* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Anatomy of
Survey
Document related concepts
Vascular remodelling in the embryo wikipedia , lookup
Anatomical terms of location wikipedia , lookup
Lymphatic system wikipedia , lookup
Human digestive system wikipedia , lookup
Anatomical terminology wikipedia , lookup
History of anatomy wikipedia , lookup
Transcript
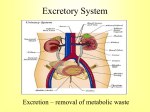
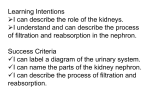
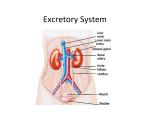
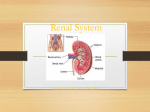
Clinically Oriented Anatomy of Retroperitoneum, Kidneys and Adrenals Associate Professor Dr. Alexey Podcheko Spring 2015 Learning Objectives To know anatomy and clinical aspects of of 1. Retroperitoneal space 2. Kidneys 3. Adrenal glands Retroperitoneal Structures The retroperitoneal space (retroperitoneum): anatomical space behind the peritoneum. There is no clear delineating anatomical structures Organs having peritoneum on their anterior side are referred to be retroperitoneal Retroperitoneal Structures not suspended by mesentery retroperitoneum is subdivided into the following spaces: 1. Perirenal space 2. Anterior pararenal space - includes duodenum, pancreas, and ascending & transverse colon 3. Posterior pararenal space - includes iliopsoas muscle, ureter, and branches of IVC and their lymphatics Anterior pararenal Posterior pararenal space Retroperitoneal Structures Primarily retroperitoneal: Adrenal gland Kidneys & ureters Bladder Aorta & inferior vena cava Rectum (lower third) Secondarily retroperitoneal: •Parts of the duodenum •Pancreas (except the tail) •Ascending & Descending Colon Retroperitoneal Structures A useful mnemonic to aid recollection of the abdominal retroperitoneal viscera is SAD PUCKER, or DUKE CRAPS: S = Suprarenal glands (aka the adrenal glands) A = Aorta/IVC D = Duodenum (2nd & 3rd segments [may be the 4th segment]) P = Pancreas (only head, neck, and body are retroperitoneal) U = Ureters C = Colon (ascending & descending colons: the transverse & sigmoid retain mesocolon) K = Kidneys E = Esophagus R = Rectum KIDNEYS •The kidneys produce urine that is conveyed by the ureters to the urinary bladder in the pelvis •The superomedial aspect of each kidney normally contacts a suprarenal gland enclosed in a fibrous capsule and a cushion of pararenal fat •A weak fascial septum separates the suprarenal glands from the kidneys so that they are not actually attached to each other •The suprarenal glands function as part of the endocrine system, completely separate in function from the kidneys. Perinephric fat •Perinephric fat (the perirenal fat capsule) surrounds the kidneys and their vessels as it extends into their hollow centers, the renal sinuses. Renal Fascia The kidneys, suprarenal glands, and the perinephric fat surrounding them are enclosed (except inferiorly) by a condensed, membranous layer of renal fascia, which continues medially to ensheath the renal vessels, blending with the vascular sheaths of the latter. Renal Fascia, contd. •Inferomedially, a delicate extension of the renal fascia is prolonged along the ureter as the periureteric fascia •External to the renal fascia is paranephric fat (or the pararenal fat body), the extraperitoneal fat of the lumbar region that is most obvious posterior to the kidney •The renal fascia sends collagen bundles through the paranephric fat. Renal Fascia, contd. •The collagen bundles, renal fascia, and perinephric and paranephric fat, along with the binding provided by the renal vessels and ureter, hold the kidneys in a relatively fixed position (T12-L3) •However, movement of the kidneys occurs during respiration and when changing from the supine to the erect position, and vice versa. Renal Fascia, contd. •Superiorly, the renal fascia is continuous with the fascia on the inferior surface of the diaphragm (diaphragmatic fascia); thus the primary attachment of the suprarenal glands is to the diaphragm. •Inferiorly, the anterior and posterior layers of renal fascia are only loosely united. Perinephric Abscess •The attachments of the renal fascia determine the path of extension of a . perinephric abscess – pus in the perinephric fat •Fascia at the renal hilum attaches to the renal vessels and ureter, usually preventing the spread of pus to the contralateral side •Pus from an abscess (or blood from an injured kidney) may force its way into the pelvis between the loosely attached anterior and posterior layers of the pelvic fascia. Nephroptosis •Because the layers of renal fascia do not fuse firmly inferiorly to offer resistance, abnormally mobile kidneys may descend more than the normal 3 cm when the body is erect. •When kidneys descend, the suprarenal glands remain in place because they lie in a separate fascial compartment and are firmly attached to the diaphragm. Nephroptosis, contd. •Nephroptosis (dropped kidney) is distinguished from an ectopic kidney (congenital misplaced kidney) by a ureter of normal length that has loose