* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Oral ulcerations
Childhood immunizations in the United States wikipedia , lookup
Ulcerative colitis wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Periodontal disease wikipedia , lookup
Schistosomiasis wikipedia , lookup
IgA nephropathy wikipedia , lookup
Rheumatoid arthritis wikipedia , lookup
Autoimmune encephalitis wikipedia , lookup
Onchocerciasis wikipedia , lookup
Kawasaki disease wikipedia , lookup
Globalization and disease wikipedia , lookup
Ankylosing spondylitis wikipedia , lookup
Germ theory of disease wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Inflammatory bowel disease wikipedia , lookup
Multiple sclerosis signs and symptoms wikipedia , lookup
Sjögren syndrome wikipedia , lookup
Neuromyelitis optica wikipedia , lookup
Pathophysiology of multiple sclerosis wikipedia , lookup
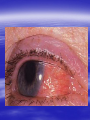
Oral ulcerations Prof. Elsanousi M Taher BDS, MSc., FFDRCSI Email: [email protected] “ an ulcer is break in the continuity or loss of integrity of skin or mucous membrane” “ an erosion is superficial and partial loss of epithelium” Classifications of oral ulcers On etiology: Traumatic Infective Neoplastic Dermatological Hematological Nutritional Immunological Cytotoxic drug related Classifications of oral ulcers On initial presentation: Primary ulcer: arise “du novo”: Trauma Dematoses Neoplastic Secondary ulcer: Preceded by vesicle or bullae: Viral infections Some dermatoses Angina bullosa hemorrhgica Traumatic ulcers Mechanical: – Of acute nature Physical: e.g. radiation Traumatic ulcers Chemical: – Aspirin burn after sloughing – Phenol (carbolic acid) used as a disinfectant – Silver nitrate that used as cauterizing agent – Trichloroacetic acid used as a stringent for gingival retraction – Excessive use of mouth wash Traumatic ulcers Traumatic ulcer may mimic neoplastic ulcer Traumatic ulcer due to use of tooth paste containing formaldehyde Management of traumatic ulcers: – Treat the cause – Symptomatic treatment – Should heal within a week other wise rethink !! – May need biopsy Infective ulcers Bacterial: Viral: Fungal: Tuberculous ulcer Neoplastic ulcers Features: – painless at early stages – single – long duration – indurated – rolled and everted edge – may be associated with palpable lymph node Neoplastic ulcers The neoplastic ulcers may be seen in: SCC BCC Melanoma Salivary gland tumor Lymphoma Dermatological ulcers: LP LE DH Linear IgA disease Linear IgA disease Variant of DH but not associated with Gluten Non specific oral ulcers Skin lesions Diagnosed by linear deposition of IgA along the BMZ in DIF sections Linear IgA disease Treatment: Dapsone Steroids Sulfones Nutritional ulcers See anemia Cytotoxic drugs related ulcers The drug cause: suppression of the immune system depression of bone marrow some other drugs may also cause anemia like phenytoin Recurrent aphthous ulceration or stomatitis The most common type of non traumatic ulcers of the mouth Affects 15-20% of the population May start in childhood but usually on teens and early twenties Affect both sexes RAU may be associated with systemic disease like: – – – – GIT Behçet disease HIV Cyclic neutropenia Etiology Of RAS Unknown but may be associated or related to: – Hereditary and genetic predisposition: Seen in children of affected parents familial tendencies (1/3 of patients) Associated with certain HLA groups – Traumatic: precipitating factor and not a causative – Hormonal: occurs at premenstrual days improved during pregnancy Etiology Of RAS GIT disorders: celiac and Crohn’s diseases other malnutrition conditions Psychosomatic: H/O stress affect stressful professional people students during exams Etiology Of RAS Hypersensitivity: – some times it is associated with atopy & food allergy Microbial: Hypersensitivity reactions to S. sanguis & L. forms Cross reactions of oral mucosa with S. sanguis Viral etiology ( adenoviruses) Etiology Of RAS Nutritional: – Iron, folate, vit. B12 deficiency were found in 5-10 % of patients – Association with celiac disease, DC & UC Etiology Of RAS Immunological: – Evidences are