* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
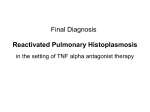
Download Presentation on Histoplasmosis
Hepatitis C wikipedia , lookup
Sarcocystis wikipedia , lookup
Oesophagostomum wikipedia , lookup
Trichinosis wikipedia , lookup
Meningococcal disease wikipedia , lookup
Hepatitis B wikipedia , lookup
Onchocerciasis wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Chagas disease wikipedia , lookup
Leishmaniasis wikipedia , lookup
Visceral leishmaniasis wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Schistosomiasis wikipedia , lookup
Leptospirosis wikipedia , lookup
www.AssignmentPoint.com Histoplasmosis is a disease, usually affecting the lungs, caused by the Histoplasma capsulatum fungus. Although many people that are or have been infected with H. capsulatum do not appear ill, some people in the acute phase of the disease have a dry cough, fever, and chest pains and do feel ill. There are several types of histoplasmosis (acute, chronic, and disseminated, all with subtypes). H. capsulatum was first described by Samuel Darling in 1906 within human tissue cells (histiocytes). In 1932, Katharine Dodd and Edna Tompkins made the first diagnosis of histoplasmosis in an infant. www.AssignmentPoint.com Types of histoplasmosis: Histoplasmosis has three major types of disease, and these three have other subtypes included in them. They are summarized with their subtypes as follows: acute pulmonary histoplasmosis; asymptomatic and symptomatic; chronic pulmonary histoplasmosis; chronic lung symptoms and occasionally ocular involvement termed ocular histoplasmosis syndrome; and progressive disseminated histoplasmosis: chronic progressive disseminated histoplasmosis with oropharyngeal lesions or ulcers; subacute progressive disseminated histoplasmosis with intestinal, adrenal, cardiac or central nervous system (CNS) involvement; and acute progressive disseminated histoplasmosis with encephalopathy, meningitis, mass lesions and cutaneous (skin) lesions. www.AssignmentPoint.com Causes of histoplasmosis: Histoplasmosis is caused by a dimorphic (two forms, mycelia and yeast) fungus named Histoplasma capsulatum. The genus name is misleading; the fungus has no capsule, but early investigators mistakenly thought it did. The mycelial phase consisting of mycelia fragments and spores can be inhaled and may reach the lung alveoli. Macrophages (human phagocytic cells of the immune system) surround and engulf (phagocytosis) H. capsulatum, which then changes inside the macrophages to the yeast form in about 15-18 hours. In most cases, the macrophage response kills the yeast. When macrophages fail to kill all the yeast, a variation of the disease develops because the yeast form multiplies and invades other cells. The larger the number of mycelia and spores the person is exposed to, the more likely the person will develop symptomatic disease. www.AssignmentPoint.com Symptoms and signs of histoplasmosis: About 90% of infections caused by H. capsulatum are asymptomatic (produce no symptoms). Occasionally, a few asymptomatic patients will show small scars in lung X-rays. Symptomatic people often develop fever, chills, dry cough, malaise, sweats, and abdominal pains about three to 14 days after exposure. If the disease progresses, symptoms such as weight loss, fatigue, dyspnea, chest pain, and reduced or loss of vision may occur. A sign of progression are patchy infiltrates seen on chest X-rays, usually in the lower lung fields. Other symptoms that can occur, especially in patients that are immunosuppressed, are mouth ulcers, fevers, headaches, confusion, seizures, encephalopathy, and infrequently, death. www.AssignmentPoint.com www.AssignmentPoint.com Treatment of histoplasmosis: For asymptomatic people or people with acute localized infection who are otherwise healthy, antifungal treatment is usually not recommended as these people have or will resolve the infection in about three weeks. If symptoms persist a month or more, itraconazole (Sporanox), ketoconazole (Nizoral) or amphotericin B (Fungizone, Amphocin) may be effective. If CNS involvement occurs, or if the person is compromised by other diseases or is immunocompromised and has severe histoplasmosis (progressive disseminated histoplasmosis), either itraconazole or amphotericin B is recommended. The lengths of time, dosing amounts, and dosing routes are usually individualized for the patient; consultations with both infectious disease and pulmonary specialists are recommended. Other new azoles compound drugs may be effective in some difficult or unresponsive cases; the consultants could help select the appropriate new drug treatment. www.AssignmentPoint.com Prevention of histoplasmosis: People living in endemic areas like the Ohio River Valley are likely to be exposed to histoplasmosis no matter what they do, since the fungus is likely in the dust in the air. However, if they are healthy, most people that get exposed or infected with H. capsulatum will be asymptomatic. Immunosuppressed (those with HIV or cancer or who are receiving chemotherapy for cancer) might reduce their chances of exposure if they live in endemic areas by avoiding high dust areas like construction sites. Soil can be decontaminated with 3% formalin under special circumstances. www.AssignmentPoint.com www.AssignmentPoint.com