coiling or kinks because the distance to the bladder has been reduced. Symptoms of intermittent pain in the renal region, relieved by lying down, appear to result from traction on the renal vessels. Kidneys Anatomy 1 •The ovoid kidneys remove excess water, salts, and wastes of protein metabolism from the blood while returning nutrients and chemicals to the blood. •They lie retroperitoneally on the posterior abdominal wall, one on each side of the vertebral column at the level of the T12 - L3 vertebrae. L: Liver, P: Pancreas, LS: Lesser sac, S: Spleen, C: Colon, V: Inferior vena cava, A: Abdominal aorta, D: Duodenum, RK: Right kidney, LK: Left kidney Kidneys Anatomy 2 •The right kidney usually lies slightly inferior to the left kidney, probably owing to its relationship to the liver. • During life, the kidneys are reddish brown and measure approximately 10 cm in length, 5 cm in width, and 2.5 cm in thickness. Kidneys Anatomy 3 Superiorly, the kidneys are associated with the diaphragm, which separates them from the pleural cavities and the 12th ribs. More inferiorly, the posterior surfaces of the kidney are related to the quadratus lumborum muscle. 12th rib Kidneys Anatomy 4 •The subcostal nerve and vessels and the iliohypogastric and ilioinguinal nerves descend diagonally across the posterior surfaces of the kidneys. 12th rib Kidneys Anatomy 5 The liver, duodenum, and ascending colon are anterior to the right kidney. The right kidney is separated from the liver by the hepatorenal recess. The left kidney is related to the stomach, spleen, pancreas, jejunum, and descending colon. Kidneys Anatomy: Hilum •At the concave medial margin of each kidney is a vertical cleft, the renal hilum, where the renal artery enters and the renal vein and renal pelvis leave the renal sinus. •At the hilum, the renal vein is anterior to the renal artery, which is anterior to the renal pelvis. Kidneys Anatomy: Sinus The renal hilum is the entrance to a space within the kidney, the renal sinus, which is occupied by the renal pelvis, calices, vessels, and nerves and a variable amount of fat. Kidneys Anatomy: Poles, Margins, Surfaces Each kidney has anterior and posterior surfaces, medial and lateral margins, and superior and inferior poles. Kidneys Anatomy: Position However, because of the protrusion of the lumbar vertebral column into the abdominal cavity, the kidneys are obliquely placed, lying at an angle to each other. Kidneys Anatomy: Renal Pelvis The lateral margin of each kidney is convex, and the medial margin is concave where the renal sinus and renal pelvis are located. The indented medial margin gives the kidney a somewhat bean-shaped appearance. The renal pelvis is the flattened, funnel-shaped expansion of the superior end of the ureter. The apex of the renal pelvis is continuous with the ureter. Kidneys Anatomy: Calyces and Papillas The renal pelvis receives two or three major calices (calyces), each of which divides into two or three minor calices. Each minor calyx is indented by the renal papilla, the apex of the renal pyramid, from which the urine is excreted. Kidneys Anatomy: Pyramides In living persons, the renal pelvis and its calices are usually collapsed (empty). The pyramids and their associated cortex form the lobes of the kidney. The lobes are visible on the external surfaces of the kidneys in fetuses, and evidence of the lobes may persist for some time after birth. Renal Transplantation Renal transplantation is now an established operation for the treatment of selected cases of chronic renal failure. The kidney can be removed from the donor without damaging the suprarenal gland because of the weak septum of renal fascia that separates the kidney from this gland. The site for transplanting a kidney is in the iliac fossa of the greater pelvis. This site supports the transplanted kidney, so that traction is not placed on the surgically anastomosed vessels. The renal artery and vein are joined to the external iliac artery and vein, respectively, and the ureter is sutured into the urinary bladder. Renal Cysts Cysts in the kidney, multiple or solitary, are common findings during ultrasound examinations and dissection of cadavers. Adult polycystic disease of the kidneys is an important cause of renal failure; it is inherited as an autosomal dominant trait. The kidneys are markedly enlarged and distorted by cysts as large as 5 cm. Ureters •The ureters are muscular ducts (25 30 cm long) with narrow lumina that carry urine from the kidneys to the urinary bladder. •They run inferiorly from the apex of the renal pelves at the hila of the kidneys, passing over the pelvic brim at the bifurcation of the common iliac arteries. •They then run along the lateral wall of the pelvis and enter the urinary bladder. •The abdominal parts of the ureters adhere closely to the parietal peritoneum and are retroperitoneal throughout their course Ureters: Constricted Areas The ureters are normally constricted to a variable degree in three places: (1) at the junction of the ureters and renal pelves, (2) where the ureters cross the brim of the pelvic inlet, and (3) during their passage through the wall of the urinary bladder. These constricted areas are potential sites of obstruction by ureteric (kidney) stones. Ureters: Blood Supply •Abdominal portion of the ureter -renal arteries, testicular, ovarian arteries, the abdominal aorta, and the common iliac arteries. •The branches approach the ureters medially and divide into ascending and descending branches, forming a longitudinal anastomosis on the ureteric wall. •Branches are small and relatively delicate, and disruption may lead to ischemia in spite of the continuous anastomotic channel formed •In operations in the posterior abdominal region, surgeons pay special attention to the location of ureters and are careful not to retract them laterally or unnecessarily. Ureters: Blood Supply Veins draining the abdominal part of the ureters drain into the renal and gonadal (testicular or ovarian) veins. Ureters: Lymphatic Drainage •The lymphatic vessels of the ureters join the renal collecting vessels or pass directly to right or left lumbar (caval or aortic) lymph nodes and the common iliac lymph nodes. •Lymph drainage from the pelvic parts of the ureters is into the common, external, and internal iliac lymph nodes. Renal Arteries and Veins •The renal arteries arise at the level of the intervertebral disc between the L1 and the L2 vertebrae. •The longer right renal artery passes posterior to the inferior vena cava. Renal Arteries and Veins Typically, each artery divides close to the hilum into five segmental arteries that are end arteries (i.e., they do not anastomose significantly with other segmental arteries, so that the area supplied by each segmental artery is an independent, surgically resectable unit or renal segment). Vascular Supply Renal artery Interlobar arteries Arcuate arteries Interlobular arteries Afferent arteries Glomeruli Efferent arterioles Peritubular plexus Arcuate veins Renal Veins •Several renal veins drain each kidney and unite in a variable fashion to form the right and left renal veins. •The right and left renal veins lie anterior to the right and left renal arteries. Renal Veins •The longer left renal vein receives the left suprarenal vein, the left gonadal (testicular or ovarian) vein, and a communication with the ascending lumbar vein, then passes anterior to the aorta. •Each renal vein drains into the inferior vena cava. Ascending lumbar vein Accessory Renal Vessels •During their ascent to their final site, the embryonic kidneys receive their blood supply and venous drainage from successively more superior vessels. •Usually the inferior vessels degenerate as superior ones take over the blood supply and venous drainage. Accessory Renal Vessels •Failure of these vessels to degenerate results in accessory renal arteries and veins (known as polar arteries and veins when they enter/exit the poles of the kidneys). •Variations in the number and position of these vessels occur in approximately 25% of people. Congenital Anomalies of the Kidneys and Ureters •Bifid renal pelvis and ureter are fairly common. These anomalies result from division of the metanephric diverticulum (ureteric bud), the primordium of the renal pelvis and ureter. Congenital Anomalies of the Kidneys and Ureters •The extent of ureteral duplication depends on the completeness of embryonic division of the metanephric diverticulum. •The bifid renal pelvis and/or . ureter may be unilateral or bilateral; however, separate openings into the bladder are uncommon. •Incomplete division of the metanephric diverticulum results in a bifid ureter; complete division results in a supernumerary kidney Congenital Anomalies of the Kidneys and Ureters •An uncommon anomaly is a retrocaval ureter, which leaves the kidney and passes posterior to the inferior vena cava. Congenital Anomalies of the Kidneys and Ureters •The embryonic kidneys are close together in the pelvis. •In approximately 1 in 600 fetuses, the inferior poles (rarely, the superior poles) of the kidneys fuse to form a horseshoe kidney. •This U-shaped kidney usually lies at the level of L3 - L5 vertebrae because the root of the inferior mesenteric artery prevented normal ascent of the abnormal kidney. •Horseshoe kidney usually produces no symptoms; however, associated abnormalities of the kidney and renal pelvis may be present, obstructing the ureter. Congenital Anomalies of the Kidneys and Ureters •Sometimes the embryonic kidney on one or both sides fails to ascend to the abdomen and lies anterior to the sacrum. •Although uncommon, awareness of the possibility of an ectopic pelvic kidney should prevent it from being mistaken for a pelvic tumor and removed. •A pelvic kidney in a woman also can be injured by or cause obstruction during childbirth. •Pelvic kidneys usually receive their blood supply from the common iliac arteries. Renal and Ureteric Calculi •Calculi are composed