevail. Minor infiltration of the tissues over the affected lymph node, painful palpation, dysfunction (e.g. opening of the mouth in case of localization of the process in the parotidmasticatory region) are characteristic features of the purulent lymphadenitis. Both serous and purulent lymphadenitis diseases in the affected tooth are marked by the acute periodontitis or chronic periodontitis at the stage of exacerbation. Treatment. 1.Treatment or extraction of the affected tooth. 2. Medical treatment (antibiotics, sulfonamides). 3. Drain of the abscess in case of purulent lymphadenitis. ABSCESSES AND PHLEGMONS OF THE MAXILLOFACIAL REGION. Abscess is a acute limited inflammatory process, while phlegmon is a generalized suppurative acute inflammatory process of the soft tissues (of the subcutaneous fat mostly). Patient complains of the painless, limited (abscess) or generalized (phlegmon) inflammatory process of the soft tissues region. Depending on the localization (superficial or deep process) the patient may complain of the complicated opening of the mouth, chewing, swallowing and bad breathing. The characteristic features of the disease are intoxication phenomena – high body temperature, headache, refusal to eat, paleness of the cutaneous covering, sleep disturbances. These symptoms are more marked in case of phlegmons, especially deep and anaerobic phlegmons. Clinical picture. Superficial abscesses and phlegmons (submaxillary, malar, submentum and 7 buccal region) are marked by the edema and deformity of the soft tissues of the corresponding zone, hyperemia of skin over the nidus of inflammation, dense, painful during palpation infiltration and fluctuation in most of the cases. In case of localization of the inflammatory process in the parotid-masticatory, buccal or retromandibular region opening of the mouth, caused by the trismus and pain in the nidus of infection, may be complicated. In cases of deep abscesses and phlegmons (retrobulbar space, temporal fossa, infratemporal fossa, palatopterygoid fossa, sphenoid maxillary space, mouth floor, peripharyngeal space) it is the function that is deteriorated most, and the external manifestation (edema of the soft tissues, infiltrate, and fluctuation) are not vividly marked. So, in case of localization of the inflammatory process in the region of the infratemporal fossa, the opening of the mouth is complicated; in case of the localization in the mandibulohyoid valley – mouth opening and then painful swallowing; in the peripharyngeal space - sharp pain when swallowing; in the region of the mouth Possible locations of temporal abscesses floor – swallowing, breath; in the retrobulbar space region - visual impairment, limited mobility of the eyeball, chemosis, exophthalmos. In case of the anaerobic phlegmon of the mouth floor (Ludwig's angina) the clinical course is of major importance. Anaerobic infection is marked by crepitation symptom (gases are accumulated in the subcutaneous fat and are cracking during palpation, resembling the creak of snow); necrotic mass is determined during draining of the nidus; muscles achieve the colour of the boiled meat; foul, grey substance is exuded, there is no pus. In case of the abscess or phlegmons of the odontogenic origin in the affected tooth – acute periodontitis or exacerbation of the chronic periodontitis, cavity or filling. Localization of inflammatory process in the region of the mouth floor 8 Localization of abscess within the mouth floor Treatment. 1. Drain of abscesses and phlegmons (under general anaesthetic) taking into consideration their localization, spreading of the n.facialis bacillus, natural folds of face, neck and creating of the favourable conditions for exudate outflow. 2. Draining of the inflammatory nidus. 3. In case of odontogenic origin of the disease – extraction of the affected tooth. 4. Bacterial examination for determining of the microflora antibiotic susceptibility. 5. General medical treatment. There is necessity to prescribe the antibiotics after correct lancing and draining of the nidus of inflammation. In case of the Ludwig’s angina: 1. Drain of the abscesses, phlegmons, infiltrates by means of section in the submaxillary, retromandibular, submental regions, joined by means of the perforated tube drainage. 2. Creating of the highest possible conditions for aeration of the wound, its dialysis with antiseptic liquid and oxidizing substances. 3. Prevention of the joining of the commonplace microflora. 4. Immune therapy. 9 Common incision sites Lymph nodes and drain directions 10