conflicting and not consistent – It may be delayed type hypersensitivity reaction – It may be immuncomplex reactions (vasculitis of local type) – It may be due to inherent imbalance of the immune regulation that results in disturbance in the ratio between T4 & T8 Etiology Of RAS “ From different studies, even though some of the evidence has been conflicting, it appears likely that aphthous ulceration results from focal immune dysfunction in which T lymphocytes play a significant role. The nature of the initiating stimulus remains a mystery. The causative agents could be endogenous ( autoimmune) antigen or exogenous (hyperimmune) antigen, or it could be non specific factor such as trauma in which a chemical mediators may be involved Clinically three stages of the ulcers may be seen: II- Pre-ulcerative stage: prodromal symptoms o Lasts for 18-72 hrs o Paraesthesia o Red macule II- Ulcerative stage: o Gray round to oval white primary ulcers surrounded by erythematous hallo III- Resolution stage: o Less pain o Epithelial regeneration Aphthous ulcers are primary ulcers on clinical bases they are classified into: minor type (80%): less than 1 cm & heal without scar, are round, shallow that persist for 10-14 days major type (10%): more than 1 cm, lip & soft palate, patient is rarely ulcer free, heal with scar, interfere with eating and speech herpetiform (10%) type: recurrent crops of dozens of ulcers that coalesce together, may resond to 2% tetracycline moutwash Compare between the size of major & minor aphthous ulcers D.D : Recurrent herpes CMV infection in immunocompromised patient Behçet syndrome MMP Pemphigus Trauma Rule out systemic disease: CD, celiac disease Major aphthous ulcer that mimic SCC Investigations: of aphthous ulcers The diagnosis of aphthous ulceration is dependent mainly on proper history & clinical examination It is necessary therefore to enquire about eye, genital, gastrointestinal or skin lesions and fever; some investigations is to be carried out to rule out any systemic cause/s. This is especially important if it appears suddenly on middle aged and above These investigations may include: CBC Serum TIBC Serum Serum Serum iron ferritin B12 folate Investigate for celiac or CD if appropriate Management of RAU 1. Explain to the patient the nature of the disease 2. Current treatment aimed at controlling rather than curing 3. Treatment modalities may include: A. Mouth rinses: A. 0.2% chlorhexidine gluconate B. benzydamine hydrochloride B. Topical steroids: Steroid Dosage Medium potency: Betamethasone phosphate tablets (Betnesol) 0.5 mg ; use as mouth wash High potency: Beclometasone (Beclomethasonedipropionate spray) 1 puff (200 mg) to C. Antimicrobial: tetracycline mouthwash D. Topical LA preparations E. Immunomodulators: a) b) c) d) Lavmisol Cholchicine Dapsone Thalidomide F. Systemic steroids: Management of RAU 4. Local preparations of cyclosporine 5. Soft laser in refractory major aphthae Management of RAU 6. Treat the systemic disease and restore deficiency if present: Thiamine (vit. B12) Pyridoxine (B6) Iron supplements Behçet syndrome It is serious disease because the eye & CNS involvement are quite serious Etiology: unknown but it is associated with HLA B-51 immune dysfunction viral etiology & vasculitis Behçet syndrome Major criteria for diagnosis of Behçet syndrome include: RAS Genital ulcers Ocular lesions CNS lesions Skin lesions Behçet syndrome Minor criteria for diagnosis of Behçet syndrome include: Arthralgia Superficial or deep migratory thrombophlebitis Inflammatory bowel disease Lung disease (pneumonitis) Renal disease: hematuria and Proteinurea Diagnostic criteria (as suggested by the 5th international conference on Behçet disease 1990) 1) Oral ulcerations: – – – aphthous like not explained otherwise persisted for at least 3 times over the last year 2) Any two of the following: – Genital area: recurrent genital ulceration – Eye lesions: retinal vasculitis/ ant. or posterior uveitis and optic neuritis ( eye and CNS are quite serious) Inflammation of the eye, which can involve the front of the eye (uvea) causing uveitis, or the back of the