of salts of inorganic or organic acids or of other materials. •They may form and become located in the calices of the kidneys, ureters, or urinary bladder. •A renal calculus (kidney stone) may pass from the kidney into the renal pelvis and then into the ureter. Renal and Ureteric Calculi •If the stone is sharp, or it is larger than the normal lumen of the ureter (approximately 3 mm) causing excessive distension of this muscular tube, the ureteric calculus will cause severe intermittent pain (ureteric colic) as it is gradually forced down the ureter by waves of contraction. •The calculus may cause complete or intermittent obstruction of urinary flow. Renal and Ureteric Calculi •Depending on the level of obstruction, which changes, the pain may be referred to the lumbar or inguinal regions, or the external genitalia and/or testis. •The pain is referred to the cutaneous areas innervated by spinal cord segments and sensory ganglia, which also receive visceral afferents from the ureter, mainly T11 - L2. •The pain passes inferoanteriorly from the loin to the groin as the stone progresses through the ureter (the loin is the lumbar region, and the groin is the inguinal region). •The pain may extend into the proximal anterior aspect of the thigh by projection through the genitofemoral nerve (L1, L2), the scrotum in males and the labia majora in females. •The extreme pain may be accompanied by marked alimentary upset (nausea, vomiting, cramping, and diarrhea) and a generalized sympathetic response that may to various degrees mask the more specific symptoms. Suprarenal Glands •The suprarenal (adrenal) glands, yellowish in living persons, are located between the superomedial aspects of the kidneys and the diaphragm, where they are surrounded by connective tissue containing considerable perinephric fat. Suprarenal Glands •The glands are enclosed by renal fascia by which they are attached to the crura of the diaphragm. •They are separated from the kidneys by a thin septum (part of the renal fascia). Suprarenal Glands: shape and relations •differ on the two sides •The pyramidal right gland is more apical (situated over the superior pole) relative to the right kidney, lies anterolateral to the right crus of the diaphragm, and makes contact with the inferior vena cava anteromedially and the liver anterolaterally. Suprarenal Glands: shape and relations •The crescent-shaped left gland is medial to the superior half of the left kidney and is related to the spleen, stomach, pancreas, and the left crus of the diaphragm. Suprarenal Glands: Size and Hilum •Each gland has a hilum, where the veins and lymphatic vessels exit the gland; whereas arteries and nerves enter the glands at multiple sites. •The medial borders of the suprarenal glands are 4 - 5 cm apart. Suprarenal Glands: •Each suprarenal gland has two parts: the suprarenal cortex and suprarenal medulla; these parts have different embryological origins and different functions. Parts Suprarenal Glands: Cortex •The suprarenal cortex derives from mesoderm and secretes corticosteroids and androgens. •These hormones cause the kidneys to retain sodium and water in response to stress, increasing the blood volume and blood pressure. •They also affect muscles and organs such as the heart and lungs. Suprarenal Glands: Medulla •The suprarenal medulla is a mass of nervous tissue permeated with capillaries and sinusoids that derives from neural crest cells associated with the sympathetic nervous system. •The chromaffin cells of the medulla are related to sympathetic ganglion (postsynaptic) neurons in both derivation (neural crest cells) and function. •These cells secrete catecholamines (mostly epinephrine) into the bloodstream in response to signals from presynaptic neurons. •The powerful medullary hormones epinephrine (adrenaline) and norepinephrine (noradrenaline) activate the body to a flight-or-fight status in response to traumatic stress. •They also increase heart rate and blood pressure, dilate the bronchioles, and change blood flow patterns, preparing for physical exertion. Suprarenal Glands: Blood Supply •The endocrine function of the suprarenal glands makes their abundant blood supply necessary. •The suprarenal arteries branch freely before entering each gland so that 50 - 60 arteries penetrate the capsule covering the entire surface of the glands. Suprarenal Glands: Blood Supply - Suprarenal arteries •Suprarenal arteries arise from three sources: 1. Superior suprarenal arteries from the inferior phrenic arteries. 2. Middle suprarenal arteries from the abdominal aorta near the level of origin of the superior mesenteric artery. 3. Inferior suprarenal arteries from the renal arteries Suprarenal Glands: •The venous drainage of the suprarenal gland is into a large suprarenal vein. •The short right suprarenal vein drains into the inferior vena cava, whereas the longer left suprarenal vein, often joined by the inferior phrenic vein, empties into the left renal vein. Blood Supply - Veins