eye (retina) causing retinitis, can lead to blindness. Symptoms of eye inflammation include pain, blurred vision, tearing, redness, and pain when looking at bright lights. It is very important for patients to have this sensitive area monitored by an eye specialist (ophthalmologist). – Skin: erythema nodosum or acniform lesion & positive pathergy test result Behçet syndrome 3) C.T disease, Reiter’s disease, inflammatory bowel disease must be excluded before making diagnosis of Behçet disease 4) Other features considered to be useful in confirming the diagnosis of Behçet disease: – CNS features: similar to MS – Other features: Deep venous thrombosis Subcutaneous thrombophlebitis Epididmitis Arthritis GIT ulcerations & aneurysmal formations Eye lesions in Behçet disease Erythema modosum Behçet syndrome D.D: – Reiter’s syndrome – Sweet syndrome: oral ulcers, conjunctivitis, episcleritis and inflamed tender skin papules or nodules – CT disease – inflammatory bowel disease Investigations: – CBC: leukocytosis, eosinophillia – Raised ESR, raised CRP and acute phase protiens – CNS investigations – GIT to exclude inflammatory bowel disease Behçet syndrome has POOR PROGNOSIS Treatment: Topical steroids Colchicine 0.6 mg bd ( inhibit the effect of leukocyte migration) – Get the approval of FDA in 2009 – it is mainly used for gout Systemic steroids Steroid sparing agents: o Azathioprine o Cyclosporine o Cyclophosphomide o Interferon- Management of eye lesions Reiter's syndrome Etiology: unknown but probably post infection (GUTI) associated with HLA-B27 Features of Reiter's syndrome: young males fever, malaise & weight loss migratory polyarthritis conjunctivitis & uveitis urethral discharge (sterile, non gonococcal urethritis) keratoderma blenorrhagica circinate balanitis aphthous like ulcers geographic tongue like lesions Features of Reiter's syndrome: young males fever, malaise & weight loss migratory polyarthritis conjunctivitis & uveitis urethral discharge (sterile, non gonococcal urethritis) keratoderma blenorrhagica circinate balanitis aphthous like ulcers geographic tongue like lesions • Keratoderma blennorrhagica (or keratoderma blennorrhagicum) are skin lesions commonly found on the palms and soles but which may spread to the scrotum, scalp and trunk also, and which resemble psoriasis. • Keratoderma blennorrhagica is commonly seen as an additional feature of Reiter's syndrome in almost 15% of male patients. • The appearance is usually of a vesico-pustular waxy lesion with a yellow brown colour. These lesions may join together to form larger crusty plaques with desquamating edges. D.D: – Behçet syndrome – GIT inflammatory conditions – Psoriasis : keratotic scaly lesions, arthritis, geographic tongue like lesions( clinically & histopathologically) Treatment: no specific treatment NSAID antibiotics An approach to diagnosing oral ulcers Oral ulceration is probably the commonest oral mucosal disease seen; it may also be the most serious It is important, therefore, to have an approach to the management of oral ulcers firmly established in your mind is the ulcer single or multiple? is it persistent or recurrent? is it primary type or preceded by blister? An approach to diagnosing oral ulcers Where is the site and distribution? Is the size enlarging? Onset? Duration and chronicity? >3 weeks after cause removal do biopsy Pain and bleeding? Aggravating and relieving factors? Any associated phenomenon Examination and describing an ulcer should include – Size – Site (anatomical locations) – Shape – Base – Edge – Induration Examination and describing an ulcer should include – Discharge – fixation – Is it painful? – Lymph drainage – General condition of the patient D.D of ulcers: depends on etiology: consider (TINNDVIM): T traumatic I infective N neoplastic N nutritional D degenerative V vascular I immunological M metabolic GDP have to refer Patients with oral ulcers into OM specialist in: – Patients with ulceration unresponsive to topical therapy; – Suspected Malignancy; – HIV-related ulceration; – Syphilis; – TB; – Drug-related ulceration; – Systemic disease; – Mucocutaneous disorders.